Korean J Radiol.
2020 Feb;21(2):192-202. 10.3348/kjr.2019.0230.
Coronary Computed Tomography Angiography-Derived Fractional Flow Reserve in Patients with Anomalous Origin of the Right Coronary Artery from the Left Coronary Sinus
- Affiliations
-
- 1Department of Medical Imaging, Jinling Hospital, Medical School of Nanjing University, Nanjing, China. kevinzhlj@163.com
- 2Division of Cardiovascular Imaging, Department of Radiology and Radiological Science, Medical University of South Carolina, Charleston, SC, USA.
- KMID: 2471636
- DOI: http://doi.org/10.3348/kjr.2019.0230
Abstract
OBJECTIVE
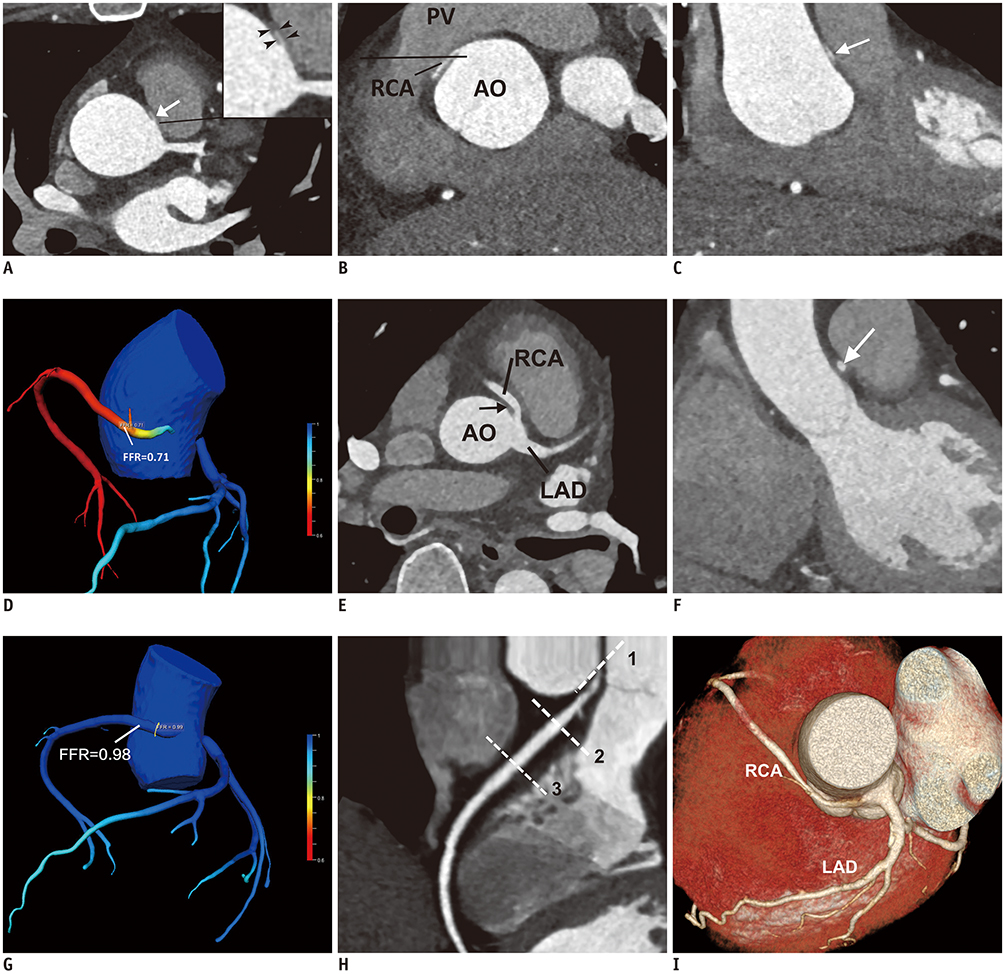
To examine the fractional flow reserve derived from computed tomographic angiography (CT-FFR) in patients with anomalous origin of the right coronary artery from the left coronary sinus (R-ACAOS) with an interarterial course, assess the relationship of CT-FFR with the anatomical features of interarterial R-ACAOS on coronary computed tomographic angiography (CCTA), and determine its clinical relevance.
MATERIALS AND METHODS
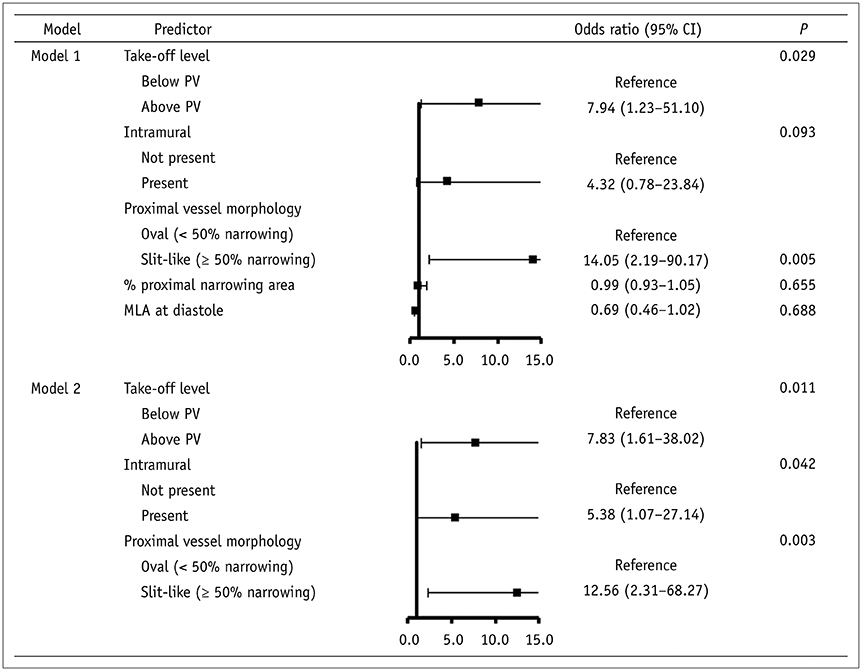
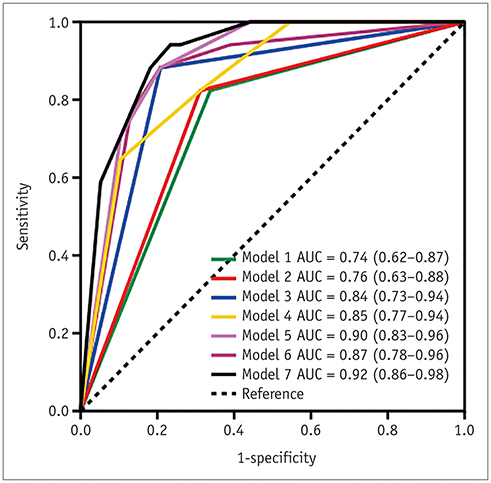
Ninety-four patients with interarterial R-ACAOS undergoing CCTA were retrospectively included. Anatomic features (proximal vessel morphology [oval or slit-like], take-off angle, take-off level [below or above the pulmonary valve], take-off type, intramural course, % proximal narrowing area, length of narrowing, minimum luminal area [MLA] at systole and diastole, and vessel compression index) on CCTA associated with CT-FFR ≤ 0.80 were analyzed. Receiver operating characteristic analysis was performed to describe the diagnostic performance of CT-FFR ≤ 0.80 in detecting interarterial R-ACAOS.
RESULTS
Significant differences were found in proximal vessel morphology, take-off level, intramural course, % proximal narrowing area, and MLA at diastole (all p < 0.05) between the normal and abnormal CT-FFR groups. Take-off level, intramural course, and slit-like ostium (all p < 0.05) predicted hemodynamic abnormality (CT-FFR ≤ 0.80) with accuracies of 0.69, 0.71, and 0.81, respectively. Patients with CT-FFR ≤ 0.80 had a higher prevalence of typical angina (29.4% vs. 7.8%, p = 0.025) and atypical angina (29.4% vs. 6.5%, p = 0.016).
CONCLUSION
Take-off level, intramural course, and slit-like ostium were the main predictors of abnormal CT-FFR values. Importantly, patients with abnormal CT-FFR values showed a higher prevalence of typical angina and atypical angina, indicating that CT-FFR is a potential tool to gauge the clinical relevance in patients with interarterial R-ACAOS.
Keyword
MeSH Terms
Figure
Reference
-
1. Lim JCE, Beale A, Ramcharitar S. Medscape. Anomalous origination of a coronary artery from the opposite sinus. Nat Rev Cardiol. 2011; 8:706–719.
Article2. Angelini P. Novel imaging of coronary artery anomalies to assess their prevalence, the causes of clinical symptoms, and the risk of sudden cardiac death. Circ Cardiovasc Imaging. 2014; 7:747–754.
Article3. Cheezum MK, Liberthson RR, Shah NR, Villines TC, O'Gara PT, Landzberg MJ, et al. Anomalous aortic origin of a coronary artery from the inappropriate sinus of valsalva. J Am Coll Cardiol. 2017; 69:1592–1608.4. Brothers JA, McBride MG, Seliem MA, Marino BS, Tomlinson RS, Pampaloni MH, et al. Evaluation of myocardial ischemia after surgical repair of anomalous aortic origin of a coronary artery in a series of pediatric patients. J Am Coll Cardiol. 2007; 50:2078–2082.
Article5. Agarwal PP, Dennie C, Pena E, Nguyen E, LaBounty T, Yang B, et al. Anomalous coronary arteries that need intervention: review of pre- and postoperative imaging appearances. Radiographics. 2017; 37:740–757.
Article6. Lee HJ, Hong YJ, Kim HY, Lee J, Hur J, Choi BW, et al. Anomalous origin of the right coronary artery from the left coronary sinus with an interarterial course: subtypes and clinical importance. Radiology. 2012; 262:101–108.
Article7. Angelini P, Vidovich MI, Lawless CE, Elayda MA, Lopez JA, Wolf D, et al. Preventing sudden cardiac death in athletes: in search of evidence-based, cost-effective screening. Tex Heart Inst J. 2013; 40:148–155.8. Shi H, Aschoff AJ, Brambs HJ, Hoffmann MH. Multislice CT imaging of anomalous coronary arteries. Eur Radiol. 2004; 14:2172–2181.
Article9. Cheezum MK, Ghoshhajra B, Bittencourt MS, Hulten EA, Bhatt A, Mousavi N, et al. Anomalous origin of the coronary artery arising from the opposite sinus: prevalence and outcomes in patients undergoing coronary CTA. Eur Heart J Cardiovasc Imaging. 2017; 18:224–235.
Article10. Sayar N, Terzi S, Akbulut T, Bilsel T, Ergelen M, Orhan L, et al. Single coronary artery with subsequent coursing of right coronary artery between aorta and pulmonary artery: fractional flow reserve of the anomalous artery guiding the treatment. Int Heart J. 2005; 46:317–322.
Article11. Dimopoulos K, Di Mario C, Barlis P, Pennell D, Goktekin O, Kaddoura S, et al. Haemodynamic significance of an anomalous right coronary with inter-arterial course assessed with intracoronary pressure measurements during dobutamine challenge. Int J Cardiol. 2008; 126:e32–e35.
Article12. Boler AN, Hilliard AA, Gordon BM. Functional assessment of anomalous right coronary artery using fractional flow reserve: an innovative modality to guide patient management. Catheter Cardiovasc Interv. 2017; 89:316–320.13. Lee SE, Yu CW, Park K, Park KW, Suh JW, Cho YS, et al. Physiological and clinical relevance of anomalous right coronary artery originating from left sinus of Valsalva in adults. Heart. 2016; 102:114–119.
Article14. Driesen BW, Warmerdam EG, Sieswerda GT, Schoof PH, Meijboom FJ, Haas F, et al. Anomalous coronary artery originating from the opposite sinus of Valsalva (ACAOS), fractional flow reserve- and intravascular ultrasound-guided management in adult patients. Catheter Cardiovasc Interv. 2018; 92:68–75.
Article15. Benton SM, Tesche C, De Cecco CN, Duguay TM, Schoepf UJ, Bayer RR. Noninvasive derivation of fractional flow reserve from coronary computed tomographic angiography: a review. J Thorac Imaging. 2018; 33:88–96.16. Tesche C, De Cecco CN, Albrecht MH, Duguay TM, Bayer RR 2nd, Litwin SE, et al. Coronary CT angiography-derived fractional flow reserve. Radiology. 2017; 285:17–33.
Article17. Röther J, Moshage M, Dey D, Schwemmer C, Tröbs M, Blachutzik F, et al. Comparison of invasively measured FFR with FFR derived from coronary CT angiography for detection of lesion-specific ischemia: results from a PC-based prototype algorithm. J Cardiovasc Comput Tomogr. 2018; 12:101–107.
Article18. Tesche C, De Cecco CN, Baumann S, Renker M, McLaurin TW, Duguay TM, et al. Coronary CT angiography-derived fractional flow reserve: machine learning algorithm versus computational fluid dynamics modeling. Radiology. 2018; 288:64–72.19. Zimmermann FM, Kobayashi Y, Mullen WL, Fearon WF. Non-invasive FFRCT revealing severe inducible ischaemia in an anomalous right coronary artery. Eur Heart J. 2017; 38:2569.20. Kawaji T, Shiomi H, Shizuta S, Kimura T. Diagnosis of functional ischemia in a right coronary artery with anomalous aortic origin. J Cardiovasc Comput Tomogr. 2016; 10:188–190.
Article21. Fox K, Garcia MA, Ardissino D, Buszman P, Camici PG, Crea F, et al. Task Force on the Management of Stable Angina Pectoris of the European Society of Cardiology. ESC Committee for Practice Guidelines (CPG). Guidelines on the management of stable angina pectoris: executive summary: the task force on the management of stable angina pectoris of the European Society of Cardiology. Eur Heart J. 2006; 27:1341–1381.22. Zhang LJ, Wang Y, Schoepf UJ, Meinel FG, Bayer RR 2nd, Qi L, et al. Image quality, radiation dose, and diagnostic accuracy of prospectively ECG-triggered high-pitch coronary CT angiography at 70 kVp in a clinical setting: comparison with invasive coronary angiography. Eur Radiol. 2016; 26:797–806.23. Nasis A, Machado C, Cameron JD, Troupis JM, Meredith IT, Seneviratne SK. Anatomic characteristics and outcome of adults with coronary arteries arising from an anomalous location detected with coronary computed tomography angiography. Int J Cardiovasc Imaging. 2015; 31:181–191.
Article24. Hlatky MA, De Bruyne B, Pontone G, Patel MR, Norgaard BL, Byrne RA, et al. Quality-of-life and economic outcomes of assessing fractional flow reserve with computed tomography angiography: PLATFORM. J Am Coll Cardiol. 2015; 66:2315–2323.25. Duguay TM, Tesche C, Vliegenthart R, De Cecco CN, Lin H, Albrecht MH, et al. Coronary computed tomographic angiography-derived fractional flow reserve based on machine learning for risk stratification of non-culprit coronary narrowings in patients with acute coronary syndrome. Am J Cardiol. 2017; 120:1260–1266.
Article26. Itu L, Rapaka S, Passerini T, Georgescu B, Schwemmer C, Schoebinger M, et al. A machine-learning approach for computation of fractional flow reserve from coronary computed tomography. J Appl Physiol (1985). 2016; 121:42–52.
Article27. Nørgaard BL, Leipsic J, Gaur S, Seneviratne S, Ko BS, Ito H, et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (analysis of coronary blood flow using CT angiography: next steps). J Am Coll Cardiol. 2014; 63:1145–1155.28. Park EA, Lee W, Park SJ, Kim YK, Hwang HY. Influence of coronary artery diameter on intracoronary transluminal attenuation gradient during CT angiography. JACC Cardiovasc Imaging. 2016; 9:1074–1083.
Article29. Renker M, Schoepf UJ, Wang R, Meinel FG, Rier JD, Bayer RR 2nd, et al. Comparison of diagnostic value of a novel noninvasive coronary computed tomography angiography method versus standard coronary angiography for assessing fractional flow reserve. Am J Cardiol. 2014; 114:1303–1308.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Anomalous Origin of Coronary Artery
- Sudden Death Associated with Anomalous Left Coronary Artery Origin from Right Sinus of Valsalva with Posterior Course
- Anomalous Origin of the Left Circumflex Coronary Artery from the Right Sinus of Valsalva Identified by Imaging with Multidetector Computed Tomography
- Anomalous Right Coronary Artery From the Left Coronary Sinus With an Interarterial Course: Is It Really Dangerous?
- A Case of Acute Myocardial Infarction with the Anomalous Origin of the Right Coronary Artery from the Ascending Aorta above the Left Sinus of Valsalva and Left Coronary Artery from the Posterior Sinus of Valsalva