Korean J Radiol.
2019 Dec;20(12):1627-1637. 10.3348/kjr.2019.0084.
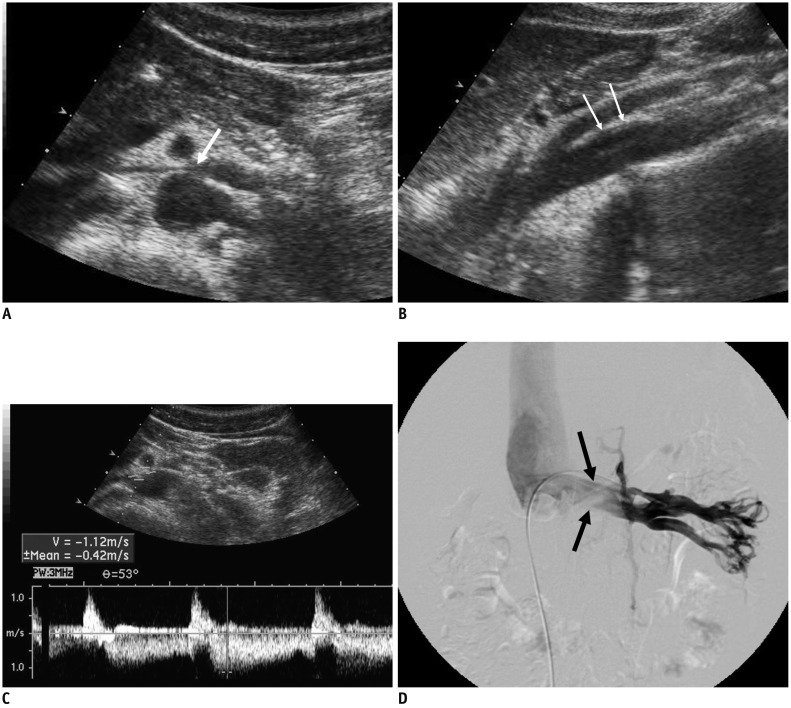
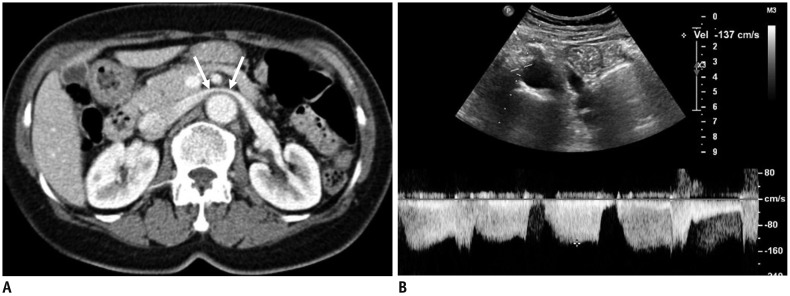
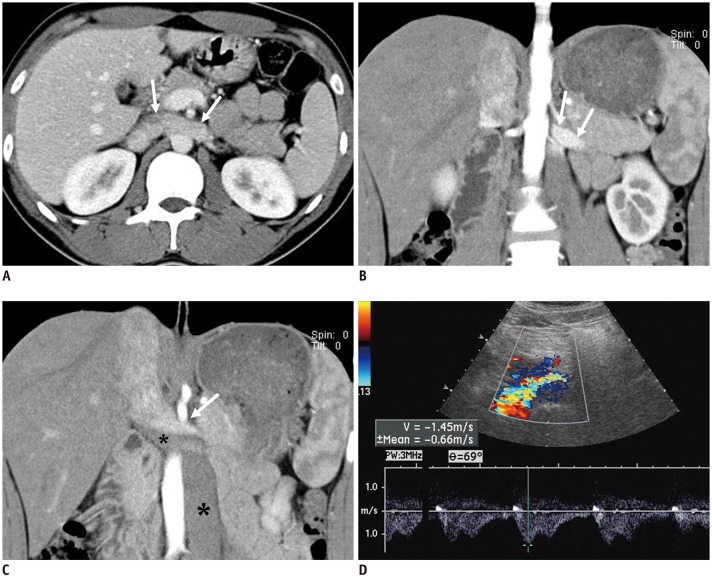
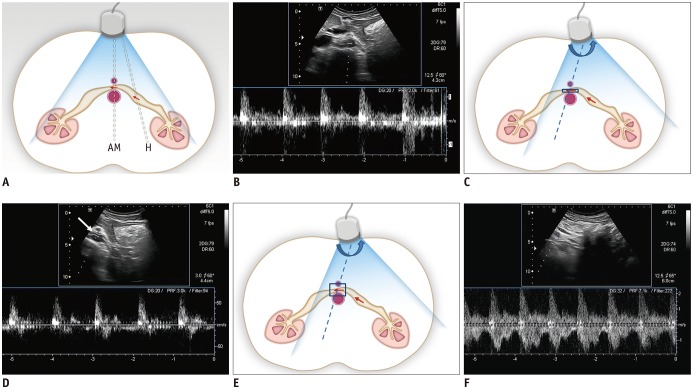
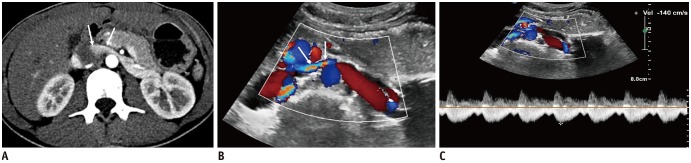
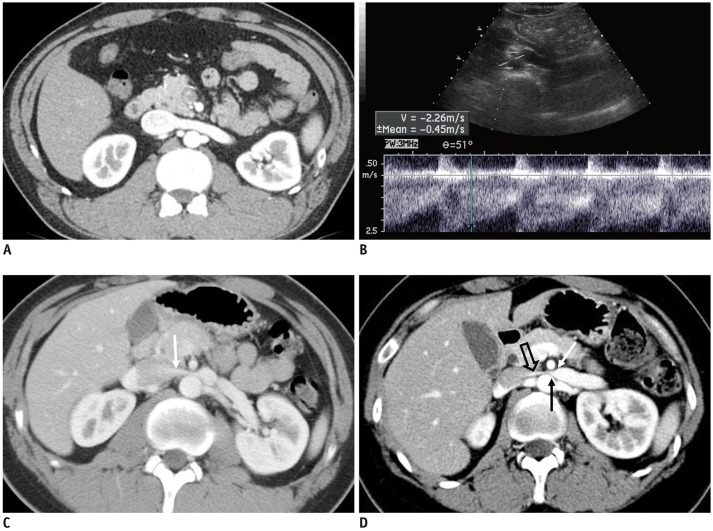
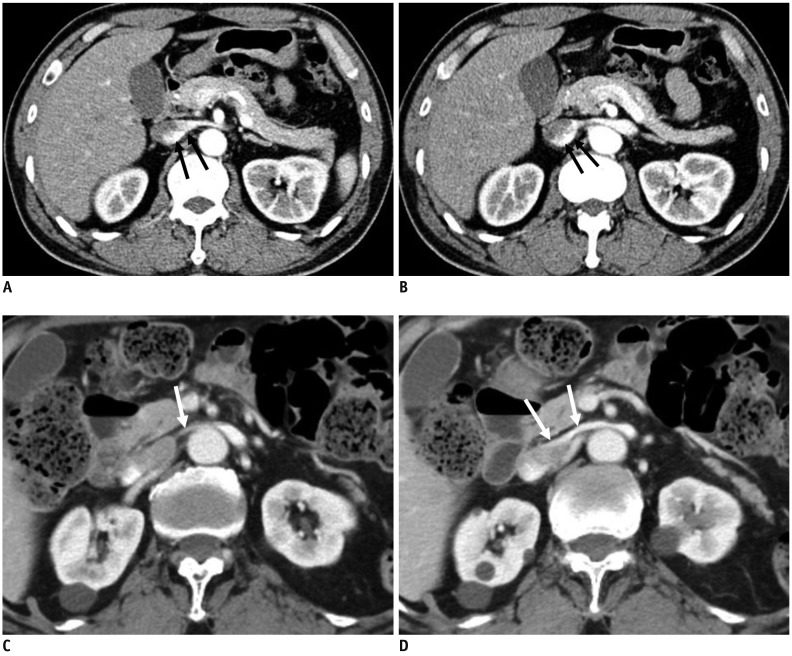
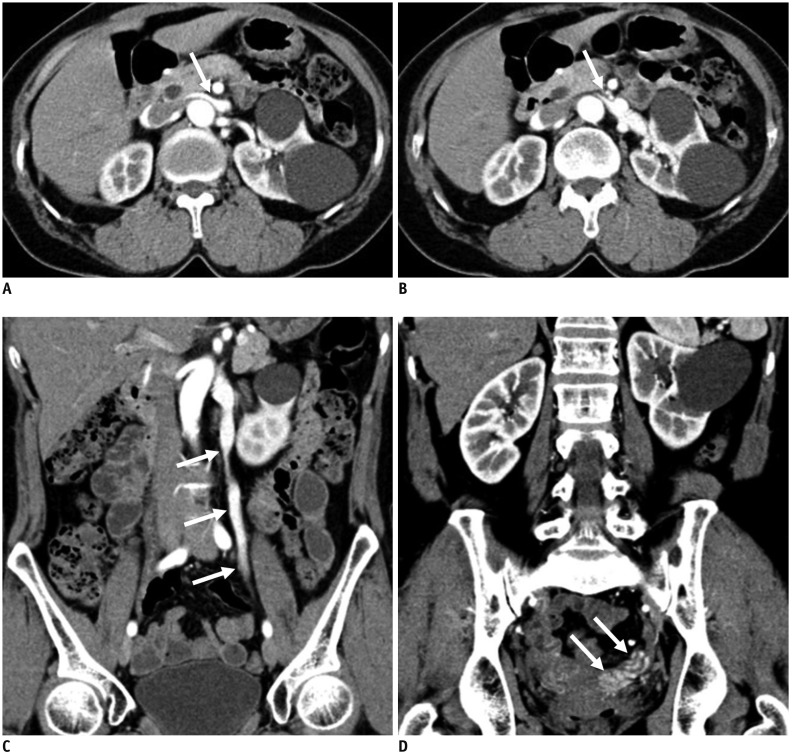
Doppler US and CT Diagnosis of Nutcracker Syndrome
- Affiliations
-
- 1Department of Radiology, Seoul National University Hospital, Seoul, Korea. kimshrad@snu.ac.kr
- 2Kidney Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2471675
- DOI: http://doi.org/10.3348/kjr.2019.0084
Abstract
- Nutcracker syndrome (NCS) is a syndrome caused by compression of the left renal vein (LRV), between the abdominal aorta and the superior mesenteric artery, resulting in hypertension of the LRV and hematuria. Doppler ultrasonography (US) has been commonly used for the diagnosis of NCS. However, several technical issues, such as Doppler angle and sample volume, need to be considered to obtain satisfactory results. In addition, morphologic changes of the LRV and a jetting phenomenon across the aortomesenteric portion of the LRV on contrast-enhanced computed tomography (CECT) are diagnostic clues of NCS. With proper Doppler US and CECT, NCS can be diagnosed noninvasively.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Nutcracker syndrome in children: review of symptom, diagnosis, and treatment
Diana S. Kalantar, Se Jin Park, Jae Il Shin
Child Kidney Dis. 2023;27(2):89-96. doi: 10.3339/ckd.23.018.Effect of renal Doppler ultrasound on the detection of nutcracker syndrome in children presenting orthostatic proteinuria
Eun Jae Hwang, Ji Hong Kim, Mi-Jung Lee, Haesung Yoon, Jae Il Shin, Keum Hwa Lee
Child Kidney Dis. 2024;28(2):74-79. doi: 10.3339/ckd.24.009.
Reference
-
1. El-Sadr AR, Mina E. Anatomical and surgical aspects in the operative management of varicocele. Urol Cutaneous Rev. 1950; 54:257–262. PMID: 15443180.2. Chait A, Matasar KW, Fabian CE, Mellins HZ. Vascular impressions on the ureters. Am J Roentgenol Radium Ther Nucl Med. 1971; 111:729–749.
Article3. de Schepper A. [“Nutcracker” phenomenon of the renal vein and venous pathology of the left kidney]. J Belge Radiol. 1972; 55:507–511. PMID: 4660828.4. Welsch T, Büchler MW, Kienle P. Recalling superior mesenteric artery syndrome. Dig Surg. 2007; 24:149–156. PMID: 17476104.
Article5. Ananthan K, Onida S, Davies AH. Nutcracker syndrome: an update on current diagnostic criteria and management guidelines. Eur J Vasc Endovasc Surg. 2017; 53:886–894. PMID: 28356209.
Article6. Nishimura Y, Fushiki M, Yoshida M, Nakamura K, Imai M, Ono T, et al. Left renal vein hypertension in patients with left renal bleeding of unknown origin. Radiology. 1986; 160:663–667. PMID: 3737903.
Article7. Kim SH, Cho SW, Kim HD, Chung JW, Park JH, Han MC. Nutcracker syndrome: diagnosis with Doppler US. Radiology. 1996; 198:93–97. PMID: 8539413.
Article8. Cheon JE, Kim WS, Kim IO, Kim SH, Yeon KM, Ha IS, et al. Nutcracker syndrome in children with gross haematuria: Doppler sonographic evaluation of the left renal vein. Pediatr Radiol. 2006; 36:682–686. PMID: 16770671.
Article9. Kim KW, Cho JY, Kim SH, Yoon JH, Kim DS, Chung JW, et al. Diagnostic value of computed tomographic findings of nutcracker syndrome: correlation with renal venography and renocaval pressure gradients. Eur J Radiol. 2011; 80:648–654. PMID: 20869828.
Article10. Kurklinsky AK, Rooke TW. Nutcracker phenomenon and nutcracker syndrome. Mayo Clin Proc. 2010; 85:552–559. PMID: 20511485.
Article11. Beinart C, Sniderman KW, Saddekni S, Weiner M, Vaughan ED Jr, Sos TA. Left renal vein hypertension: a cause of occult hematuria. Radiology. 1982; 145:647–650. PMID: 7146391.
Article12. Oteki T, Nagase S, Hirayama A, Sugimoto H, Hirayama K, Hattori K, et al. Nutcracker syndrome associated with severe anemia and mild proteinuria. Clin Nephrol. 2004; 62:62–65. PMID: 15267016.
Article13. Trambert JJ, Rabin AM, Weiss KL, Tein AB. Pericaliceal varices due to the nutcracker phenomenon. AJR Am J Roentgenol. 1990; 154:305–306. PMID: 2105019.
Article14. Cho BS, Choi YM, Kang HH, Park SJ, Lim JW, Yoon TY. Diagnosis of nut-cracker phenomenon using renal Doppler ultrasound in orthostatic proteinuria. Nephrol Dial Transplant. 2001; 16:1620–1625. PMID: 11477164.
Article15. Park SJ, Lim JW, Cho BS, Yoon TY, Oh JH. Nutcracker syndrome in children with orthostatic proteinuria: diagnosis on the basis of Doppler sonography. J Ultrasound Med. 2002; 21:39–45. PMID: 11794401.16. Pournasiri Z. The nutcracker syndrome as a rare cause of chronic abdominal pain: a case report. J Compr Ped. 2016; 7:e39741.
Article17. Taktak A, Hakan Demirkan T, Acar B, Gu R G, Köksoy A, Uncu N, et al. Clinico-radiological correlation of nutcracker syndrome: a single centre experience. Arch Argent Pediatr. 2017; 115:165–168. PMID: 28318183.
Article18. Liebl R. Nutcracker phenomenon or nutcracker syndrome? Nephrol Dial Transplant. 2005; 20:2009. author reply 2009. PMID: 15985517.
Article19. Buschi AJ, Harrison RB, Norman A, Brenbridge AG, Williamson BR, Gentry RR, et al. Distended left renal vein: CT/sonographic normal variant. AJR Am J Roentgenol. 1980; 135:339–342. PMID: 6773339.
Article20. Zerin JM, Hernandez RJ, Sedman AB, Kelsch RC. “Dilatation” of the left renal vein on computed tomography in children: a normal variant. Pediatr Radiol. 1991; 21:267–269. PMID: 1870922.
Article21. Sebro K, Goetz L, Persaud S. Nutcracker syndrome: a rare and potentially under diagnosed cause of haematuria. Case Rep Surg Invasive Proced. 2017; 1:4–6.22. He Y, Wu Z, Chen S, Tian L, Li D, Li M, et al. Nutcracker syndrome—How well do we know it? Urology. 2014; 83:12–17. PMID: 24139744.
Article23. Wendel RG, Crawford ED, Hehman KN. The “nutcracker” phenomenon: an unusual cause for renal varicosities with hematuria. J Urol. 1980; 123:761–763. PMID: 7420571.
Article24. Hayashi M, Kume T, Nihira H. Abnormalities of renal venous system and unexplained renal hematuria. J Urol. 1980; 124:12–16. PMID: 7411696.
Article25. Lau JLT, Lo R, Chan FL, Wong KK. The posterior “nutcracker”: hematuria secondary to retroaortic left renal vein. Urology. 1986; 28:437–439. PMID: 3787913.
Article26. Ali-El-Dein B, Osman Y, Shehab El-Din AB, El-Diasty T, Mansour O, Ghoneim MA. Anterior and posterior nutcracker syndrome: a report on 11 cases. Transplant Proc. 2003; 35:851–853. PMID: 12644163.
Article27. Skeik N, Gloviczki P, Macedo TA. Posterior nutcracker syndrome. Vasc Endovascular Surg. 2011; 45:749–755. PMID: 21890560.
Article28. Özkan MB, Ceyhan Bilgici M, Hayalioglu E. Anterior and posterior nutcracker syndrome accompanying left circumaortic renal vein in an adolescent: case report. Arch Argent Pediatr. 2016; 114:e114–e116. PMID: 27079405.29. Naito M, Terayama H, Nakamura Y, Hayashi S, Miyaki T, Itoh M. Left testicular artery arching over the ipsilateral renal vein. Asian J Androl. 2006; 8:107–110. PMID: 16372128.
Article30. Radisic MV, Feldman D, Diaz C, Froment RO. Unexplained hematuria during pregnancy: right-sided nutcracker phenomenon. Int Urol Nephrol. 2007; 39:709–711. PMID: 17031506.
Article31. Beinart C, Sniderman KW, Tamura S, Vaughan ED Jr, Sos TA. Left renal vein to inferior vena cava pressure relationship in humans. J Urol. 1982; 127:1070–1071. PMID: 7087011.
Article32. Hangge PT, Gupta N, Khurana A, Quencer KB, Albadawi H, Alzubaidi SJ, et al. Degree of left renal vein compression predicts nutcracker syndrome. J Clin Med. 2018; 7:E107. PMID: 29738433.
Article33. Fong JKK, Poh ACC, Tan AGS, Taneja R. Imaging findings and clinical features of abdominal vascular compression syndromes. AJR Am J Roentgenol. 2014; 203:29–36. PMID: 24951193.
Article34. Orczyk K, Wysiadecki G, Majos A, Stefańczyk L, Topol M, Polguj M. What each clinical anatomist has to know about left renal vein entrapment syndrome (nutcracker syndrome): a review of the most important findings. Biomed Res Int. 2017; DOI: 10.1155/2017/1746570. [Epub].
Article35. Ahmed K, Sampath R, Khan MS. Current trends in the diagnosis and management of renal nutcracker syndrome: a review. Eur J Vasc Endovasc Surg. 2006; 31:410–416. PMID: 16431142.
Article36. Hohenfellner M, Steinbach F, Schultz-Lampel D, Schantzen W, Walter K, Cramer BM, et al. The nutcracker syndrome: new aspects of pathophysiology, diagnosis and treatment. J Urol. 1991; 146:685–688. PMID: 1875472.
Article37. Fitoz S, Ekim M, Ozcakar ZB, Elhan AH, Yalcinkaya F. Nutcracker syndrome in children: the role of upright position examination and superior mesenteric artery angle measurement in the diagnosis. J Ultrasound Med. 2007; 26:573–580. PMID: 17459998.38. Stewart BH, Reiman G. Left renal venous hypertension “nutcracker” syndrome: managed by direct renocaval reimplantation. Urology. 1982; 20:365–369. PMID: 7147503.39. Kim SH, Park JH, Han MC, Paick JS. Embolization of the internal spermatic vein in varicocele: significance of venous pressure. Cardiovasc Intervent Radiol. 1992; 15:102–106. PMID: 1571922.
Article40. Zerhouni EA, Siegelman SS, Walsh PC, White RI. Elevated pressure in the left renal vein in patients with varicocele: preliminary observations. J Urol. 1980; 123:512–513. PMID: 7365887.
Article41. Pallwein L, Pinggera G, Schuster AH, Klauser A, Weirich HG, Recheis W, et al. The influence of left renal vein entrapment on outcome after surgical varicocele repair: a color Doppler sonographic demonstration. J Ultrasound Med. 2004; 23:595–601. PMID: 15154525.42. Scultetus AH, Villavicencio JL, Gillespie DL. The nutcracker syndrome: its role in the pelvic venous disorders. J Vasc Surg. 2001; 34:812–819. PMID: 11700480.
Article43. Kim WS, Cheon JE, Kim IO, Kim SH, Yeon KM, Kim KM, et al. Hemodynamic investigation of the left renal vein in pediatric varicocele: Doppler US, venography, and pressure measurements. Radiology. 2006; 241:228–234. PMID: 16908673.
Article44. Barsoum MK, Shepherd RFJ, Welch TJ. Patient with both Wilkie syndrome and nutcracker syndrome. Vasc Med. 2008; 13:247–250. PMID: 18687762.
Article45. Inal M, Unal Daphan B, Karadeniz Bilgili MY. Superior mesenteric artery syndrome accompanying with nutcracker syndrome: a case report. Iran Red Crescent Med J. 2014; 16:e14755. PMID: 25763192.
Article46. Javaid MM, Ong CC, Subramanian S. Blood in urine: a hard nut to crack. Am J Med. 2017; 130:e89–e91. PMID: 27816446.
Article47. Sugimoto I, Ohta T, Ishibashi H, Takeuchi N, Nagata Y, Honda Y. Left renal vein entrapment syndrome (nutcracker syndrome) treated with left renal vein transposition. Jpn J Vasc Surg. 2001; 10:503–507.48. Barnes RW, Fleisher HL 3rd, Redman JF, Smith JW, Harshfield DL, Ferris EJ. Mesoaortic compression of the left renal vein (the so-called nutcracker syndrome): repair by a new stenting procedure. J Vasc Surg. 1988; 8:415–421. PMID: 3172376.
Article49. Shokeir AA, El-Diasty TA, Ghoneim MA. The nutcracker syndrome: new methods of diagnosis and treatment. Br J Urol. 1994; 74:139–143. PMID: 7921927.
Article50. Reed NR, Kalra M, Bower TC, Vrtiska TJ, Ricotta JJ 2nd, Gloviczki P. Left renal vein transposition for nutcracker syndrome. J Vasc Surg. 2009; 49:386–393. PMID: 19216958.
Article51. Xu D, Liu Y, Gao Y, Zhang L, Wang J, Che J, et al. Management of renal nutcracker syndrome by retroperitoneal laparoscopic nephrectomy with ex vivo autograft repair and autotransplantation: a case report and review of the literature. J Med Case Rep. 2009; 3:82. PMID: 19946558.
Article52. Hartung O. Nutcracker syndrome. Phlebolymphology. 2009; 16:246–252.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The role of Doppler ultrasonography in the detection and management of nutcracker syndrome
- Nutcracker Syndrome: Diagnostic Usefulness of Doppler US
- Spontaneous Resolution of Childhood Nutcracker Syndrome
- Superior Mesenteric Artery Syndrome Combined with Renal Nutcracker Syndrome in a Young Male: A Case Report
- A Case of the Nutcracker Syndrome