Korean J Radiol.
2020 Mar;21(3):259-267. 10.3348/kjr.2019.0695.
Annual Trends in Ultrasonography-Guided 14-Gauge Core Needle Biopsy for Breast Lesions
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiological Science, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. ekkim@yuhs.ac
- 2Department of Radiology and Research Institute of Radiological Science, Yonsei Biomedical Research Institute, Seoul, Korea.
- KMID: 2470749
- DOI: http://doi.org/10.3348/kjr.2019.0695
Abstract
OBJECTIVE
To examine time trends in ultrasonography (US)-guided 14-gauge core needle biopsy (CNB) for breast lesions based on the lesion size, Breast Imaging-Reporting and Data System (BI-RADS) category, and pathologic findings.
MATERIALS AND METHODS
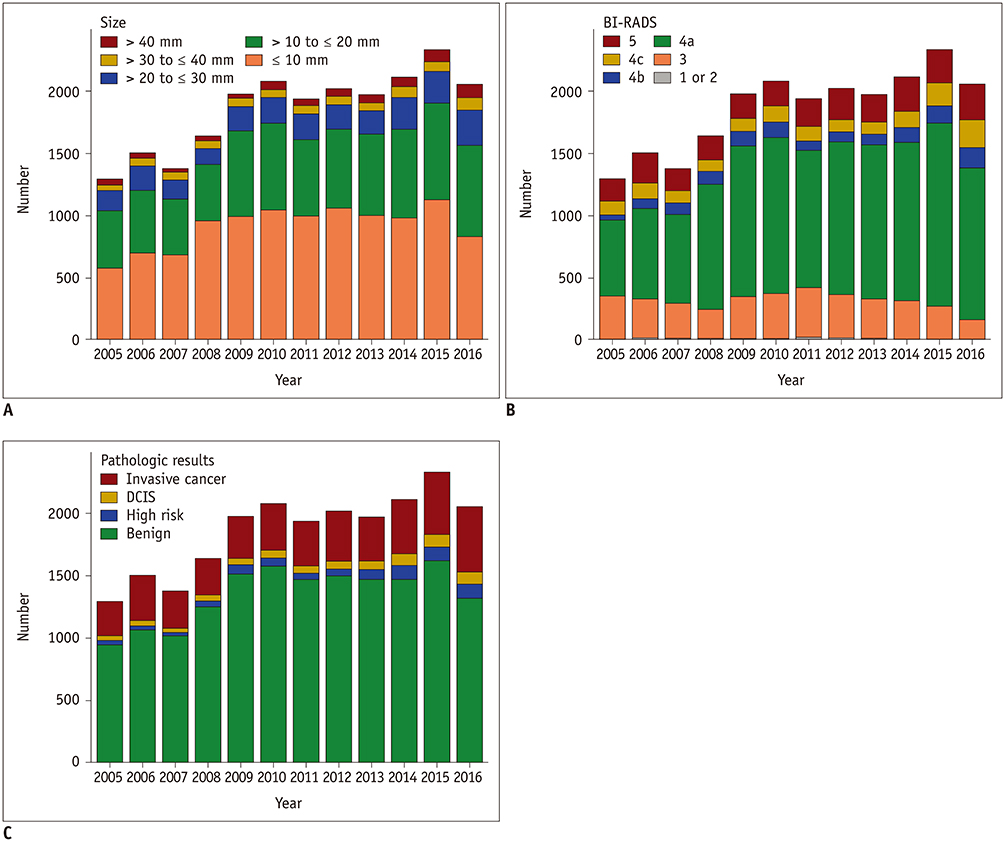
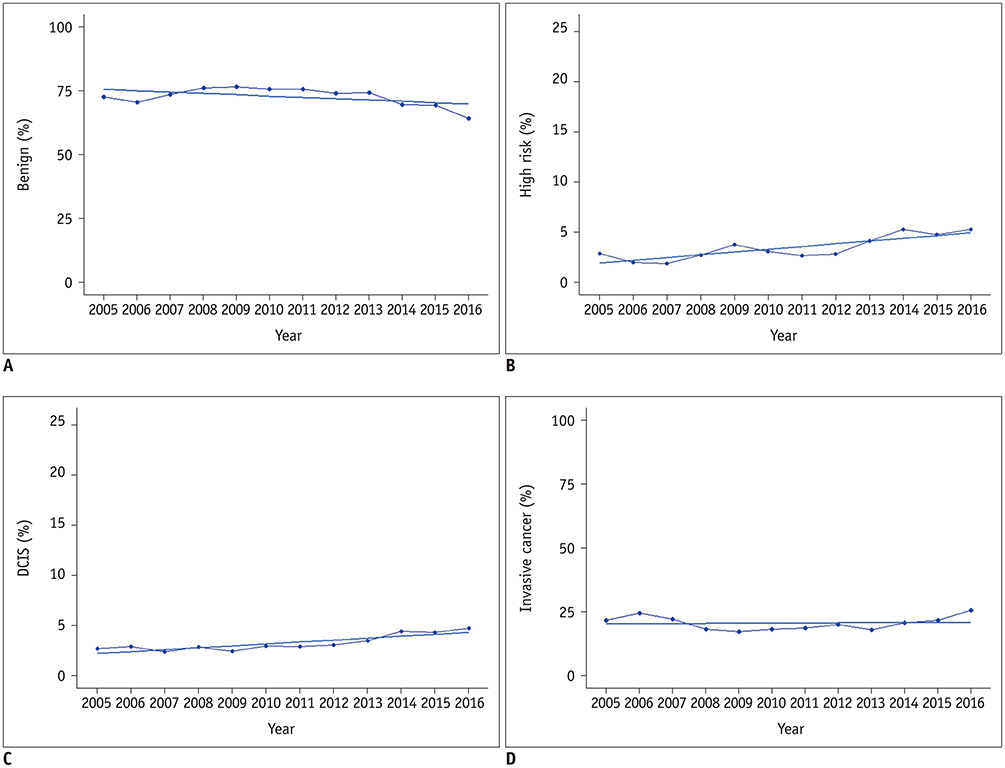
We retrospectively reviewed consecutive US-guided 14-gauge CNBs performed from January 2005 to December 2016 at our institution. A total of 22,297 breast lesions were included. The total number of biopsies, tumor size (≤ 10 mm to > 40 mm), BI-RADS category (1 to 5), and pathologic findings (benign, high risk, ductal carcinoma in situ [DCIS], invasive cancer) were examined annually, and the malignancy rate was analyzed based on the BI-RADS category.
RESULTS
Both the total number of US scans and US-guided CNBs increased while the proportion of US-guided CNBs to the total number of US scans decreased significantly. The number of biopsies classified based on the tumor size, BI-RADS category, and pathologic findings all increased over time, except for BI-RADS categories 1 or 2 and category 3 (odds ratio [OR] = 0.951 per year, 95% confidence interval [CI]: 0.902, 1.002 and odds ratio = 0.979, 95% CI: 0.970, 0.988, respectively). Both the unadjusted and adjusted total malignancy rates and the DCIS rate increased significantly over time. BI-RADS categories 4a, 4b, and 4c showed a significant increasing trend in the total malignancy rate and DCIS rate.
CONCLUSION
The malignancy rate in the results of US-guided 14-gauge CNB for breast lesions increased as the total number of biopsies increased from 2005 to 2016. This trend persisted after adjusting for the BI-RADS category.
Keyword
MeSH Terms
Figure
Reference
-
1. Fuhrman GM, Cederbom GJ, Bolton JS, King TA, Duncan JL, Champaign JL, et al. Image-guided core-needle breast biopsy is an accurate technique to evaluate patients with nonpalpable imaging abnormalities. Ann Surg. 1998; 227:932–939.
Article2. Liberman L. Clinical management issues in percutaneous core breast biopsy. Radiol Clin North Am. 2000; 38:791–807.
Article3. Dillon MF, Hill AD, Quinn CM, O'Doherty A, McDermott EW, O'Higgins N. The accuracy of ultrasound, stereotactic, and clinical core biopsies in the diagnosis of breast cancer, with an analysis of false-negative cases. Ann Surg. 2005; 242:701–707.
Article4. Bassett LW, Mahoney MC, Apple SK. Interventional breast imaging: current procedures and assessing for concordance with pathology. Radiol Clin North Am. 2007; 45:881–894.
Article5. Youk JH, Kim EK, Kim MJ, Oh KK. Sonographically guided 14-gauge core needle biopsy of breast masses: a review of 2,420 cases with long-term follow-up. AJR Am J Roentgenol. 2008; 190:202–207.
Article6. Liberman L, Feng TL, Dershaw DD, Morris EA, Abramson AF. US-guided core breast biopsy: use and cost-effectiveness. Radiology. 1998; 208:717–723.
Article7. Philpotts LE, Hooley RJ, Lee CH. Comparison of automated versus vacuum-assisted biopsy methods for sonographically guided core biopsy of the breast. AJR Am J Roentgenol. 2003; 180:347–351.
Article8. Jung I, Kim MJ, Moon HJ, Yoon JH, Kim EK. Ultrasonography-guided 14-gauge core biopsy of the breast: results of 7 years of experience. Ultrasonography. 2018; 37:55–62.
Article9. Silverstein MJ, Recht A, Lagios MD, Bleiweiss IJ, Blumencranz PW, Gizienski T, et al. Special report: consensus conference III. Image-detected breast cancer: state-of-the-art diagnosis and treatment. J Am Coll Surg. 2009; 209:504–520.10. Lakoma A, Kim ES. Minimally invasive surgical management of benign breast lesions. Gland Surg. 2014; 3:142–148.11. D'Orsi CJ, Sickles EA, Mendelson EB, Morris EA. 2013 ACR BI-RADS Atlas, Breast Imaging Reporting and Data System. 5th ed. Reston, VA: American College of Radiology;2013.12. Spak DA, Plaxco JS, Santiago L, Dryden MJ, Dogan BE. BI-RADS® fifth edition: a summary of changes. Diagn Interv Imaging. 2017; 98:179–190.13. Lee SH, Chang JM, Kim WH, Bae MS, Seo M, Koo HR, et al. Added value of shear-wave elastography for evaluation of breast masses detected with screening US imaging. Radiology. 2014; 273:61–69.
Article14. Kim MY, Cho N, Yi A, Koo HR, Yun BL, Moon WK. Sonoelastography in distinguishing benign from malignant complex breast mass and making the decision to biopsy. Korean J Radiol. 2013; 14:559–567.
Article15. Zheng X, Huang Y, Wang Y, Liu Y, Li F, Han J, et al. Combination of different types of elastography in downgrading ultrasound Breast Imaging-Reporting and Data System category 4a breast lesions. Breast Cancer Res Treat. 2019; 174:423–432.
Article16. Kim SY, Kim MJ, Moon HJ, Yoon JH, Kim EK. Application of the downgrade criteria to supplemental screening ultrasound for women with negative mammography but dense breasts. Medicine (Baltimore). 2016; 95:e5279.
Article17. DeSantis CE, Ma J, Goding Sauer A, Newman LA, Jemal A. Breast cancer statistics, 2017, racial disparity in mortality by state. CA Cancer J Clin. 2017; 67:439–448.
Article18. Trentin C, Dominelli V, Maisonneuve P, Menna S, Bazolli B, Luini A, et al. Predictors of invasive breast cancer and lymph node involvement in ductal carcinoma in situ initially diagnosed by vacuum-assisted breast biopsy: experience of 733 cases. Breast. 2012; 21:635–640.
Article19. Jansen SA. Ductal carcinoma in situ: detection, diagnosis, and characterization with magnetic resonance imaging. Semin Ultrasound CT MR. 2011; 32:306–318.
Article20. Bae S, Yoon JH, Moon HJ, Kim MJ, Kim EK. Breast microcalcifications: diagnostic outcomes according to image-guided biopsy method. Korean J Radiol. 2015; 16:996–1005.
Article21. Soo MS, Baker JA, Rosen EL, Vo TT. Sonographically guided biopsy of suspicious microcalcifications of the breast: a pilot study. AJR Am J Roentgenol. 2002; 178:1007–1015.22. Yi J, Lee EH, Kwak JJ, Cha JG, Jung SH. Retrieval rate and accuracy of ultrasound-guided 14-G semi-automated core needle biopsy of breast microcalcifications. Korean J Radiol. 2014; 15:12–19.
Article23. Ghosh K, Melton LJ III, Suman VJ, Grant CS, Sterioff S, Brandt KR, et al. Breast biopsy utilization: a population-based study. Arch Intern Med. 2005; 165:1593–1598.24. American College of Surgeons. National Accrediation Program for Breast Centers standards manual. Chicago, IL: American College of Surgeons;2018.25. Zimmermann CJ, Sheffield KM, Duncan CB, Han Y, Cooksley CD, Townsend CM Jr, et al. Time trends and geographic variation in use of minimally invasive breast biopsy. J Am Coll Surg. 2013; 216:814–824.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Track Seeding in a Breast Cancer Patient after a 14-Gauge Core Needle Biopsy: A Case Report
- Usefulness of Ultrasound-Guided Automated Core Biopsy of Nonpalpable Breast Lesions
- Sonographically-Guided 14-Gauge Core Needle Biopsy for Papillary Lesions of the Breast
- Clinicopathologic Features of the Papillary Breast Lesions Diagnosed on Ultrasonography-guided Core Needle Biopsy
- Pseudoaneurysm of the Breast after Core Needle Biopsy: A Case Report