Ann Surg Treat Res.
2022 Dec;103(6):340-349. 10.4174/astr.2022.103.6.340.
Utility of fistula risk score in assessing the risk of postoperative pancreatic fistula occurrence and other significant complications after different types of pancreatic neuroendocrine tumor resections
- Affiliations
-
- 1Department of Gastrointestinal Surgery, Faculty of Medical Sciences in Katowice, Medical University of Silesia, Katowice, Poland
- 2Department of General Surgery, St. Alexander Hospital, Kielce, Poland
- KMID: 2536910
- DOI: http://doi.org/10.4174/astr.2022.103.6.340
Abstract
- Purpose
This study was performed to evaluate the utility of the fistula risk score (FRS) and its components in predicting the occurrence of postoperative pancreatic fistula and other significant postoperative complications after resections of pancreatic neuroendocrine tumors.
Methods
Retrospective analysis of 131 patients operated on for pancreatic neuroendocrine tumors between 2015 and 2021 was performed. The correlation of the FRS scale with the occurrence of postoperative pancreatic fistulas and postoperative complications according to the Clavien-Dindo classification was analyzed; only in 109 cases of distal resections and pancreatoduodenectomies (PD).
Results
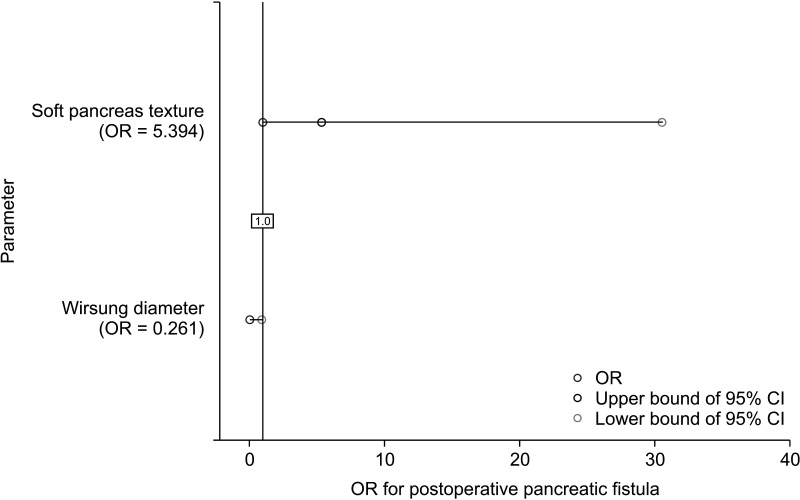
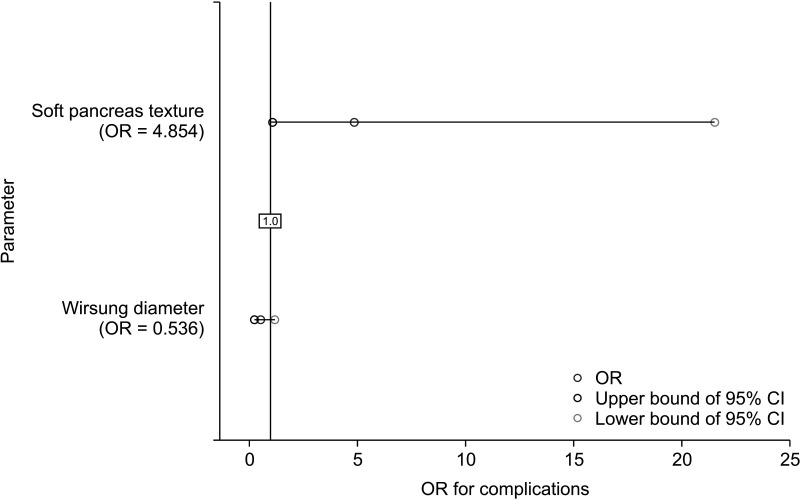
Soft pancreatic texture and intraoperative blood loss of >700 mL are risk factors for clinically significant pancreatic fistula (P = 0.001 and P = 0.001, respectively) and significant postoperative complications (P = 0.016 and P = 0.001, respectively). Wirsung duct diameter (WDD) was associated only with the occurrence of postoperative pancreatic fistula (P = 0.013). FRS scale is associated with the occurrence of pancreatic fistulas and clinically significant postoperative complications in cases of distal resections and PDs (P < 0.001 and P = 0.005, respectively). Postoperative complications are correlated with the occurrence of fistula type B or C (P < 0.001).
Conclusion
Soft pancreatic texture, intraoperative blood loss of >700 mL, and a WDD of ≤3 mm are risk factors for clinically significant postoperative pancreatic fistula. FRS may be applied not only in PDs but also in distal pancreatectomies. Unfortunately, it is not used in total pancreatic resections and enucleations since FRS takes into account the WDD.
Figure
Reference
-
1. Pedrazzoli S. Pancreatoduodenectomy (PD) and postoperative pancreatic fistula (POPF): a systematic review and analysis of the POPF-related mortality rate in 60,739 patients retrieved from the English literature published between 1990 and 2015. Medicine (Baltimore). 2017; 96:e6858. PMID: 28489778.2. Ecker BL, McMillan MT, Allegrini V, Bassi C, Beane JD, Beckman RM, et al. Risk factors and mitigation strategies for pancreatic fistula after distal pancreatectomy: analysis of 2026 resections from the international, multi-institutional distal pancreatectomy study group. Ann Surg. 2019; 269:143–149. PMID: 28857813.3. Unegbu FC, Anjum F. Pancreatic Fistula. Mutignani M, Albert JG, Fabbri C, editors. Endotherapy in biliopancreatic diseases: ERCP meets EUS: two techniques for one vision. Springer Cham;2020. p. 551–560.4. Jilesen AP, van Eijck CH, in’t Hof KH, van Dieren S, Gouma DJ, van Dijkum EJ. Postoperative complications, in-hospital mortality and 5-year survival after surgical resection for patients with a pancreatic neuroendocrine tumor: a systematic review. World J Surg. 2016; 40:729–748. PMID: 26661846.5. Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017; 161:584–591. PMID: 28040257.6. Falconi M, Eriksson B, Kaltsas G, Bartsch DK, Capdevila J, Caplin M, et al. ENETS consensus guidelines update for the management of patients with functional pancreatic neuroendocrine tumors and non-functional pancreatic neuroendocrine tumors. Neuroendocrinology. 2016; 103:153–171. PMID: 26742109.7. Albers MB, Almquist M, Bergenfelz A, Nordenström E. Complications of surgery for gastro-entero-pancreatic neuroendocrine neoplasias. Langenbecks Arch Surg. 2020; 405:137–143. PMID: 32291468.8. Guo CX, Shen YN, Zhang Q, Zhang XZ, Wang JL, Gao SL, et al. Prediction of postoperative pancreatic fistula using a nomogram based on the updated definition. Ann Surg Treat Res. 2020; 98:72–81. PMID: 32051815.9. Tessman D, Chou J, Shebrain S, Munene G. Surgical outcomes of distal pancreatectomy in elderly patients. Am Surg. 2022; 88:115–119. PMID: 33342301.10. Callery MP, Pratt WB, Kent TS, Chaikof EL, Vollmer CM. A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. J Am Coll Surg. 2013; 216:1–14. PMID: 23122535.11. Miller BC, Christein JD, Behrman SW, Drebin JA, Pratt WB, Callery MP, et al. A multi-institutional external validation of the fistula risk score for pancreatoduodenectomy. J Gastrointest Surg. 2014; 18:172–179. discussion 179-80. PMID: 24002771.12. Kos-Kudła B, Rosiek V, Borowska M, Bałdys-Waligórska A, Bednarczuk T, Blicharz-Dorniak J, et al. Pancreatic neuroendocrine neoplasms - management guidelines (recommended by the Polish Network of Neuroendocrine Tumours). Endokrynol Pol. 2017; 68:169–197. PMID: 28540973.13. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196. PMID: 19638912.14. Zovak M, Mužina Mišić D, Glavčić G. Pancreatic surgery: evolution and current tailored approach. Hepatobiliary Surg Nutr. 2014; 3:247–258. PMID: 25392836.15. Jiwani A, Chawla T. Risk factors of pancreatic fistula in distal pancreatectomy patients. Surg Res Pract. 2019; 2019:4940508. PMID: 31396547.16. Stella M, Bissolati M, Gentile D, Arriciati A. Impact of surgical experience on management and outcome of pancreatic surgery performed in high- and low-volume centers. Updates Surg. 2017; 69:351–358. PMID: 28215039.17. Cao X, Zhu S, Luo G, Huang G. Soft pancreas should be assessed histopathologically for fibrosis to predict postoperative pancreatic fistula after pancreaticoduodenectomy. Asian J Surg. 2021; 44:421–422. PMID: 33246802.18. Petrova E, Lapshyn H, Bausch D, D’Haese J, Werner J, Klier T, et al. Risk stratification for postoperative pancreatic fistula using the pancreatic surgery registry StuDoQ|Pancreas of the German Society for General and Visceral Surgery. Pancreatology. 2019; 19:17–25. PMID: 30563791.19. Kumar S, Chandra A, Madhavan SM, Kumar D, Chauhan S, Pandey A, et al. Predictors and outcomes of pancreatic fistula following pancreaticoduodenectomy: a dual center experience. Indian J Surg Oncol. 2021; 12:22–30. PMID: 33814828.20. Schober M, Jesenofsky R, Faissner R, Weidenauer C, Hagmann W, Michl P, et al. Desmoplasia and chemoresistance in pancreatic cancer. Cancers (Basel). 2014; 6:2137–2154. PMID: 25337831.21. Fendrich V, Waldmann J, Bartsch DK, Langer P. Surgical management of pancreatic endocrine tumors. Nat Rev Clin Oncol. 2009; 6:419–428. PMID: 19506584.22. Bartolini I, Bencini L, Risaliti M, Ringressi MN, Moraldi L, Taddei A. Current management of pancreatic neuroendocrine tumors: from demolitive surgery to observation. Gastroenterol Res Pract. 2018; 2018:9647247. PMID: 30140282.23. Satoi S, Yamamoto T, Motoi F, Matsumoto I, Yoshitomi H, Amano R, et al. Clinical impact of developing better practices at the institutional level on surgical outcomes after distal pancreatectomy in 1515 patients: domestic audit of the Japanese Society of Pancreatic Surgery. Ann Gastroenterol Surg. 2018; 2:212–219. PMID: 29863185.24. Eshmuminov D, Schneider MA, Tschuor C, Raptis DA, Kambakamba P, Muller X, et al. Systematic review and meta-analysis of postoperative pancreatic fistula rates using the updated 2016 International Study Group pancreatic fistula definition in patients undergoing pancreatic resection with soft and hard pancreatic texture. HPB (Oxford). 2018; 20:992–1003. PMID: 29807807.25. Martin AN, Narayanan S, Turrentine FE, Bauer TW, Adams RB, Zaydfudim VM. Pancreatic duct size and gland texture are associated with pancreatic fistula after pancreaticoduodenectomy but not after distal pancreatectomy. PLoS One. 2018; 13:e0203841. PMID: 30212577.26. Baxi AC, Jiang Q, Hao J, Yang Z, Woods K, Keilin S, et al. The effect of solid pancreatic mass lesions on pancreatic duct diameter at endoscopic ultrasound. Endosc Ultrasound. 2017; 6:103–108. PMID: 28440235.27. Jilesen AP, van Eijck CH, Busch OR, van Gulik TM, Gouma DJ, van Dijkum EJ. Postoperative outcomes of enucleation and standard resections in patients with a pancreatic neuroendocrine tumor. World J Surg. 2016; 40:715–728. PMID: 26608956.28. Valente R, Lykoudis P, Tamburrino D, Inama M, Passas I, Toumpanakis C, et al. Major postoperative complications after pancreatic resection for P-NETS are not associated to earlier recurrence. Eur J Surg Oncol. 2017; 43:2119–2128. PMID: 28821361.29. Mohamed A, Nicolais L, Fitzgerald TL. Revisiting the pancreatic fistula risk score: clinical nomogram accurately assesses risk. Am Surg. 2021; 31348211047471. PMID: 34633224.30. Chong E, Ratnayake B, Lee S, French JJ, Wilson C, Roberts KJ, et al. Systematic review and meta-analysis of risk factors of postoperative pancreatic fistula after distal pancreatectomy in the era of 2016 International Study Group pancreatic fistula definition. HPB (Oxford). 2021; 23:1139–1151. PMID: 33820687.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Risk Factors of Pancreatic Fistula after Pancratoduodenectomy
- Complication analysis of distal pancreatectomy based on early personal experience
- A Case of a Traumatic Pancreatic Neck Transection Treated with a Binding Pancreaticogastrostomy
- The management of Pancreatic fistula Complicated by Gastric fistulation following Emergency Splenectomy
- Fish-Mouth Closure of the Pancreatic Stump and Parachuting of the Pancreatic End with Double U Trans-Pancreatic Sutures for Pancreatico-Jejunostomy