Hip Pelvis.
2020 Mar;32(1):17-25. 10.5371/hp.2020.32.1.17.
Midterm-clinical Outcomes after Hip Arthroscopy in Middle-aged Patients with Early Osteoarthritis
- Affiliations
-
- 1Department of Orthopaedic Surgery, Chungnam National University School of Medicine, Daejeon, Korea. dshwang@cnu.ac.kr
- 2Department of Orthopaedic Surgery, Yanbian University Hospital, Yanji, China.
- KMID: 2471127
- DOI: http://doi.org/10.5371/hp.2020.32.1.17
Abstract
- PURPOSE
Although the number of hip arthroscopies is rapidly increasing in non-elderly patients, outcomes of this procedure in middle-aged patients are not well documented or clearly understood. The purpose of this study was to evaluate the clinical and radiological outcomes after hip arthroscopy in middle-aged patients with early osteoarthritis.
MATERIALS AND METHODS
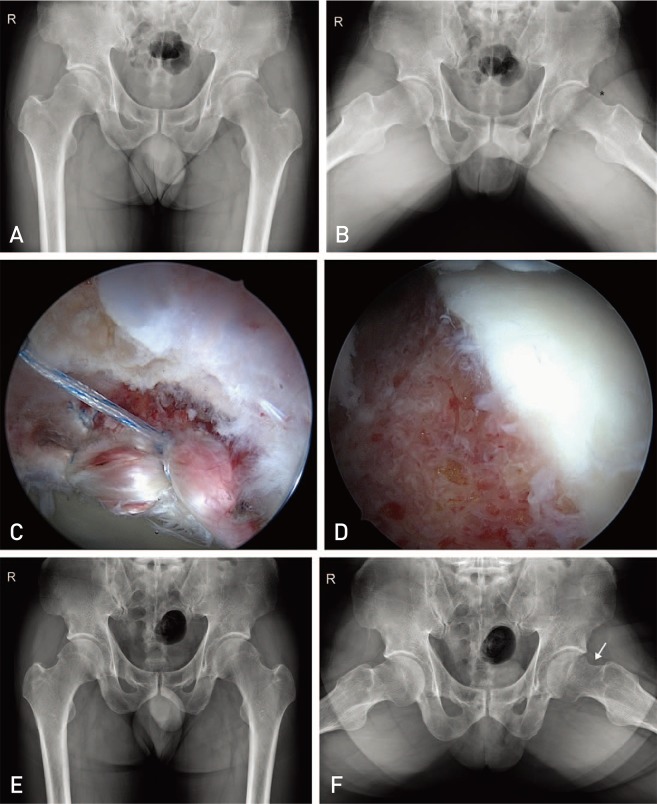
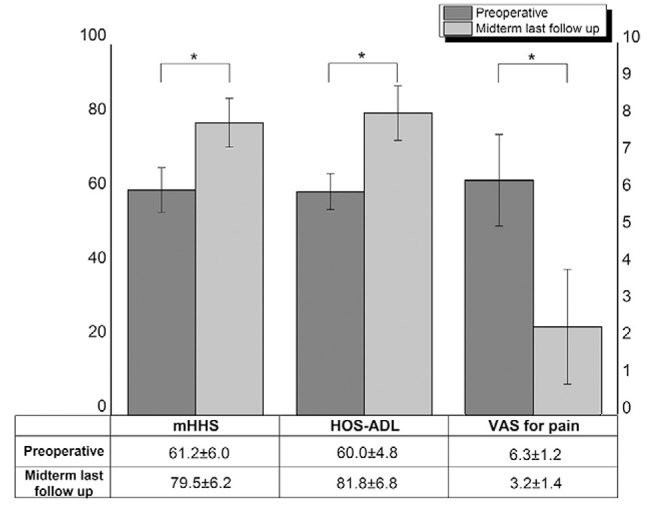
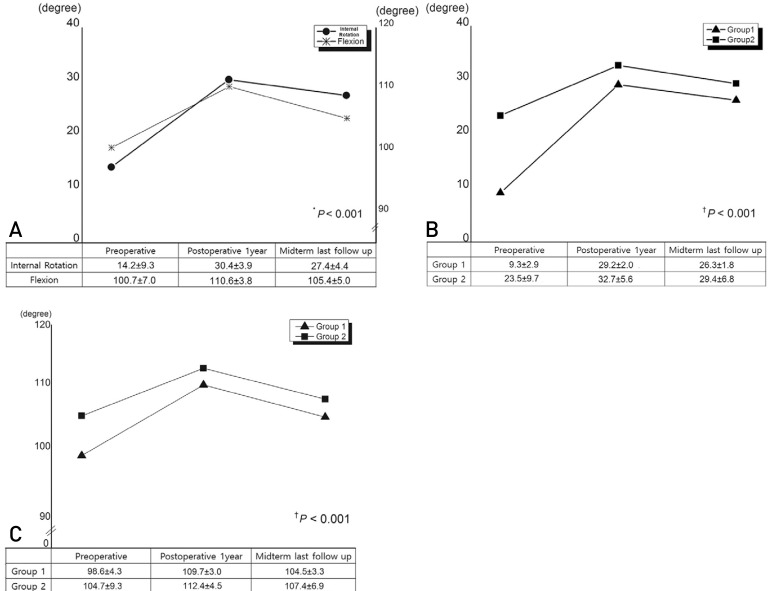
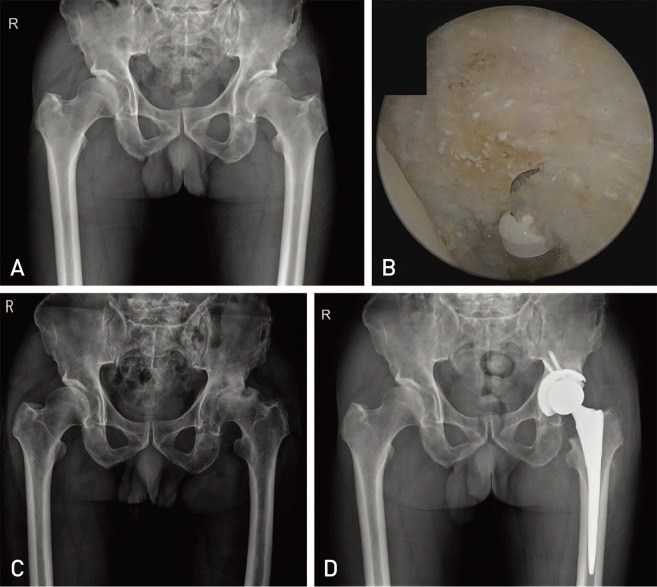
This retrospective study analyzed 189 patients with early osteoarthritis of various diagnoses aged 40 years or older who underwent hip arthroscopy between January 2010 and December 2015. Clinical (e.g., modified Harris hip score [mHHS], hip outcome score-activities of daily living [HOS-ADL], visual analogue scale [VAS] for pain, range of motion) and radiological (change of Tönnis grade) outcomes were assessed at a minimum of 3-year follow-up.
RESULTS
The mean preoperative and final mHHS and HOS-ADL improved from 61.2 and 60.6 to 79.5 and 81.8, respectively, while the VAS pain score decreased from 6.3 to 3.2 (P<0.001). Although the mean range of internal rotation and flexion increased from 14.2 and 100.7° preoperatively to 30.4 and 110.6° at 1-year postoperatively, they decreased slightly to 27.4 and 105.4° at the final follow-up, respectively. Eight cases (4.2%) underwent revision arthroscopic surgery and three cases (1.6%) were converted to total hip arthroplasty.
CONCLUSION
Patients with early-stage osteoarthritis of various diagnoses achieved improved clinical outcomes. Therefore, using hip arthroscopy in middle-aged patients with early osteoarthritis, it is possible to achieve good surgical options.
MeSH Terms
Figure
Reference
-
1. Danielsson L, Lindberg H. Prevalence of coxarthrosis in an urban population during four decades. Clin Orthop Relat Res. 1997; (342):106–110.
Article2. Sing DC, Feeley BT, Tay B, Vail TP, Zhang AL. Age-related trends in hip arthroscopy: a large cross-sectional analysis. Arthroscopy. 2015; 31:2307–2313.e2. PMID: 26194938.
Article3. Montgomery SR, Ngo SS, Hobson T, et al. Trends and demographics in hip arthroscopy in the United States. Arthroscopy. 2013; 29:661–665. PMID: 23375668.
Article4. Schairer WW, Nwachukwu BU, McCormick F, Lyman S, Mayman D. Use of hip arthroscopy and risk of conversion to total hip arthroplasty: a population-based analysis. Arthroscopy. 2016; 32:587–593. PMID: 26671201.
Article5. Lee JW, Hwang DS, Kang C, Hwang JM, Chung HJ. Arthroscopic repair of acetabular labral tears associated with femoroacetabular impingement: 7-10 years of long-term follow-up results. Clin Orthop Surg. 2019; 11:28–35. PMID: 30838105.
Article6. Philippon MJ, Ejnisman L, Ellis HB, Briggs KK. Outcomes 2 to 5 years following hip arthroscopy for femoroacetabular impingement in the patient aged 11 to 16 years. Arthroscopy. 2012; 28:1255–1261. PMID: 22560486.
Article7. Jayakumar P, Ramachandran M, Youm T, Achan P. Arthroscopy of the hip for paediatric and adolescent disorders: current concepts. J Bone Joint Surg Br. 2012; 94:290–296. PMID: 22371532.8. Byrd JW, Jones KS. Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2009; 467:739–746. PMID: 19096902.
Article9. Suarez-Ahedo C, Gui C, Rabe SM, Walsh JP, Chandrasekaran S, Domb BG. Relationship between age at onset of symptoms and intraoperative findings in hip arthroscopic surgery. Orthop J Sports Med. 2017; 5:2325967117737480. PMID: 29226162.
Article10. Herrmann SJ, Bernauer M, Erdle B, Südkamp NP, Helwig P, Hauschild O. Osteoarthritic changes rather than age predict outcome following arthroscopic treatment of femoroacetabular impingement in middle-aged patients. BMC Musculoskelet Disord. 2016; 17:253. PMID: 27278243.
Article11. Wilkin G, March G, Beaulé PE. Arthroscopic acetabular labral debridement in patients forty-five years of age or older has minimal benefit for pain and function. J Bone Joint Surg Am. 2014; 96:113–118. PMID: 24430410.
Article12. Javed A, O'Donnell JM. Arthroscopic femoral osteochondroplasty for cam femoroacetabular impingement in patients over 60 years of age. J Bone Joint Surg Br. 2011; 93:326–331. PMID: 21357953.
Article13. Kim KC, Hwang DS, Lee CH, Kwon ST. Influence of femoroacetabular impingement on results of hip arthroscopy in patients with early osteoarthritis. Clin Orthop Relat Res. 2007; 456:128–132. PMID: 17106273.
Article14. Griffin DW, Kinnard MJ, Formby PM, McCabe MP, Anderson TD. Outcomes of hip arthroscopy in the older adult: a systematic review of the literature. Am J Sports Med. 2017; 45:1928–1936. PMID: 27756723.
Article15. Piuzzi NS, Slullitel PA, Bertona A, et al. Hip arthroscopy in osteoarthritis: a systematic review of the literature. Hip Int. 2016; 26:8–14.
Article16. Kemp JL, MacDonald D, Collins NJ, Hatton AL, Crossley KM. Hip arthroscopy in the setting of hip osteoarthritis: systematic review of outcomes and progression to hip arthroplasty. Clin Orthop Relat Res. 2015; 473:1055–1073. PMID: 25231154.
Article17. Griffin DR, Dickenson EJ, O'Donnell J, et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med. 2016; 50:1169–1176. PMID: 27629403.18. Hoaglund FT, Steinbach LS. Primary osteoarthritis of the hip: etiology and epidemiology. J Am Acad Orthop Surg. 2001; 9:320–327. PMID: 11575911.
Article19. Lodhia P, Slobogean GP, Noonan VK, Gilbart MK. Patient-reported outcome instruments for femoroacetabular impingement and hip labral pathology: a systematic review of the clinimetric evidence. Arthroscopy. 2011; 27:279–286. PMID: 21035994.
Article20. Byrd JW. Evaluation of the hip: history and physical examination. N Am J Sports Phys Ther. 2007; 2:231–240. PMID: 21509142.21. Stelzeneder D, Mamisch TC, Kress I, et al. Patterns of joint damage seen on MRI in early hip osteoarthritis due to structural hip deformities. Osteoarthritis Cartilage. 2012; 20:661–669. PMID: 22469848.
Article22. Horisberger M, Brunner A, Herzog RF. Arthroscopic treatment of femoral acetabular impingement in patients with preoperative generalized degenerative changes. Arthroscopy. 2010; 26:623–629. PMID: 20434659.
Article23. Capogna BM, Ryan MK, Begly JP, Chenard KE, Mahure SA, Youm T. Clinical outcomes of hip arthroscopy in patients 60 or older: a minimum of 2-year follow-up. Arthroscopy. 2016; 32:2505–2510. PMID: 27544591.24. Domb BG, Chaharbakhshi EO, Rybalko D, Close MR, Litrenta J, Perets I. Outcomes of hip arthroscopic surgery in patients with Tönnis grade 1 osteoarthritis at a minimum 5-year follow-up: a matched-pair comparison with a Tönnis grade 0 control group. Am J Sports Med. 2017; 45:2294–2302. PMID: 28609644.
Article25. Chandrasekaran S, Gui C, Darwish N, Lodhia P, Suarez-Ahedo C, Domb BG. Outcomes of hip arthroscopic surgery in patients with Tönnis grade 1 osteoarthritis with a minimum 2-year follow-up: evaluation using a matched-pair analysis with a control group with Tönnis grade 0. Am J Sports Med. 2016; 44:1781–1788. PMID: 27045086.26. Egerton T, Hinman RS, Takla A, Bennell KL, O'Donnell J. Intraoperative cartilage degeneration predicts outcome 12 months after hip arthroscopy. Clin Orthop Relat Res. 2013; 471:593–599. PMID: 22992870.
Article27. Philippon MJ, Schroder E Souza BG, Briggs KK. Hip arthroscopy for femoroacetabular impingement in patients aged 50 years or older. Arthroscopy. 2012; 28:59–65. PMID: 21982390.
Article28. Philippon MJ, Briggs KK, Carlisle JC, Patterson DC. Joint space predicts THA after hip arthroscopy in patients 50 years and older. Clin Orthop Relat Res. 2013; 471:2492–2496. PMID: 23292888.
Article29. Bedi A, Dolan M, Hetsroni I, et al. Surgical treatment of femoroacetabular impingement improves hip kinematics: a computer-assisted model. Am J Sports Med. 2011; 39:43S–49S. PMID: 21709031.30. Ross JR, Larson CM, Adeoye O, Kelly BT, Bedi A. Residual deformity is the most common reason for revision hip arthroscopy: a three-dimensional CT study. Clin Orthop Relat Res. 2015; 473:1388–1395. PMID: 25475714.
Article31. Philippon MJ, Schenker ML, Briggs KK, Kuppersmith DA, Maxwell RB, Stubbs AJ. Revision hip arthroscopy. Am J Sports Med. 2007; 35:1918–1921. PMID: 17703000.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Application of Hip Arthroscopy in Degenerative Osteoarthritis
- Comprehensive Review of Advancements in Hip Arthroscopy
- Arthroscopy of the Hip Joint: Diagnosis and Treatment
- Hip Arthroscopy for Incarcerated Acetabular Labrum following Reduction of Traumatic Hip Dislocation: Three Case Reports
- The Usefulness of Hip Arthroscopy