Brain Tumor Res Treat.
2020 Apr;8(1):29-35. 10.14791/btrt.2020.8.e10.
Re-Irradiation and Its Contribution to Good Prognosisin Recurrent Glioblastoma Patients
- Affiliations
-
- 1Departments of 1Radiation Oncology, Bundang CHA Medical Center, CHA University College of Medicine, Seongnam, Korea
- 2Departments of Neurosurgery, Bundang CHA Medical Center, CHA University College of Medicine, Seongnam, Korea
- KMID: 2500119
- DOI: http://doi.org/10.14791/btrt.2020.8.e10
Abstract
- Background
: Radiation therapy, one of the strongest anti-cancer treatments, is already performed to treat primary glioblastoma; however, the effect of repeated radiation therapy for recurrent tumors has not been fully explored. The aim of this study was to determine the efficacy of re-irradiation in treating recurrent glioblastoma.
Methods
: The study included 36 patients with recurrent glioblastoma treated with repeated radiation therapy between 2002 and 2016. Stereotactic radiosurgery (SRS) and hypo-fractionated stereotactic radiotherapy (HSRT) were performed in these patients.
Results
: Fourteen patients received SRS with a median dose of 25 Gy (range, 20-32 Gy) in 1-5 fractions. Twenty-two patients received HSRT with a median dose of 40 Gy (range, 31.5-52 Gy) in 6-20 fractions. There were six treatment-related grade 3 adverse events. Survival analysis showed that re-irradiation significantly prolonged overall survival (OS) and progression-free survival (PFS). The median OS and one-year OS rate after re-irradiation were 17.2 months and 60.4%, respectively. The median PFS and 6-month PFS rate after re-irradiation were 4.4 months and 41.9%, respectively. Of the 36 patients, three survived without any progression in their condition.
Conclusion
: Re-irradiation for recurrent glioblastoma showed favorable outcomes. Radiation dose and fractionation should be carefully considered to minimize radiation necrosis.
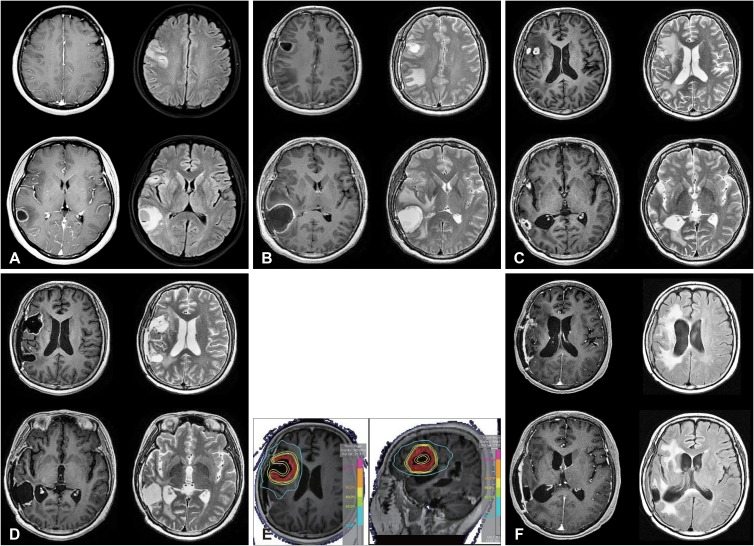
Figure
Reference
-
1. Stupp R, Mason WP, van den Bent MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005; 352:987–996. PMID: 15758009.2. Patel M, Siddiqui F, Jin JY, et al. Salvage reirradiation for recurrent glioblastoma with radiosurgery: radiographic response and improved survival. J Neurooncol. 2009; 92:185–191. PMID: 19066727.3. Gallego O. Nonsurgical treatment of recurrent glioblastoma. Curr Oncol. 2015; 22:e273–e281. PMID: 26300678.4. Roy S, Lahiri D, Maji T, Biswas J. Recurrent glioblastoma: where we stand. South Asian J Cancer. 2015; 4:163–173. PMID: 26981507.5. Redmond KJ, Mehta M. Stereotactic radiosurgery for glioblastoma. Cureus. 2015; 7:e413. PMID: 26848407.6. Ryu S, Buatti JM, Morris A, et al. The role of radiotherapy in the management of progressive glioblastoma : a systematic review and evidence-based clinical practice guideline. J Neurooncol. 2014; 118:489–499. PMID: 24728785.7. Torok JA, Wegner RE, Mintz AH, Heron DE, Burton SA. Re-irradiation with radiosurgery for recurrent glioblastoma multiforme. Technol Cancer Res Treat. 2011; 10:253–258. PMID: 21517131.8. Holt DE, Bernard ME, Quan K, et al. Salvage stereotactic radiosurgery for recurrent glioblastoma multiforme with prior radiation therapy. J Cancer Res Ther. 2016; 12:1243–1248. PMID: 28169234.9. U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE). Version 4.3. Bethesda, MD: U.S. Department of Health and Human Services;2010. Accessed April 19, 2017. at https://www.eortc.be/services/doc/ctc/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf.10. Fogh SE, Andrews DW, Glass J, et al. Hypofractionated stereotactic radiation therapy: an effective therapy for recurrent high-grade gliomas. J Clin Oncol. 2010; 28:3048–3053. PMID: 20479391.11. Maranzano E, Anselmo P, Casale M, et al. Treatment of recurrent glioblastoma with stereotactic radiotherapy: long-term results of a mono-institutional trial. Tumori. 2011; 97:56–61. PMID: 21528665.12. Cuneo KC, Vredenburgh JJ, Sampson JH, et al. Safety and efficacy of stereotactic radiosurgery and adjuvant bevacizumab in patients with recurrent malignant gliomas. Int J Radiat Oncol Biol Phys. 2012; 82:2018–2024. PMID: 21489708.13. Minniti G, Scaringi C, De Sanctis V, et al. Hypofractionated stereotactic radiotherapy and continuous low-dose temozolomide in patients with recurrent or progressive malignant gliomas. J Neurooncol. 2013; 111:187–194. PMID: 23129347.14. Greenspoon JN, Sharieff W, Hirte H, et al. Fractionated stereotactic radiosurgery with concurrent temozolomide chemotherapy for locally recurrent glioblastoma multiforme: a prospective cohort study. Onco Targets Ther. 2014; 7:485–490. PMID: 24711705.15. Minniti G, Agolli L, Falco T, et al. Hypofractionated stereotactic radiotherapy in combination with bevacizumab or fotemustine for patients with progressive malignant gliomas. J Neurooncol. 2015; 122:559–566. PMID: 25702193.16. Kim BS, Kong DS, Seol HJ, Nam DH, Lee JI. MGMT promoter methylation status as a prognostic factor for the outcome of gamma knife radiosurgery for recurrent glioblastoma. J Neurooncol. 2017; 133:615–622. PMID: 28536992.17. Back M, Gzell CE, Kastelan M, Guo L, Wheeler HR. Large volume re-irradiation with bevacizumab is a feasible salvage option for patients with refractory high-grade glioma. Neurooncol Pract. 2015; 2:48–53. PMID: 26034641.18. Azoulay M, Santos F, Shenouda G, et al. Benefit of re-operation and salvage therapies for recurrent glioblastoma multiforme: results from a single institution. J Neurooncol. 2017; 132:419–426. PMID: 28374095.19. Lu VM, Goyal A, Graffeo CS, et al. Survival benefit of maximal resection for glioblastoma reoperation in the temozolomide era: a meta-analysis. World Neurosurg. 2019; 127:31–37. PMID: 30947000.20. Martínez-Carrillo M, Tovar-Martín I, Zurita-Herrera M, et al. Salvage radiosurgery for selected patients with recurrent malignant gliomas. Biomed Res Int. 2014; 2014:657953. PMID: 24895599.21. Scharfen CO, Sneed PK, Wara WM, et al. High activity iodine-125 interstitial implant for gliomas. Int J Radiat Oncol Biol Phys. 1992; 24:583–591. PMID: 1429079.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Appraisal of re-irradiation for the recurrent glioblastoma in the era of MGMT promotor methylation
- Intracavitary Irradiation of Locally Advanced Recurrent Adenocarcinoma of Rectum Along the Fistula tract
- Hypofractionated Re-irradiation after Maximal Surgical Resection for Recurrent Glioblastoma: Therapeutic Adequacy and Its Prognosticators of Survival
- Re-Irradiation for Recurrent Gliomas: Treatment Outcomes and Prognostic Factors
- Radiation-Induced Glioblastoma Multiforme in a Remitted Acute Lymphocytic Leukemia Patient