Anesth Pain Med.
2020 Jan;15(1):103-110. 10.17085/apm.2020.15.1.103.
The prevalence and clinical significance of transitional vertebrae: a radiologic investigation using whole spine spiral three-dimensional computed tomographic images
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Jeonbuk National University Medical School, Korea
- 2Research Institute of Clinical Medicine of Jeonbuk National University-Biomedical Research Institute of Jeonbuk National University Hospital, Jeonju, Korea
- KMID: 2500463
- DOI: http://doi.org/10.17085/apm.2020.15.1.103
Abstract
- Background
Errors in counting spinal segments are common during interventional procedures when there are transitional vertebrae. In this study, we investigated the prevalence of the transitional vertebrae including thoracolumbar transitional vertebra (TLTV) and lumbosacral transitional vertebrae (LSTV). The relationship between the existence of TLTV and abnormal rib count or the existence of LSTV were also evaluated.
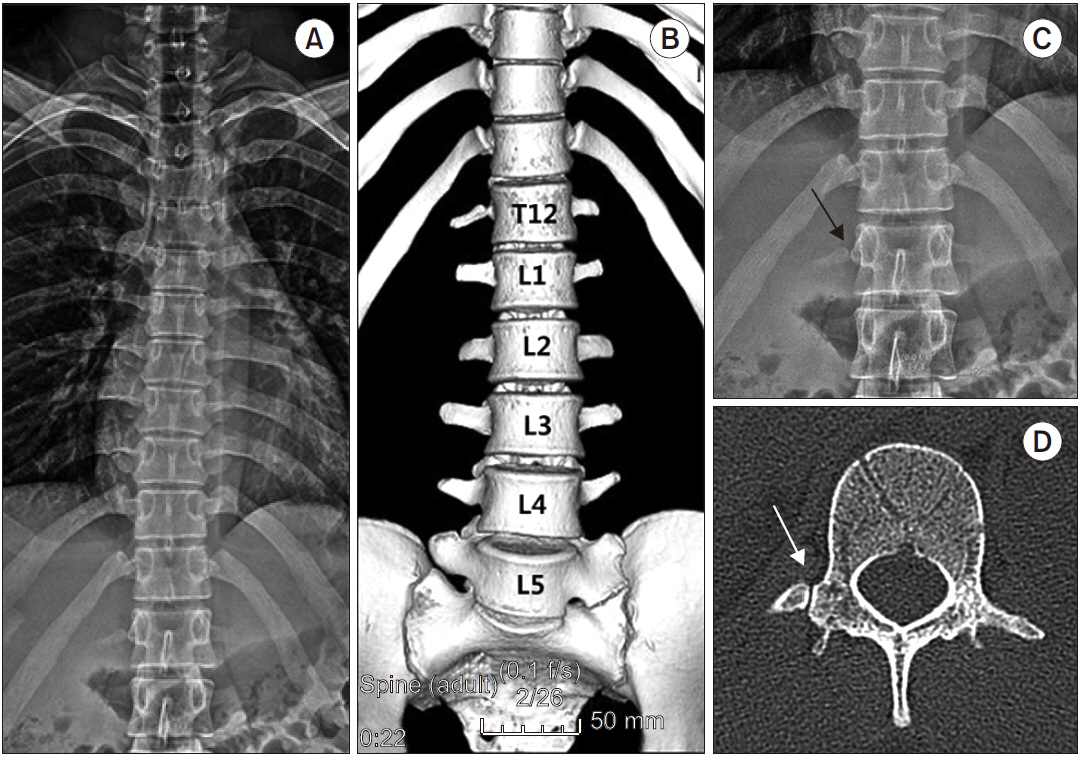
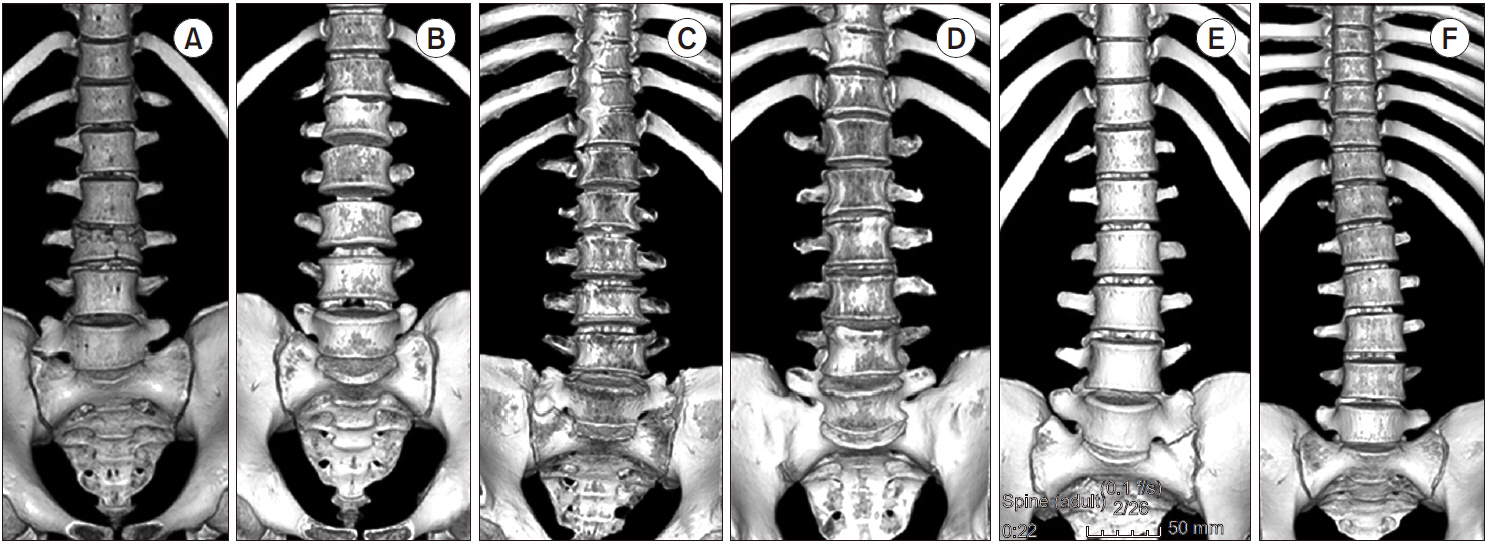
Methods
The vertebral levels were counted craniocaudally, starting from C1, based on the assumption of 7 cervical, 12 thoracic, and 5 lumbar vertebrae, using whole spine spiral three-dimensional computed tomographic images. The 20th and 25th vertebrae were defined as L1 and S1, respectively.
Results
In total, 150 patients had TLTV, with a prevalence of 11.2% (150/1,340). LSTV was observed in 111 of 1,340 cases (8.3%). Sacralization was observed in 68 of 1,340 cases (5.1%) and lumbarization in 43 of 1,340 cases (3.2%). There was a significant relationship between the existence of TLTV and the abnormal rib count (odds ratio [OR]: 117.26, 95% confidence interval [95% CI]: 60.77–226.27; P < 0.001) and LSTV (OR: 7.38, 95% CI: 3.99–13.63; P < 0.001).
Conclusions
Our study results suggest that patients with TLTV are more likely to have an abnormal rib count or LSTV. If a TLTV or LSTV is seen on the fluoroscopic image, a whole spine image is necessary to permit accurate numbering of the lumbar vertebra.
Keyword
Figure
Cited by 1 articles
-
Prediction of successful caudal epidural injection using color Doppler ultrasonography in the paramedian sagittal oblique view of the lumbosacral spine
Seon Woo Yoo, Min-Jong Ki, A Ram Doo, Cheol Jong Woo, Ye Sull Kim, Ji-Seon Son
Korean J Pain. 2021;34(3):339-345. doi: 10.3344/kjp.2021.34.3.339.
Reference
-
Bron JL., van Royen BJ BJ., Wuisman PI. 2007. The clinical significance of lumbosacral transitional anomalies. Acta Orthop Belg. 73:687–95. PMID: 18260478.Nakajima A., Usui A., Hosokai Y., Kawasumi Y., Abiko K., Funayama M, et al. 2014. The prevalence of morphological changes in the thoracolumbar spine on whole-spine computed tomographic images. Insights Imaging. 5:77–83. DOI: 10.1007/s13244-013-0286-0. PMID: 24052419. PMCID: PMC3948909.Castellvi AE., Goldstein LA., Chan DP. 1984. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976). 9:493–5. DOI: 10.1097/00007632-198407000-00014. PMID: 6495013.Akbar JJ., Weiss KL., Saafir MA., Weiss JL. 2010. Rapid MRI detection of vertebral numeric variation. AJR Am J Roentgenol. 195:465–6. DOI: 10.2214/AJR.09.3997. PMID: 20651206.Thawait GK., Chhabra A., Carrino JA. 2012. Spine segmentation and enumeration and normal variants. Radiol Clin North Am. 50:587–98. DOI: 10.1016/j.rcl.2012.04.003. PMID: 22643386.Park SK., Park JG., Kim BS., Huh JD., Kang H. 2016. Thoracolumbar junction: morphologic characteristics, various variants and significance. Br J Radiol. 89:20150784. DOI: 10.1259/bjr.20150784. PMID: 26670155. PMCID: PMC5124870.Lee JH., Lee KJ., Ki M., Kim M., Doo AR., Son JS. 2019. The abnormality of the number of ribs misleading incorrect vertebral segment identification during lumbar intervention: two cases report. Anesth Pain Med. 14:331–4. DOI: 10.17085/apm.2019.14.3.331.Wigh RE. 1980. The thoracolumbar and lumbosacral transitional junctions. Spine (Phila Pa 1976). 5:215–22. DOI: 10.1097/00007632-198005000-00003. PMID: 7394660.Farshad-Amacker NA., Aichmair A., Herzog RJ., Farshad M. 2015. Merits of different anatomical landmarks for correct numbering of the lumbar vertebrae in lumbosacral transitional anomalies. Eur Spine J. 24:600–8. DOI: 10.1007/s00586-014-3573-7. PMID: 25223429.Sekharappa V., Amritanand R., Krishnan V., David KS. 2014. Lumbosacral transition vertebra: prevalence and its significance. Asian Spine J. 8:51–8. DOI: 10.4184/asj.2014.8.1.51. PMID: 24596605. PMCID: PMC3939369.Hahn PY., Strobel JJ., Hahn FJ. 1992. Verification of lumbosacral segments on MR images: identification of transitional vertebrae. Radiology. 182:580–1. DOI: 10.1148/radiology.182.2.1732988. PMID: 1732988.O’Driscoll CM., Irwin A., Saifuddin A. 1996. Variations in morphology of the lumbosacral junction on sagittal MRI: correlation with plain radiography. Skeletal Radiol. 25:225–30. DOI: 10.1007/s002560050069. PMID: 8741056.Mellado JM., Larrosa R., Martín J., Yanguas N., Solanas S., Cozcolluela MR. 2011. MDCT of variations and anomalies of the neural arch and its processes: part 2--articular processes, transverse processes, and high cervical spine. AJR Am J Roentgenol. 197:W114–21. DOI: 10.2214/AJR.10.5811. PMID: 21700971.Tini PG., Wieser C., Zinn WM. 1977. The transitional vertebra of the lumbosacral spine: its radiological classification, incidence, prevalence, and clinical significance. Rheumatol Rehabil. 16:180–5. DOI: 10.1093/rheumatology/16.3.180. PMID: 143714.Newell RLM. Standring S, editor. 2008. Development of the back: development of vertebrae. Gray’s anatomy: the anatomical basis of clinical practice. 40th ed. Elsevier;London: p. 768–9.Jain A., Agarwal A., Jain S., Shamshery C. 2013. Bertolotti syndrome: a diagnostic and management dilemma for pain physicians. Korean J Pain. 26:368–73. DOI: 10.3344/kjp.2013.26.4.368. PMID: 24156003. PMCID: PMC3800709.Apaydin M., Uluc ME., Sezgin G. 2019. Lumbosacral transitional vertebra in the young men population with low back pain: anatomical considerations and degenerations (transitional vertebra types in the young men population with low back pain). Radiol Med. 124:375–81. DOI: 10.1007/s11547-018-0974-4. PMID: 30547357.Peh WC., Siu TH., Chan JH. 1999. Determining the lumbar vertebral segments on magnetic resonance imaging. Spine (Phila Pa 1976). 24:1852–5. DOI: 10.1097/00007632-199909010-00017. PMID: 10488518.Hughes RJ., Saifuddin A. 2006. Numbering of lumbosacral transitional vertebrae on MRI: role of the iliolumbar ligaments. AJR Am J Roentgenol. 187:W59–65. DOI: 10.2214/AJR.05.0415. PMID: 16794140.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anthropologic Study of Korean Mandible Using Three--dimensional Computed Tomography--Evaluation of the Accuracy of a Three--dimensional Image
- THREE-DIMENSIONAL CONFUTED TOMOGRAPHY FOR EVALUATION AND PLANNING OF ORAL AND MAXILLOFACIAL SURGERY
- Morphometrical dimensions of the sheep thoracolumbar vertebrae as seen on digitised CT images
- Ameloblastoma with dystrophic calcification: A case report with 3-dimensional cone-beam computed tomographic images of calcification
- Prevalence of Lumbosacral Transitional Vertebra in Individuals with Low Back Pain: Evaluation Using Plain Radiography and Magnetic Resonance Imaging