Pediatr Gastroenterol Hepatol Nutr.
2020 Mar;23(2):137-145. 10.5223/pghn.2020.23.2.137.
Does the Oral-Anal Transit Test Correlate with Colonic Manometry Findings in Children with Refractory Constipation?
- Affiliations
-
- 1Department of Pediatric Gastroenterology, Hepatology, and Nutrition, Atrium Health Levine Children's Hospital, Charlotte, NC, USA. Jason.dranove@yahoo.com
- 2Department of Pediatric Gastroenterology, Children's Mercy Hospital, Kansas City, MO, USA.
- 3Department of Public Health, UNC Gillings School of Global Public Health, Chapel Hill, NC, USA.
- 4Division of Pediatric Surgery, Atrium Health Levine Children's Hospital, Charlotte, NC, USA.
- KMID: 2471623
- DOI: http://doi.org/10.5223/pghn.2020.23.2.137
Abstract
- PURPOSE
The Oral-anal Transit Test (OTT) is a simple method of obtaining information about colonic transit. We aim to assess the correlation of OTT with the neuromuscular integrity of the colon determined by colonic manometry (CM).
METHODS
All patients who had OTT followed by CM were evaluated. Less than 6 of 24 markers remaining on OTT was considered normal. CM was performed per previously published guidelines. A normal CM was defined as at least one High Amplitude Propagating Contraction progressing from the most proximal sensor through the sigmoid colon.
RESULTS
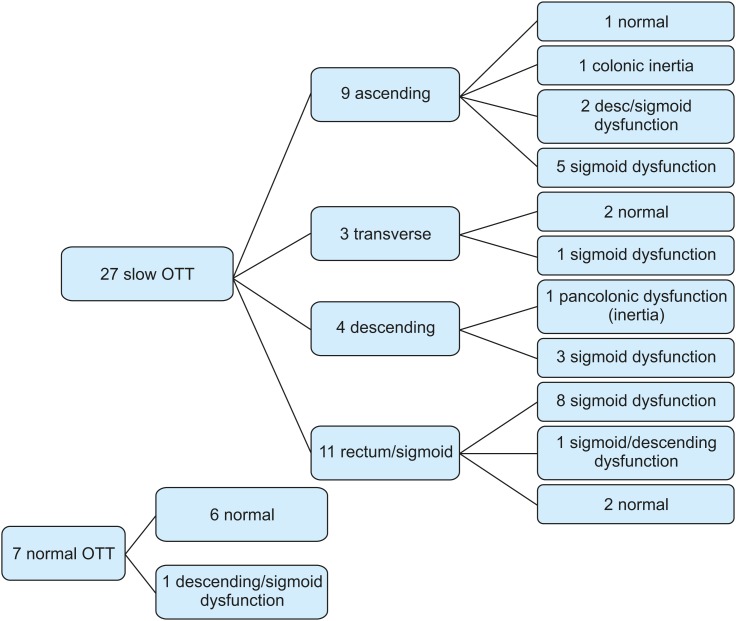
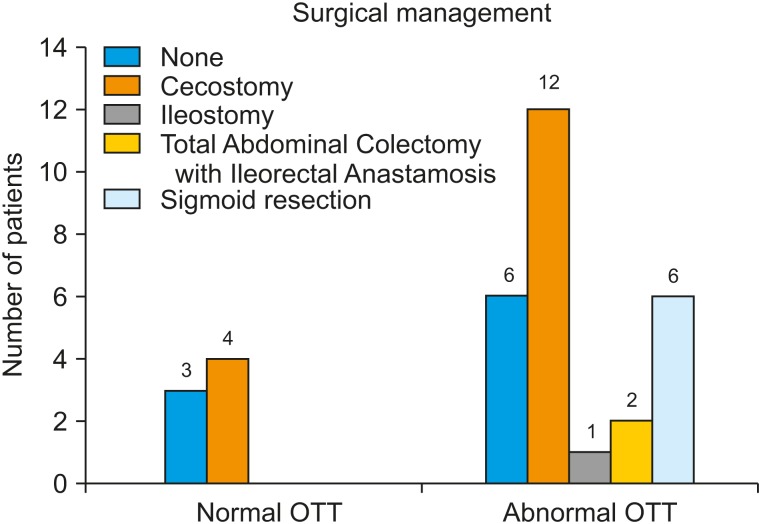
A total of 34 patients underwent both OTT and CM (44% male, age 4-18 years, mean 11.5 years, 97% functional constipation +/− soiling, Hirschsprung's Disease). Of normal and abnormal OTT patients, 85.7% (6/7) and 18.5% (5/27) respectively had normal CM. When all markers progressed to at least the sigmoid colon, this was 100% predictive against colonic inertia. Greater than 50% of patients with manometric isolated sigmoid dysfunction had markers proximal to the recto-sigmoid.
CONCLUSION
OTT and CM are both valuable studies that assess different aspects of colonic function. OTT can be used as a screening test to rule out colonic inertia. However, the most proximal extent of remaining markers does not predict the anatomical extent of the manometric abnormality, particularly in isolated sigmoid dysfunction.
Keyword
MeSH Terms
Figure
Reference
-
1. Wood RJ, Yacob D, Levitt MA. Surgical options for the management of severe functional constipation in children. Curr Opin Pediatr. 2016; 28:370–379. PMID: 26963948.
Article2. Tabbers MM, DiLorenzo C, Berger MY, Faure C, Langendam MW, Nurko S, et al. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. North American Society for Pediatric Gastroenterology. Evaluation and treatment of functional constipation in infants and children: evidence-based recommendations from ESPGHAN and NASPGHAN. J Pediatr Gastroenterol Nutr. 2014; 58:258–274. PMID: 24345831.3. Koppen IJ, Di Lorenzo C, Saps M, Dinning PG, Yacob D, Levitt MA, et al. Childhood constipation: finally something is moving! Expert Rev Gastroenterol Hepatol. 2016; 10:141–155. PMID: 26466201.
Article4. Rodriguez L, Sood M, Di Lorenzo C, Saps M. An ANMS-NASPGHAN consensus document on anorectal and colonic manometry in children. Neurogastroenterol Motil. 2017; 29.
Article5. Rao SS, Camilleri M, Hasler WL, Maurer AH, Parkman HP, Saad R, et al. Evaluation of gastrointestinal transit in clinical practice: position paper of the American and European Neurogastroenterology and Motility Societies. Neurogastroenterol Motil. 2011; 23:8–23. PMID: 21138500.
Article6. Koppen IJ, Kuizenga-Wessel S, Lu PL, Benninga MA, Di Lorenzo C, Lane VA, et al. Surgical decision-making in the management of children with intractable functional constipation: what are we doing and are we doing it right? J Pediatr Surg. 2016; 51:1607–1612. PMID: 27329390.
Article7. Gasior A, Reck C, Vilanova-Sanchez A, Diefenbach KA, Yacob D, Lu P, et al. Surgical management of functional constipation: an intermediate report of a new approach using a laparoscopic sigmoid resection combined with malone appendicostomy. J Pediatr Surg. 2018; 53:1160–1162. PMID: 29588075.
Article8. Tipnis NA, El-Chammas KI, Rudolph CD, Werlin SL, Sood MR. Do oro-anal transit markers predict which children would benefit from colonic manometry studies? J Pediatr Gastroenterol Nutr. 2012; 54:258–262. PMID: 21734599.
Article9. Bharucha AE. High amplitude propagated contractions. Neurogastroenterol Motil. 2012; 24:977–982. PMID: 23057554.
Article10. Siddiqui AA, Fishman SJ, Bauer SB, Nurko S. Long-term follow-up of patients after antegrade continence enema procedure. J Pediatr Gastroenterol Nutr. 2011; 52:574–580. PMID: 21502828.
Article11. Siminas S, Losty PD. Current surgical management of pediatric idiopathic constipation: a systematic review of published studies. Ann Surg. 2015; 262:925–933. PMID: 25775070.12. Sood MR, Mousa H, Tipnis N, Di Lorenzo C, Werlin S, Fernandez S, et al. Interobserver variability in the interpretation of colon manometry studies in children. J Pediatr Gastroenterol Nutr. 2012; 55:548–551. PMID: 22465932.
Article13. Kuizenga-Wessel S, Mousa HM, Benninga MA, Di Lorenzo C. Lack of agreement on how to use antegrade enemas in children. J Pediatr Gastroenterol Nutr. 2016; 62:71–79. PMID: 26192697.
Article14. Abrahamsson H, Antov S, Bosaeus I. Gastrointestinal and colonic segmental transit time evaluated by a single abdominal x-ray in healthy subjects and constipated patients. Scand J Gastroenterol Suppl. 1988; 152(152 sup152):72–80. PMID: 3254616.
Article15. Chaussade S, Khyari A, Roche H, Garret M, Gaudric M, Couturier D, et al. Determination of total and segmental colonic transit time in constipated patients. Results in 91 patients with a new simplified method. Dig Dis Sci. 1989; 34:1168–1172. PMID: 2546720.16. Giorgio V, Borrelli O, Smith VV, Rampling D, Köglmeier J, Shah N, et al. High-resolution colonic manometry accurately predicts colonic neuromuscular pathological phenotype in pediatric slow transit constipation. Neurogastroenterol Motil. 2013; 25:70–8.e8-9. PMID: 23030503.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usefulness of Colonic Transit Time Measurement in Chronic Constipation
- Comparison of Anorectal Function Tests according to the Types of Colon Transit Time in Patients with Chronic Idiopathic Constipation
- How to Perform and Assess Colonic Manometry and Barostat Study in Chronic Constipation
- Colonic Transit Time in Chronic Constipated Patients
- Regional Colonic Transit Pattern Does Not Conclusively Identify Evacuation Disorders in Constipated Patients with Delayed Colonic Transit