Obstet Gynecol Sci.
2020 Mar;63(2):108-116. 10.5468/ogs.2020.63.2.108.
Fetal therapies as standard prenatal care in Japan
- Affiliations
-
- 1Center for Maternal-Fetal, Neonatal and Reproductive Medicine, National Center for Child Health and Development, Tokyo, Japan. sagou-h@ncchd.go.jp
- KMID: 2471747
- DOI: http://doi.org/10.5468/ogs.2020.63.2.108
Abstract
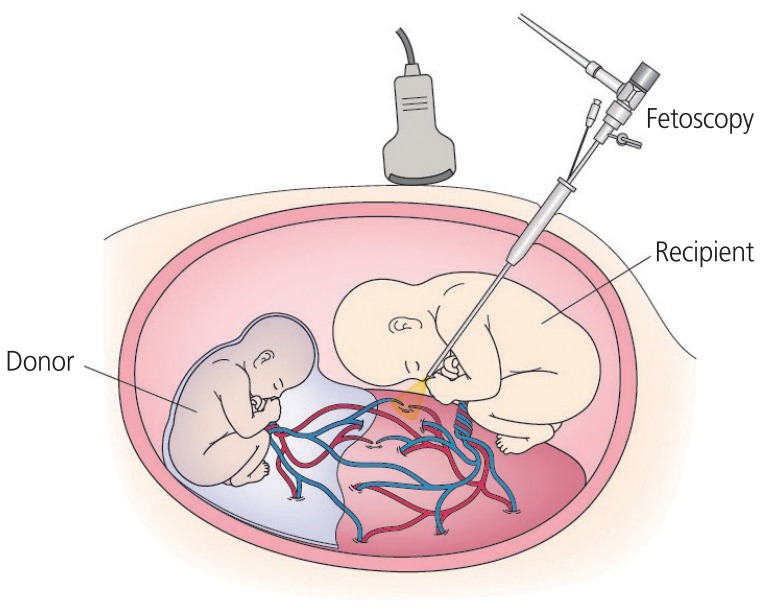
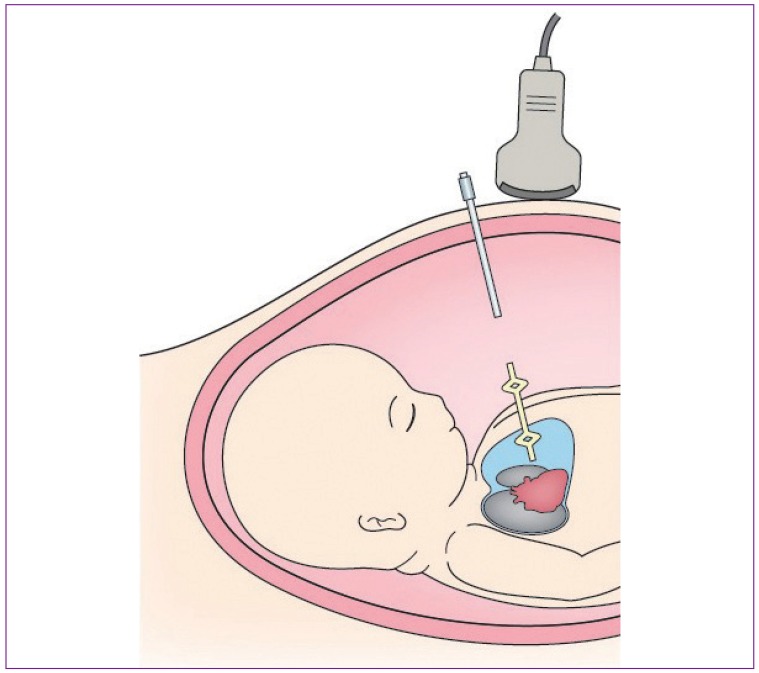
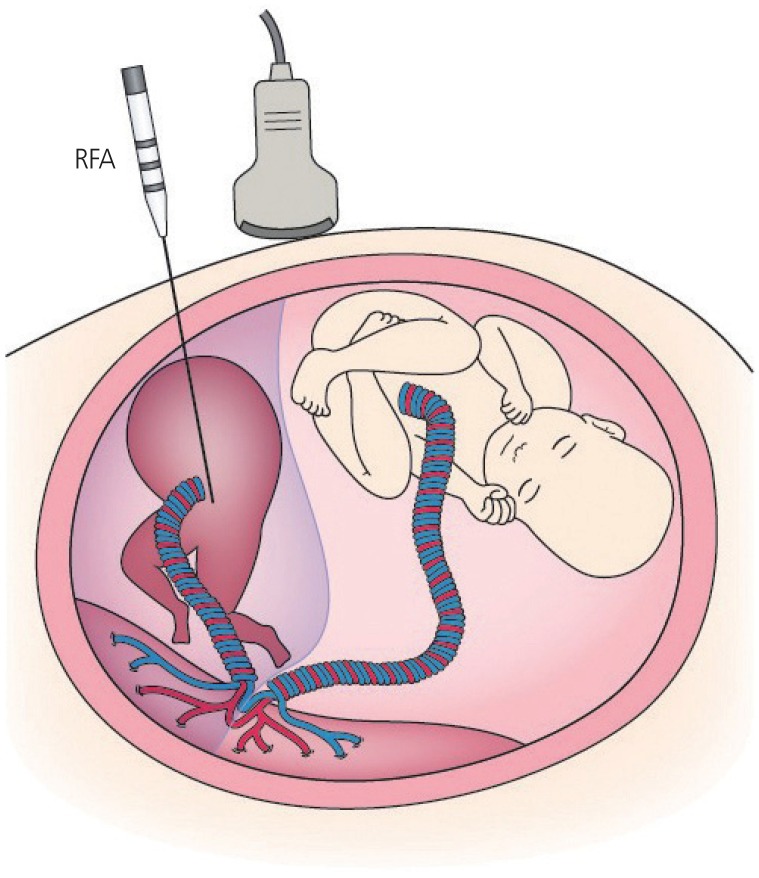
- With recent advances in fetal medicine, various attempts have been made to save fetuses facing perinatal death or devastating consequences despite optimal management after birth. The concept of the fetus as a patient has been established through the application of in utero treatments. This paper reviews fetal therapies in order to highlight the role of perinatal medicine as standard prenatal care. Fetal therapies consist of medical therapy, percutaneous ultrasound-guided surgery, fetoscopic surgery, and open fetal surgery. In the 1980s, with advances in ultrasound imaging, percutaneous ultrasound-guided surgeries such as vesicoamniotic shunting for lower urinary tract obstruction and thoracoamniotic shunting (TAS) for fetal hydrothorax (FHT) were started. In the 1990s, fetoscopic laser surgery (FLS) for twin-twin transfusion syndrome (TTTS) was introduced, and later, a fetoscopic approach for congenital diaphragmatic hernia was also established. The revival of open fetal surgery, introduced in the 1980s by pediatric surgeons, began in the 2010s after a successful clinical study for myelomeningocele. Although many fetal therapies are still considered experimental, some have proven effective, such as FLS for TTTS, TAS for primary FHT, and radiofrequency ablation (RFA) for twin reversed arterial perfusion (TRAP) sequence. These three fetal therapies have been approved for coverage by Japan National Health Insurance as a result of clinical studies performed in Japan. FLS for TTTS, TAS for primary FHT, and RFA for TRAP sequence have become standard prenatal care approaches in Japan. These three minimally invasive fetal therapies will help improve the perinatal outcomes of fetuses with these disorders.
MeSH Terms
Figure
Cited by 1 articles
-
Fetal growth changes and prediction of selective fetal growth restriction following fetoscopic laser coagulation in twin-to-twin transfusion syndrome
So Yeon Kim, Hye-Sung Won, Mi-Young Lee, Jin Hoon Chung, Jin-Hee Park, You-Kyoung Kim, Hwang-Mi Lee
Obstet Gynecol Sci. 2023;66(6):529-536. doi: 10.5468/ogs.23108.
Reference
-
1. Liley AW. Intrauterine transfusion of foetus in haemolytic disease. BMJ. 1963; 2:1107–1109. PMID: 14057715.
Article2. Bang J, Bock JE, Trolle D. Ultrasound-guided fetal intravenous transfusion for severe rhesus haemolytic disease. Br Med J (Clin Res Ed). 1982; 284:373–374.
Article3. Golbus MS, Harrison MR, Filly RA, Callen PW, Katz M. In utero treatment of urinary tract obstruction. Am J Obstet Gynecol. 1982; 142:383–388. PMID: 7199255.4. Rodeck CH, Fisk NM, Fraser DI, Nicolini U. Long-term in utero drainage of fetal hydrothorax. N Engl J Med. 1988; 319:1135–1138. PMID: 3173443.5. Crombleholme TM, Harrison MR, Langer JC, Longaker MT, Anderson RL, Slotnick NS, et al. Early experience with open fetal surgery for congenital hydronephrosis. J Pediatr Surg. 1988; 23:1114–1121. PMID: 3236176.
Article6. Adzick NS, Harrison MR, Flake AW, Howell LJ, Golbus MS, Filly RA. Fetal surgery for cystic adenomatoid malformation of the lung. J Pediatr Surg. 1993; 28:806–812. PMID: 8331508.7. Harrison MR, Adzick NS, Longaker MT, Goldberg JD, Rosen MA, Filly RA, et al. Successful repair in utero of a fetal diaphragmatic hernia after removal of herniated viscera from the left thorax. N Engl J Med. 1990; 322:1582–1584. PMID: 2336088.8. De Lia JE, Cruikshank DP, Keye WR Jr. Fetoscopic neodymium:YAG laser occlusion of placental vessels in severe twin-twin transfusion syndrome. Obstet Gynecol. 1990; 75:1046–1053. PMID: 2342732.9. Ville Y, Hyett J, Hecher K, Nicolaides K. Preliminary experience with endoscopic laser surgery for severe twin-twin transfusion syndrome. N Engl J Med. 1995; 332:224–227. PMID: 7808488.
Article10. Ville Y, Hecher K, Gagnon A, Sebire N, Hyett J, Nicolaides K. Endoscopic laser coagulation in the management of severe twin-to-twin transfusion syndrome. Br J Obstet Gynaecol. 1998; 105:446–453. PMID: 9609274.
Article11. Senat MV, Deprest J, Boulvain M, Paupe A, Winer N, Ville Y. Endoscopic laser surgery versus serial amnioreduction for severe twin-to-twin transfusion syndrome. N Engl J Med. 2004; 351:136–144. PMID: 15238624.
Article12. Harrison MR, Keller RL, Hawgood SB, Kitterman JA, Sandberg PL, Farmer DL, et al. A randomized trial of fetal endoscopic tracheal occlusion for severe fetal congenital diaphragmatic hernia. N Engl J Med. 2003; 349:1916–1924. PMID: 14614166.
Article13. Deprest J, Gratacos E, Nicolaides KH. FETO Task Group. Fetoscopic tracheal occlusion (FETO) for severe congenital diaphragmatic hernia: evolution of a technique and preliminary results. Ultrasound Obstet Gynecol. 2004; 24:121–126. PMID: 15287047.
Article14. Adzick NS, Thom EA, Spong CY, Brock JW 3rd, Burrows PK, Johnson MP, et al. A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med. 2011; 364:993–1004. PMID: 21306277.
Article15. Deprest JA, Flake AW, Gratacos E, Ville Y, Hecher K, Nicolaides K, et al. The making of fetal surgery. Prenat Diagn. 2010; 30:653–667. PMID: 20572114.
Article16. Sago H, Ishii K, Sugibayashi R, Ozawa K, Sumie M, Wada S. Fetoscopic laser photocoagulation for twin-twin transfusion syndrome. J Obstet Gynaecol Res. 2018; 44:831–839. PMID: 29436080.
Article17. Fetal therapy. In : Cunningham FG, Leveno KJ, Bloom SL, Dashe JS, Hoffman BL, Casey BM, editors. Williams obstetrics. 25th ed. New York (NY): McGraw-Hill Education;2018. p. 315–330.18. Slaghekke F, Lopriore E, Lewi L, Middeldorp JM, van Zwet EW, Weingertner AS, et al. Fetoscopic laser coagulation of the vascular equator versus selective coagulation for twin-to-twin transfusion syndrome: an open-label randomised controlled trial. Lancet. 2014; 383:2144–2151. PMID: 24613024.
Article19. Mahony BS, Petty CN, Nyberg DA, Luthy DA, Hickok DE, Hirsch JH. The “stuck twin” phenomenon: ultrasonographic findings, pregnancy outcome, and management with serial amniocenteses. Am J Obstet Gynecol. 1990; 163:1513–1522. PMID: 2240099.
Article20. Quintero RA, Morales WJ, Allen MH, Bornick PW, Johnson PK, Kruger M. Staging of twin-twin transfusion syndrome. J Perinatol. 1999; 19:550–555. PMID: 10645517.
Article21. Diehl W, Hecher K, Zikulnig L, Vetter M, Hackelöer BJ. Placental vascular anastomoses visualized during fetoscopic laser surgery in severe mid-trimester twin-twin transfusion syndrome. Placenta. 2001; 22:876–881. PMID: 11718576.
Article22. Sago H, Hayashi S, Saito M, Hasegawa H, Kawamoto H, Kato N, et al. The outcome and prognostic factors of twin-twin transfusion syndrome following fetoscopic laser surgery. Prenat Diagn. 2010; 30:1185–1191. PMID: 21064193.
Article23. Diehl W, Diemert A, Grasso D, Sehner S, Wegscheider K, Hecher K. Fetoscopic laser coagulation in 1020 pregnancies with twin-twin transfusion syndrome demonstrates improvement in double-twin survival rate. Ultrasound Obstet Gynecol. 2017; 50:728–735. PMID: 28477345.
Article24. Sato Y, Ishii K, Yokouchi T, Murakoshi T, Kiyoshi K, Nakayama S, et al. Incidences of feto-fetal transfusion syndrome and perinatal outcomes in triplet gestations with monochorionic placentation. Fetal Diagn Ther. 2016; 40:181–186. PMID: 26760043.
Article25. Sepulveda W, Surerus E, Vandecruys H, Nicolaides KH. Fetofetal transfusion syndrome in triplet pregnancies: outcome after endoscopic laser surgery. Am J Obstet Gynecol. 2005; 192:161–164. PMID: 15672019.
Article26. Ishii K, Nakata M, Wada S, Hayashi S, Murakoshi T, Sago H. Perinatal outcome after laser surgery for triplet gestations with feto-fetal transfusion syndrome. Prenat Diagn. 2014; 34:734–738. PMID: 24659408.
Article27. Valsky DV, Eixarch E, Martinez-Crespo JM, Acosta ER, Lewi L, Deprest J, et al. Fetoscopic laser surgery for twin-to-twin transfusion syndrome after 26 weeks of gestation. Fetal Diagn Ther. 2012; 31:30–34. PMID: 22156583.
Article28. Baud D, Windrim R, Keunen J, Kelly EN, Shah P, van Mieghem T, et al. Fetoscopic laser therapy for twin-twin transfusion syndrome before 17 and after 26 weeks' gestation. Am J Obstet Gynecol. 2013; 208:197.e1–197.e7. PMID: 23178244.
Article29. Nakata M, Ishii K, Sumie M, Takano M, Hirata H, Murata S, et al. A prospective pilot study of fetoscopic laser surgery for twin-to-twin transfusion syndrome between 26 and 27 weeks of gestation. Taiwan J Obstet Gynecol. 2016; 55:512–514. PMID: 27590373.
Article30. Quintero RA, Bornick PW, Morales WJ, Allen MH. Selective photocoagulation of communicating vessels in the treatment of monochorionic twins with selective growth retardation. Am J Obstet Gynecol. 2001; 185:689–696. PMID: 11568799.
Article31. Gratacós E, Antolin E, Lewi L, Martínez JM, Hernandez-Andrade E, Acosta-Rojas R, et al. Monochorionic twins with selective intrauterine growth restriction and intermittent absent or reversed end-diastolic flow (Type III): feasibility and perinatal outcome of fetoscopic placental laser coagulation. Ultrasound Obstet Gynecol. 2008; 31:669–675. PMID: 18504780.
Article32. Chalouhi GE, Marangoni MA, Quibel T, Deloison B, Benzina N, Essaoui M, et al. Active management of selective intrauterine growth restriction with abnormal Doppler in monochorionic diamniotic twin pregnancies diagnosed in the second trimester of pregnancy. Prenat Diagn. 2013; 33:109–115. PMID: 23280487.
Article33. Ishii K, Nakata M, Wada S, Murakoshi T, Sago H. Feasibility and preliminary outcomes of fetoscopic laser photocoagulation for monochorionic twin gestation with selective intrauterine growth restriction accompanied by severe oligohydramnios. J Obstet Gynaecol Res. 2015; 41:1732–1737. PMID: 26369752.
Article34. Ishii K, Wada S, Takano M, Nakata M, Murakoshi T, Sago H. Survival rate without brain abnormalities on postnatal ultrasonography among monochorionic twins after fetoscopic laser photocoagulation for selective intrauterine growth restriction with concomitant oligohydramnios. Fetal Diagn Ther. 2019; 45:21–27. PMID: 29462812.
Article35. Smith RP, Illanes S, Denbow ML, Soothill PW. Outcome of fetal pleural effusions treated by thoracoamniotic shunting. Ultrasound Obstet Gynecol. 2005; 26:63–66. PMID: 15861415.
Article36. Achiron R, Weissman A, Lipitz S, Mashiach S, Goldman B. Fetal pleural effusion: the risk of fetal trisomy. Gynecol Obstet Invest. 1995; 39:153–156. PMID: 7789908.
Article37. Barron SD, Pass RF. Infectious causes of hydrops fetalis. Semin Perinatol. 1995; 19:493–501. PMID: 8822333.
Article38. Longaker MT, Laberge JM, Dansereau J, Langer JC, Crombleholme TM, Callen PW, et al. Primary fetal hydrothorax: natural history and management. J Pediatr Surg. 1989; 24:573–576. PMID: 2661800.
Article39. Weber AM, Philipson EH. Fetal pleural effusion: a review and meta-analysis for prognostic indicators. Obstet Gynecol. 1992; 79:281–286. PMID: 1530987.40. Yinon Y, Grisaru-Granovsky S, Chaddha V, Windrim R, Seaward PG, Kelly EN, et al. Perinatal outcome following fetal chest shunt insertion for pleural effusion. Ultrasound Obstet Gynecol. 2010; 36:58–64. PMID: 20069656.
Article41. Jeong BD, Won HS, Lee MY, Shim JY, Lee PR, Kim A. Perinatal outcomes of fetal pleural effusion following thoracoamniotic shunting. Prenat Diagn. 2015; 35:1365–1370. PMID: 26479499.
Article42. Chiba Y, Kobayashi H, Kanzaki T, Murakami M, Takahashi S, Takahashi H. Clinical aspects of fetal obstructive uropathy with in utero estimation of renal function and intrauterine shunt placement. J Matern Fetal Investig. 1993; 3:225–231.43. Takahashi Y, Kawabata I, Sumie M, Nakata M, Ishii K, Murakoshi T, et al. Thoracoamniotic shunting for fetal pleural effusions using a double-basket shunt. Prenat Diagn. 2012; 32:1282–1287. PMID: 23138652.
Article44. Wada S, Jwa SC, Yumoto Y, Takahashi Y, Ishii K, Usui N, et al. The prognostic factors and outcomes of primary fetal hydrothorax with the effects of fetal intervention. Prenat Diagn. 2017; 37:184–192. PMID: 27977046.
Article45. Yumoto Y, Jwa SC, Wada S, Takahashi Y, Ishii K, Kato K, et al. The outcomes and prognostic factors of fetal hydrothorax associated with trisomy 21. Prenat Diagn. 2017; 37:686–692. PMID: 28493447.
Article46. Gillim DL, Hendricks CH. Holoacardius; review of the literature and case report. Obstet Gynecol. 1953; 2:647–653. PMID: 13120037.47. Moore TR, Gale S, Benirschke K. Perinatal outcome of forty-nine pregnancies complicated by acardiac twinning. Am J Obstet Gynecol. 1990; 163:907–912. PMID: 2206078.
Article48. Lewi L, Gratacos E, Ortibus E, Van Schoubroeck D, Carreras E, Higueras T, et al. Pregnancy and infant outcome of 80 consecutive cord coagulations in complicated monochorionic multiple pregnancies. Am J Obstet Gynecol. 2006; 194:782–789. PMID: 16522413.
Article49. Lanna MM, Rustico MA, Dell'Avanzo M, Schena V, Faiola S, Consonni D, et al. Bipolar cord coagulation for selective feticide in complicated monochorionic twin pregnancies: 118 consecutive cases at a single center. Ultrasound Obstet Gynecol. 2012; 39:407–413. PMID: 22173905.
Article50. Scheier M, Molina FS. Outcome of twin reversed arterial perfusion sequence following treatment with interstitial laser: a retrospective study. Fetal Diagn Ther. 2012; 31:35–41. PMID: 22204966.
Article51. Chaveeva P, Poon LC, Sotiriadis A, Kosinski P, Nicolaides KH. Optimal method and timing of intrauterine intervention in twin reversed arterial perfusion sequence: case study and meta-analysis. Fetal Diagn Ther. 2014; 35:267–279. PMID: 24751835.
Article52. Tsao K, Feldstein VA, Albanese CT, Sandberg PL, Lee H, Harrison MR, et al. Selective reduction of acardiac twin by radiofrequency ablation. Am J Obstet Gynecol. 2002; 187:635–640. PMID: 12237640.
Article53. Gaerty K, Greer RM, Kumar S. Systematic review and metaanalysis of perinatal outcomes after radiofrequency ablation and bipolar cord occlusion in monochorionic pregnancies. Am J Obstet Gynecol. 2015; 213:637–643. PMID: 25935786.
Article54. Bebbington MW, Danzer E, Moldenhauer J, Khalek N, Johnson MP. Radiofrequency ablation vs bipolar umbilical cord coagulation in the management of complicated monochorionic pregnancies. Ultrasound Obstet Gynecol. 2012; 40:319–324. PMID: 22302774.55. Lee H, Bebbington M, Crombleholme TM. North American Fetal Therapy Network. The North American Fetal Therapy Network Registry data on outcomes of radiofrequency ablation for twin-reversed arterial perfusion sequence. Fetal Diagn Ther. 2013; 33:224–229. PMID: 23594603.
Article56. Sugibayashi R, Ozawa K, Sumie M, Wada S, Ito Y, Sago H. Forty cases of twin reversed arterial perfusion sequence treated with radio frequency ablation using the multistep coagulation method: a single-center experience. Prenat Diagn. 2016; 36:437–443. PMID: 26934598.
Article57. Wagata M, Murakoshi T, Ishii K, Muromoto J, Sasahara J, Murotsuki J. Radiofrequency ablation with an internally cooled electrode for twin reversed arterial perfusion sequence. Fetal Diagn Ther. 2016; 40:110–115. PMID: 26928848.
Article58. Kitano Y, Chiba T, Kuroda T, Sago H, Hayashi S, Kitagawa M, et al. Open fetal surgery for congenital cystic adenomatoid malformation complicated with fetal hydrops: A case report. J Jpn Soc Perin Neon Med. 2005; 41:67–72.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Trends in Fetal and Perinatal Mortality in Korea (2009–2014): Comparison with Japan and the United States
- An unusual prenatal manifestation of a huge congenital cystic adenomatoid malformation with favorable perinatal outcome
- The Present of Fetal Therapy and Future Prospect
- Prenatal Diagnosis of Intrauterine Fetal Femur Fracture
- Technique of fetal echocardiography