Hip Pelvis.
2020 Mar;32(1):1-10. 10.5371/hp.2020.32.1.1.
Three-dimensional-printing Technology in Hip and Pelvic Surgery: Current Landscape
- Affiliations
-
- 1Department of Orthopedic Surgery, Center for Joint Disease, Chonnam National University Hwasun Hospital, Hwasun, Korea. tryoon@chonnam.ac.kr
- KMID: 2471125
- DOI: http://doi.org/10.5371/hp.2020.32.1.1
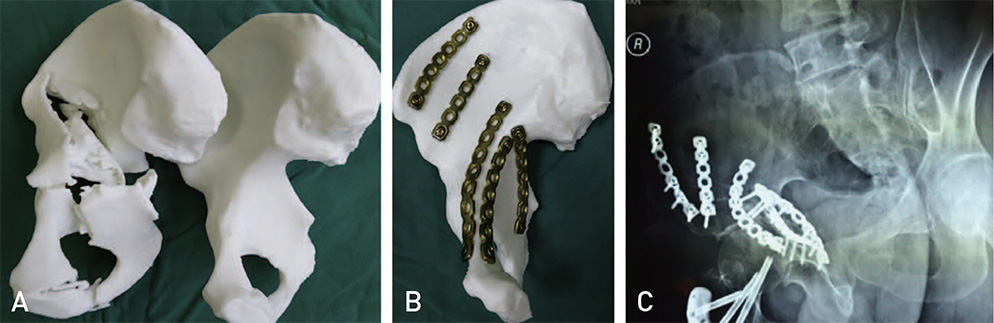
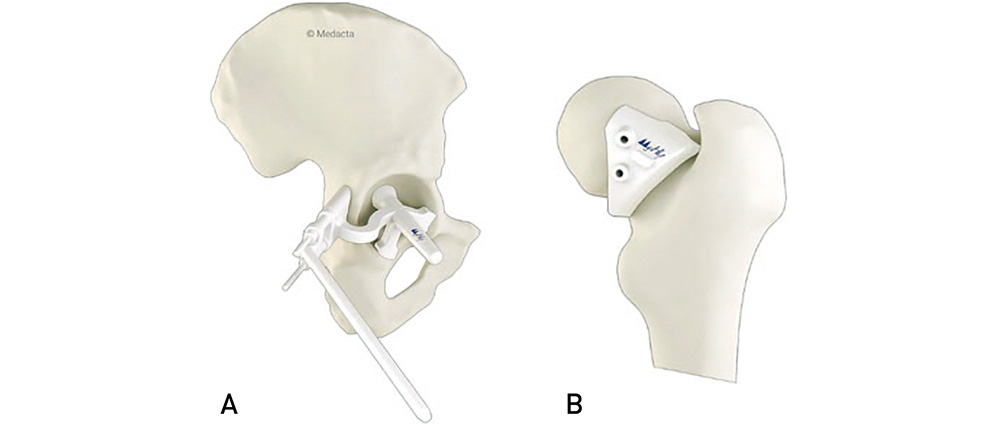
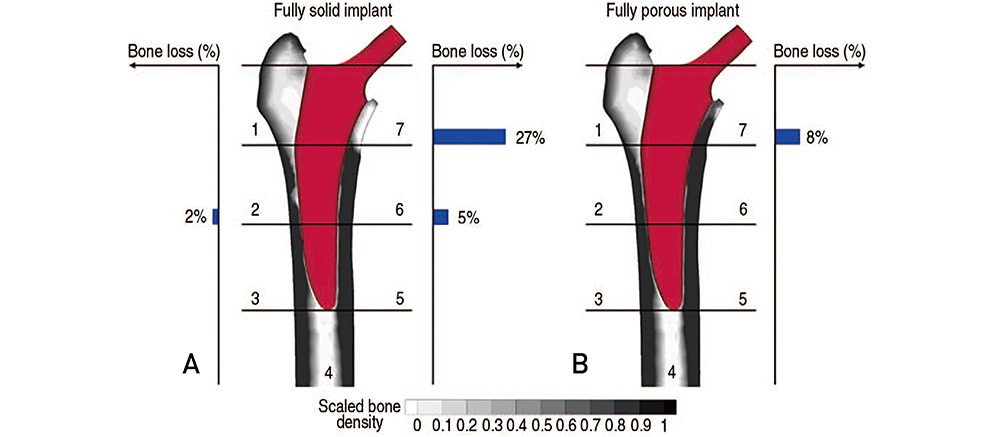
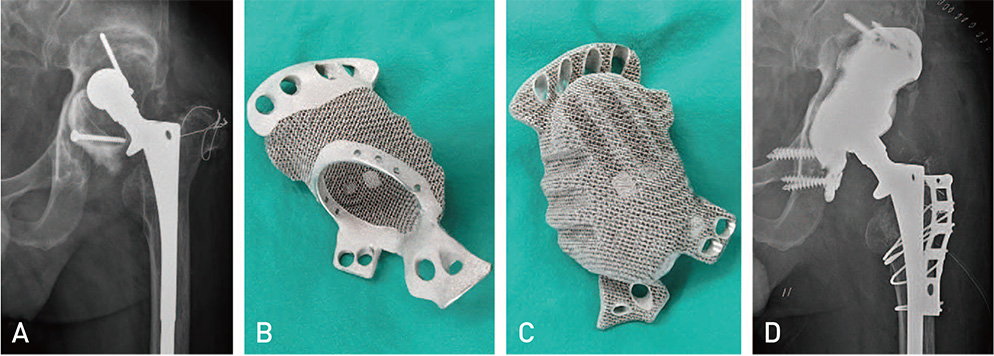
Abstract
- The use of three-dimensional (3D) printing is becoming more common, including in the field of orthopaedic surgery. There are currently four primary clinical applications for 3D-printing in hip and pelvic surgeries: (i) 3D-printed anatomical models for planning and surgery simulation, (ii) patient-specific instruments (PSI), (iii) generation of prostheses with 3D-additive manufacturing, and (iv) custom 3D-printed prostheses. Simulation surgery using a 3D-printed bone model allows surgeons to develop better surgical approaches, test the feasibility of procedures and determine optimal location and size for a prosthesis. PSI will help inform accurate bone cuts and prosthesis placement during surgery. Using 3D-additive manufacturing, especially with a trabecular pattern, is possible to produce a prosthesis mechanically stable and biocompatible prosthesis capable of promoting osseointergration. Custom implants are useful in patients with massive acetabular bone loss or periacetabular malignant bone tumors as they may improve the fit between implants and patient-specific anatomy. 3D-printing technology can improve surgical efficiency, shorten operation times and reduce exposure to radiation. This technology also offers new potential for treating complex hip joint diseases. Orthopaedic surgeons should develop guidelines to outline the most effective uses of 3D-printing technology to maximize patient benefits.
Keyword
Figure
Reference
-
1. Hegde A. Healthcare 3D printing market 2018 prominent players - Aprecia pharmaceuticals, Aspect Biosystems, Bio 3D Technologies, BioBots, Cyfuse Biomedical, Digilab, 3Dynamics Systems, Envision TEC, Luxexcel, Materialise NV, Nano3D Biosciences, Oceanz, Organovo Ho [Internet]. Cleveland (OH): Global Market Insights, Inc.;2018. 08. 03. cited 2019 Oct 18. Available from: https://www.openpr.com/news/1160692/healthcare-3d-printing-market-2018-prominent-players-aprecia-pharmaceuticals-aspect-biosystemsbio-3d-technologies-biobots-cyfuse-biomedical-digilab-3dynamics-systems-envision-tec-luxexcel-materialise-nvnano3d-biosciences-oceanz-organovo-ho.html.2. Ventola CL. Medical applications for 3D printing: current and projected uses. Pharm Ther. 2014; 39:704–711.3. Xia RZ, Zhai ZJ, Chang YY, Li HW. Clinical applications of 3-dimensional printing technology in hip joint. Orthop Surg. 2019; 11:533–544.
Article4. Baauw M, van Hellemondt GG, van Hooff ML, Spruit M. The accuracy of positioning of a custom-made implant within a large acetabular defect at revision arthroplasty of the hip. Bone Joint J. 2015; 97:780–785.
Article5. Shin JK, Son SM, Kim TW, Shin WC, Lee JS, Suh KT. Accuracy and reliability of preoperative on-screen templating using digital radiographs for total hip arthroplasty. Hip Pelvis. 2016; 28:201–207.
Article6. Zheng SN, Yao QQ, Mao FY, et al. Application of 3D printing rapid prototyping-assisted percutaneous fixation in the treatment of intertrochanteric fracture. Exp Ther Med. 2017; 14:3644–3650.
Article7. Yu AW, Duncan JM, Daurka JS, Lewis A, Cobb J. A feasibility study into the use of three-dimensional printer modelling in acetabular fracture surgery. Adv Orthop. 2015; 2015:617046.
Article8. Chen K, Yang F, Yao S, et al. Application of computer-assisted virtual surgical procedures and three-dimensional printing of patient-specific pre-contoured plates in bicolumnar acetabular fracture fixation. Orthop Traumatol Surg Res. 2019; 105:877–884.
Article9. Won SH, Lee YK, Ha YC, Suh YS, Koo KH. Improving pre-operative planning for complex total hip replacement with a Rapid Prototype model enabling surgical simulation. Bone Joint J. 2013; 95:1458–1463.
Article10. Xu J, Li D, Ma RF, Barden B, Ding Y. Application of rapid prototyping pelvic model for patients with DDH to facilitate arthroplasty planning: a pilot study. J Arthroplasty. 2015; 30:1963–1970.
Article11. Faur C, Crainic N, Sticlaru C, Oancea C. Rapid prototyping technique in the preoperative planning for total hip arthroplasty with custom femoral components. Wien Klin Wochenschr. 2013; 125:144–149.
Article12. Verma T, Mishra A, Agarwal G, Maini L. Application of three dimensional printing in surgery for cam type of femoro-acetabular impingement. J Clin Orthop Trauma. 2018; 9:241–246.
Article13. Li B, Lei P, Liu H, et al. Clinical value of 3D printing guide plate in core decompression plus porous bioceramics rod placement for the treatment of early osteonecrosis of the femoral head. J Orthop Surg Res. 2018; 13:130.
Article14. Henckel J, Holme TJ, Radford W, Skinner JA, Hart AJ. 3D-printed patient-specific guides for hip arthroplasty. J Am Acad Orthop Surg. 2018; 26:e342–e348.
Article15. Small T, Krebs V, Molloy R, Bryan J, Klika AK, Barsoum WK. Comparison of acetabular shell position using patient specific instruments vs. standard surgical instruments: a randomized clinical trial. J Arthroplasty. 2014; 29:1030–1037.
Article16. Ohldin P. Series production of CE-certified orthopedic implants with integrated porous structures for improved bone ingrowth [Internet]. Vienna: Annals of DAAAM & Proceedings;2010. cited 2019 Sep 27. Available from: http://connection.ebscohost.com/c/articles/55675250/series-production-cecertified-orthopedic-implants-integrated-porous-structuresimproved-bone-ingrowth.17. Regis M, Marin E, Fedrizzi L, Pressacco M. Additive manufacturing of Trabecular Titanium orthopedic implants. MRS Bull. 2015; 40:137–144.
Article18. Taniguchi N, Fujibayashi S, Takemoto M, et al. Effect of pore size on bone ingrowth into porous titanium implants fabricated by additive manufacturing: an in vivo experiment. Mater Sci Eng C Mater Biol Appl. 2016; 59:690–701.
Article19. Asti A, Gastaldi G, Dorati R, et al. Stem cells grown in osteogenic medium on PLGA, PLGA/HA, and titanium scaffolds for surgical applications. Bioinorg Chem Appl. 2010; 2010:831031.
Article20. Castagnini F, Bordini B, Stea S, Calderoni PP, Masetti C, Busanelli L. Highly porous titanium cup in cementless total hip arthroplasty: registry results at eight years. Int Orthop. 2019; 43:1815–1821.
Article21. Arabnejad S, Johnston B, Tanzer M, Pasini D. Fully porous 3D printed titanium femoral stem to reduce stress-shielding following total hip arthroplasty. J Orthop Res. 2017; 35:1774–1783.
Article22. Rengier F, Mehndiratta A, von Tengg-Kobligk H, et al. 3D printing based on imaging data: review of medical applications. Int J Comput Assist Radiol Surg. 2010; 5:335–341.
Article23. Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994; 9:33–44.
Article24. Berry DJ, Lewallen DG, Hanssen AD, Cabanela ME. Pelvic discontinuity in revision total hip arthroplasty. J Bone Joint Surg Am. 1999; 81:1692–1702.
Article25. Abolghasemian M, Tangsataporn S, Sternheim A, Backstein D, Safir O, Gross AE. Combined trabecular metal acetabular shell and augment for acetabular revision with substantial bone loss: a mid-term review. Bone Joint J. 2013; 95:166–172.26. Banerjee S, Issa K, Kapadia BH, Pivec R, Khanuja HS, Mont MA. Systematic review on outcomes of acetabular revisions with highly-porous metals. Int Orthop. 2014; 38:689–702.
Article27. Beckmann NA, Weiss S, Klotz MC, Gondan M, Jaeger S, Bitsch RG. Loosening after acetabular revision: comparison of trabecular metal and reinforcement rings. A systematic review. J Arthroplasty. 2014; 29:229–235.
Article28. Sculco PK, Ledford CK, Hanssen AD, Abdel MP, Lewallen DG. The evolution of the cup-cage technique for major acetabular defects: full and half cup-cage reconstruction. J Bone Joint Surg Am. 2017; 99:1104–1110.29. Barlow BT, Oi KK, Lee YY, Carli AV, Choi DS, Bostrom MP. Outcomes of custom flange acetabular components in revision total hip arthroplasty and predictors of failure. J Arthroplasty. 2016; 31:1057–1064.
Article30. Moore KD, McClenny MD, Wills BW. Custom triflange acetabular components for large acetabular defects: minimum 10-year follow-up. Orthopedics. 2018; 41:e316–e320.
Article31. Myncke I, van Schaik D, Scheerlinck T. Custom-made triflanged acetabular components in the treatment of major acetabular defects. Short-term results and clinical experience. Acta Orthop Belg. 2017; 83:341–350.32. Colen S, Harake R, De Haan J, Mulier M. A modified custommade triflanged acetabular reconstruction ring (MCTARR) for revision hip arthroplasty with severe acetabular defects. Acta Orthop Belg. 2013; 79:71–75.33. DeBoer DK, Christie MJ, Brinson MF, Morrison JC. Revision total hip arthroplasty for pelvic discontinuity. J Bone Joint Surg Am. 2007; 89:835–840.
Article34. Wind MA Jr, Swank ML, Sorger JI. Short-term results of a custom triflange acetabular component for massive acetabular bone loss in revision THA. Orthopedics. 2013; 36:e260–e265.
Article35. Taunton MJ, Fehring TK, Edwards P, Bernasek T, Holt GE, Christie MJ. Pelvic discontinuity treated with custom triflange component: a reliable option. Clin Orthop Relat Res. 2012; 470:428–434.
Article36. De Martino I, Strigelli V, Cacciola G, Gu A, Bostrom MP, Sculco PK. Survivorship and clinical outcomes of custom triflange acetabular components in revision total hip arthroplasty: a systematic review. J Arthroplasty. 2019; 34:2511–2518.
Article37. Carter SR, Eastwood DM, Grimer RJ, Sneath RS. Hindquarter amputation for tumours of the musculoskeletal system. J Bone Joint Surg Br. 1990; 72:490–493.
Article38. Ayvaz M, Bekmez S, Mermerkaya MU, Caglar O, Acaroglu E, Tokgozoglu AM. Long-term results of reconstruction with pelvic allografts after wide resection of pelvic sarcomas. ScientificWorldJournal. 2014; 2014:605019.
Article39. Puri A, Gulia A, Pruthi M. Outcome of surgical resection of pelvic osteosarcoma. Indian J Orthop. 2014; 48:273–278.
Article40. Zang J, Guo W, Yang Y, Xie L. Reconstruction of the hemipelvis with a modular prosthesis after resection of a primary malignant peri-acetabular tumour involving the sacroiliac joint. Bone Joint J. 2014; 96:399–405.
Article41. Sun W, Li J, Li Q, Li G, Cai Z. Clinical effectiveness of hemipelvic reconstruction using computer-aided custom-made prostheses after resection of malignant pelvic tumors. J Arthroplasty. 2011; 26:1508–1513.
Article42. Chen X, Xu L, Wang Y, Hao Y, Wang L. Image-guided installation of 3D-printed patient-specific implant and its application in pelvic tumor resection and reconstruction surgery. Comput Methods Programs Biomed. 2016; 125:66–78.
Article43. Wong KC, Kumta SM, Geel NV, Demol J. One-step reconstruction with a 3D-printed, biomechanically evaluated custom implant after complex pelvic tumor resection. Comput Aided Surg. 2015; 20:14–23.
Article44. Liang H, Ji T, Zhang Y, Wang Y, Guo W. Reconstruction with 3D-printed pelvic endoprostheses after resection of a pelvic tumour. Bone Joint J. 2017; 99:267–275.
Article45. Wang B, Hao Y, Pu F, Jiang W, Shao Z. Computer-aided designed, three dimensional-printed hemipelvic prosthesis for peri-acetabular malignant bone tumour. Int Orthop. 2018; 42:687–694.
Article46. Hughes AJ, DeBuitleir C, Soden P, et al. 3D printing aids acetabular reconstruction in complex revision hip arthroplasty. Adv Orthop. 2017; 2017:8925050.
Article47. Li CS, Vannabouathong C, Sprague S, Bhandari M. The use of carbon-fiber-reinforced (CFR) PEEK material in orthopedic implants: a systematic review. Clin Med Insights Arthritis Musculoskelet Disord. 2015; 8:33–45.
Article48. Kersten RF, van Gaalen SM, de Gast A, Öner FC. Polyetheretherketone (PEEK) cages in cervical applications: a systematic review. Spine J. 2015; 15:1446–1460.
Article49. Wong KC. 3D-printed patient-specific applications in orthopedics. Orthop Res Rev. 2016; 8:57–66.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Three-Dimensional Printing Technology in Orthopedic Surgery
- 3-Dimensional Printing for Hip Surgery: Current Landscape and Future Perspectives
- Application of Three-Dimensional Printing in the Fracture Management
- A Review of Current Clinical Applications of Three-Dimensional Printing in Spine Surgery
- Clinical Application of Three-Dimensional Printing Technology in Craniofacial Plastic Surgery