Ann Surg Treat Res.
2020 Feb;98(2):72-81. 10.4174/astr.2020.98.2.72.
Prediction of postoperative pancreatic fistula using a nomogram based on the updated definition
- Affiliations
-
- 1Department of Hepatobiliary and Pancreatic Surgery, the First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China. shirleybai@zju.edu.cn
- 2Key Laboratory of Pancreatic Disease of Zhejiang Province, Hangzhou, China.
- 3Department of Hepatobiliary and Pancreatic Surgery, the Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China.
- KMID: 2469106
- DOI: http://doi.org/10.4174/astr.2020.98.2.72
Abstract
- PURPOSE
The International Study Group on Pancreatic Fistula's definition of postoperative pancreatic fistula (POPF) has recently been updated. This study aimed to identify risk factors for POPF in patients having pancreaticoduodenectomy (PD) and to generate a nomogram to predict POPF.
METHODS
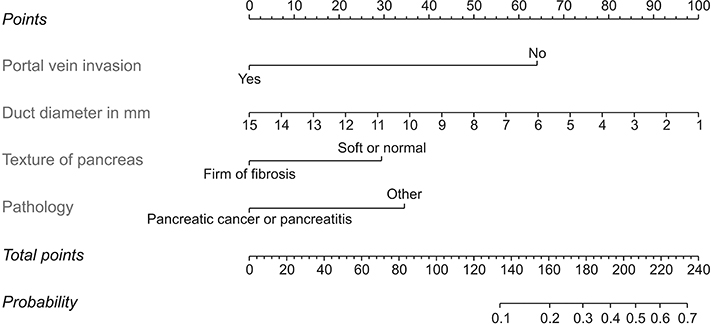
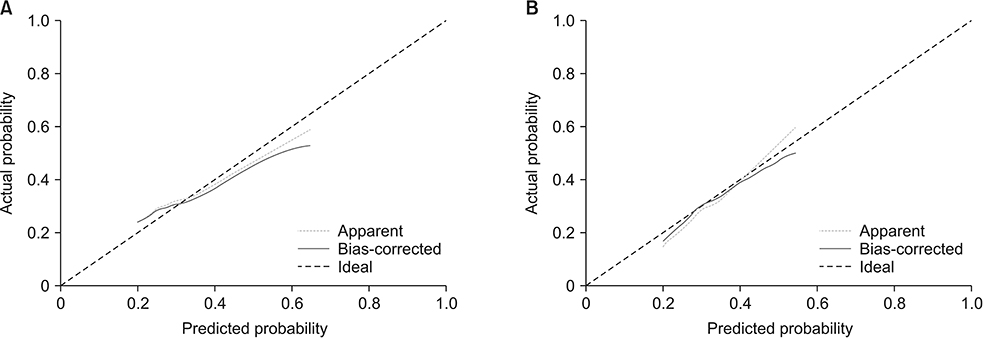
Data on 298 patients who underwent PD from March 2012 to October 2017 was retrospectively reviewed and POPF statuses were redefined. A nomogram was constructed using data from 220 patients and validated using the remaining 78 patients. Independent risk factors for POPF were identified using univariate and multivariate analyses. A predictive nomogram was established based on the independent risk factors and was compared with existing models.
RESULTS
Texture of the pancreas, size of the main pancreatic duct, portal vein invasion, and definitive pathology were the identified risk factors. The nomogram had a C-index of 0.793 and was internally validated. The nomogram performed better (C-index of 0.816) than the other most cited models (C-indexes of 0.728 and 0.735) in the validation cohort. In addition, the nomogram can assign patients into low- (less than 10%), intermediate- (10% to 30%), and high-risk (equal or higher than 30%) groups to facilitate personalized management.
CONCLUSION
The nomogram accurately predicted POPF in patients having PD.
MeSH Terms
Figure
Cited by 1 articles
-
A reinforced suture method for stapled gastrointestinal anastomosis to reduce gastrointestinal hemorrhage during Whipple operation in laparoscopy
La Zhang, Ning Jiang, Liujun Jiang, Rui Liao, Lei Xiang, Baoyong Zhou, Dewei Li
Ann Surg Treat Res. 2022;102(2):110-116. doi: 10.4174/astr.2022.102.2.110.
Reference
-
1. Vin Y, Sima CS, Getrajdman GI, Brown KT, Covey A, Brennan MF, et al. Management and outcomes of postpancreatectomy fistula, leak, and abscess: results of 908 patients resected at a single institution between 2000 and 2005. J Am Coll Surg. 2008; 207:490–498.
Article2. Allen PJ, Gonen M, Brennan MF, Bucknor AA, Robinson LM, Pappas MM, et al. Pasireotide for postoperative pancreatic fistula. N Engl J Med. 2014; 370:2014–2022.
Article3. Ramacciato G, Mercantini P, Petrucciani N, Nigri GR, Kazemi A, Muroni M, et al. Risk factors of pancreatic fistula after pancreaticoduodenectomy: a collective review. Am Surg. 2011; 77:257–269.4. Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005; 138:8–13.
Article5. Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017; 161:584–591.6. Vallance AE, Young AL, Macutkiewicz C, Roberts KJ, Smith AM. Calculating the risk of a pancreatic fistula after a pancreaticoduodenectomy: a systematic review. HPB (Oxford). 2015; 17:1040–1048.
Article7. Callery MP, Pratt WB, Kent TS, Chaikof EL, Vollmer CM Jr. A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. J Am Coll Surg. 2013; 216:1–14.
Article8. Roberts KJ, Hodson J, Mehrzad H, Marudanayagam R, Sutcliffe RP, Muiesan P, et al. A preoperative predictive score of pancreatic fistula following pancreatoduodenectomy. HPB (Oxford). 2014; 16:620–628.
Article9. Ven Fong Z, Correa-Gallego C, Ferrone CR, Veillette GR, Warshaw AL, Lillemoe KD, et al. Early drain removal--the middle ground between the drain versus no drain debate in patients undergoing pancreaticoduodenectomy: a prospective validation study. Ann Surg. 2015; 262:378–383.10. Yamamoto Y, Sakamoto Y, Nara S, Esaki M, Shimada K, Kosuge T. A preoperative predictive scoring system for postoperative pancreatic fistula after pancreaticoduodenectomy. World J Surg. 2011; 35:2747–2755.
Article11. Gaujoux S, Cortes A, Couvelard A, Noullet S, Clavel L, Rebours V, et al. Fatty pancreas and increased body mass index are risk factors of pancreatic fistula after pancreaticoduodenectomy. Surgery. 2010; 148:15–23.
Article12. Miao Y, Lu Z, Zhu Q, Yin J, Zhang K, Dai C, et al. Risk prediction for pancreatic fistula and risk-stratified strategy for prophylactic intra-abdominal drainage after Whipple’s procedure. Pancreatology. 2017; 3 Supplement:S94.
Article13. Gemenetzis G, Bagante F, Griffin JF, Rezaee N, Javed AA, Manos LL, et al. Neutrophil-to-lymphocyte ratio is a predictive marker for invasive malignancy in intraductal papillary mucinous neoplasms of the pancreas. Ann Surg. 2017; 266:339–345.
Article14. Jang JY, Park T, Lee S, Kim Y, Lee SY, Kim SW, et al. Proposed nomogram predicting the individual risk of malignancy in the patients with branch duct type intraductal papillary mucinous neoplasms of the pancreas. Ann Surg. 2017; 266:1062–1068.15. de Castro SM, Biere SS, Lagarde SM, Busch OR, van Gulik TM, Gouma DJ. Validation of a nomogram for predicting survival after resection for adenocarcinoma of the pancreas. Br J Surg. 2009; 96:417–423.
Article16. Shariat SF, Capitanio U, Jeldres C, Karakiewicz PI. Can nomograms be superior to other prediction tools. BJU Int. 2009; 103:492–495.
Article17. Bai X, Zhang Q, Gao S, Lou J, Li G, Zhang Y, et al. Duct-to-mucosa vs invagination for pancreaticojejunostomy after pancreaticoduodenectomy: a prospective, randomized controlled trial from a single surgeon. J Am Coll Surg. 2016; 222:10–18.
Article18. Bai X, Zhang X, Lu F, Li G, Gao S, Lou J, et al. The implementation of an enhanced recovery after surgery (ERAS) program following pancreatic surgery in an academic medical center of China. Pancreatology. 2016; 16:665–670.
Article19. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.20. Shukla PJ, Barreto SG, Fingerhut A, Bassi C, Buchler MW, Dervenis C, et al. Toward improving uniformity and standardization in the reporting of pancreatic anastomoses: a new classification system by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2010; 147:144–153.
Article21. Mungroop TH, van Rijssen LB, van Klaveren D, Smits FJ, van Woerden V, Linnemann RJ, et al. Alternative fistula risk score for pancreatoduodenectomy (a-FRS): design and international external validation. Ann Surg. 2019; 269:937–943.22. Hu BY, Wan T, Zhang WZ, Dong JH. Risk factors for postoperative pancreatic fistula: analysis of 539 successive cases of pancreaticoduodenectomy. World J Gastroenterol. 2016; 22:7797–7805.
Article23. Liu QY, Zhang WZ, Xia HT, Leng JJ, Wan T, Liang B, et al. Analysis of risk factors for postoperative pancreatic fistula following pancreaticoduodenectomy. World J Gastroenterol. 2014; 20:17491–17497.
Article24. Akamatsu N, Sugawara Y, Komagome M, Shin N, Cho N, Ishida T, et al. Risk factors for postoperative pancreatic fistula after pancreaticoduodenectomy: the significance of the ratio of the main pancreatic duct to the pancreas body as a predictor of leakage. J Hepatobiliary Pancreat Sci. 2010; 17:322–328.
Article25. Fu SJ, Shen SL, Li SQ, Hu WJ, Hua YP, Kuang M, et al. Risk factors and outcomes of postoperative pancreatic fistula after pancreatico-duodenectomy: an audit of 532 consecutive cases. BMC Surg. 2015; 15:34.
Article26. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128•9 million children, adolescents, and adults. Lancet. 2017; 390:2627–2642.27. Rungsakulkij N, Mingphruedhi S, Tangtawee P, Krutsri C, Muangkaew P, Suragul W, et al. Risk factors for pancreatic fistula following pancreaticoduodenectomy: a retrospective study in a Thai tertiary center. World J Gastrointest Surg. 2017; 9:270–280.
Article28. Braga M, Capretti G, Pecorelli N, Balzano G, Doglioni C, Ariotti R, et al. A prognostic score to predict major complications after pancreaticoduodenectomy. Ann Surg. 2011; 254:702–707.
Article29. Kimura W, Miyata H, Gotoh M, Hirai I, Kenjo A, Kitagawa Y, et al. A pancreaticoduodenectomy risk model derived from 8575 cases from a national single-race population (Japanese) using a web-based data entry system: the 30-day and in-hospital mortality rates for pancreaticoduodenectomy. Ann Surg. 2014; 259:773–780.30. Cioc AM, Ellison EC, Proca DM, Lucas JG, Frankel WL. Frozen section diagnosis of pancreatic lesions. Arch Pathol Lab Med. 2002; 126:1169–1173.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Definition of and Controversial Issues Regarding Postoperative Pancreatic Fistulas
- External validation of risk prediction platforms for pancreatic fistula after pancreatoduodenectomy using nomograms and artificial intelligence
- Utility of fistula risk score in assessing the risk of postoperative pancreatic fistula occurrence and other significant complications after different types of pancreatic neuroendocrine tumor resections
- A model for predicting pancreatic leakage after pancreaticoduodenectomy based on the international study group of pancreatic surgery classification
- Does international study group on pancreatic fistula (ISGPF) classification need modification after distal pancreatectomy?