Nutr Res Pract.
2020 Feb;14(1):32-44. 10.4162/nrp.2020.14.1.32.
Development of the anti-cancer food scoring system 2.0: Validation and nutritional analyses of quantitative anti-cancer food scoring model
- Affiliations
-
- 1Department of Nutrition, Yonsei University, Seoul 03722, Korea.
- 2Department of Cancer Biomedical Science, Graduate School of Cancer Science and Policy, National Cancer Center, Gyeonggi 10408, Korea.
- 3Department of Surgery, Korea University Medical College, Seoul 02841, Korea.
- 4Department of Radiation Oncology, Korea University Medical College and Korea University Ansan hospital, Gyeonggi 15355, Korea. crusion3@naver.com
- KMID: 2468511
- DOI: http://doi.org/10.4162/nrp.2020.14.1.32
Abstract
- BACKGROUND/OBJECTIVES
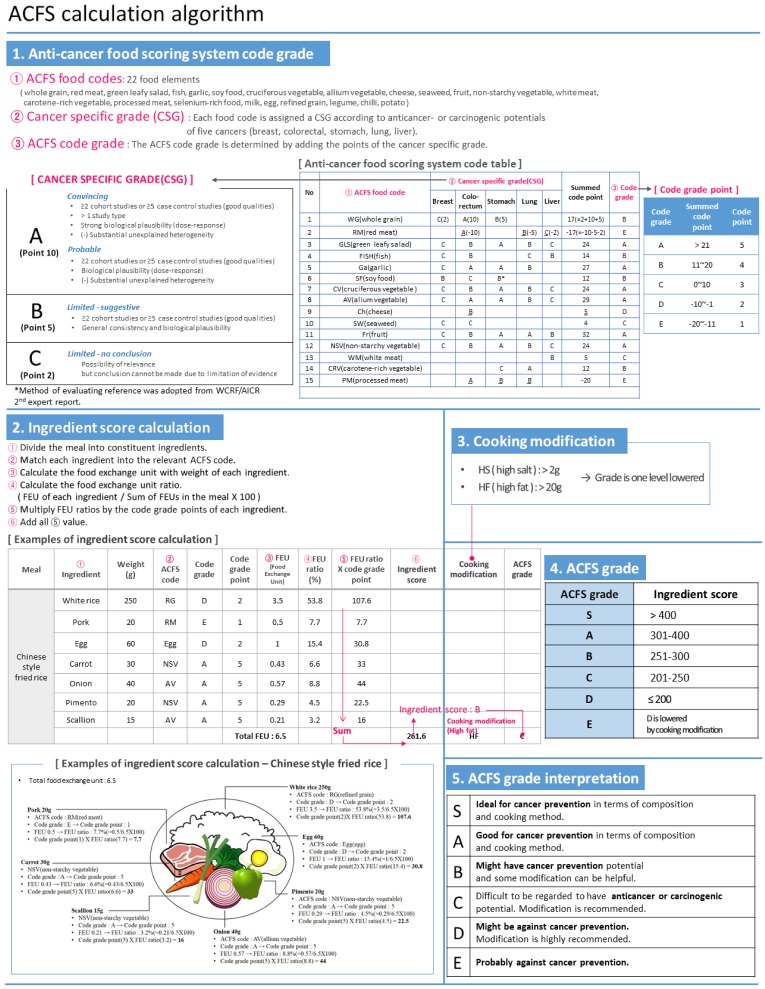
We have previously designed the anti-cancer food scoring model (ACFS) 1.0, an evidence-based quantitative tool analyzing the anti-cancer or carcinogenic potential of diets. Analysis was performed using simple quantitative indexes divided into 6 categories (S, A, B, C, D, and E). In this study, we applied this scoring model to wider recipes and evaluated its nutritional relevance.
MATERIALS/METHODS
National or known regional databases were searched for recipes from 6 categories: Korean out-dining, Korean home-dining, Western, Chinese, Mediterranean, and vegetarian. These recipes were scored using the ACFS formula and the nutrition profiles were analyzed.
RESULTS
Eighty-eight international recipes were analyzed. All S-graded recipes were from vegetarian or Mediterranean categories. The median code values of each category were B (Korean home-dining), C (Korean out-dining), B (Chinese), A (Mediterranean), S (vegetarian), and D (Western). The following profiles were correlated (P < 0.05) with ACFS grades in the univariate trend analysis: total calories, total fat, animal fat, animal protein, total protein, vitamin D, riboflavin, niacin, vitamin Bâ‚â‚‚, pantothenic acid, sodium, animal iron, zinc, selenium, and cholesterol (negative trends), and carbohydrate rate, fiber, water-soluble fiber, vitamin K, vitamin C, and plant calcium (positive trends). Multivariate analysis revealed that animal fat, animal iron, and niacin (negative trends) and animal protein, fiber, and vitamin C (positive trends) were statistically significant. Pantothenic acid and sodium showed non-significant negative trends (P < 0.1), and vitamin Bâ‚â‚‚ showed a non-significant positive trend.
CONCLUSION
This study provided a nutritional basis and extended the utility of ACFS, which is a bridgehead for future cancer-preventive clinical trials using ACFS.
Keyword
MeSH Terms
-
Animals
Ascorbic Acid
Asian Continental Ancestry Group
Calcium
Cholesterol
Diet
Humans
Iron
Multivariate Analysis
Niacin
Pantothenic Acid
Plants
Riboflavin
Selenium
Sodium
Vegetarians
Vitamin D
Vitamin K
Vitamins
Zinc
Ascorbic Acid
Calcium
Cholesterol
Iron
Niacin
Pantothenic Acid
Riboflavin
Selenium
Sodium
Vitamin D
Vitamin K
Vitamins
Zinc
Figure
Reference
-
1. GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the global burden of disease study 2015. Lancet. 2016; 388:1459–1544. PMID: 27733281.2. National Cancer Information Center. Title [Internet]. Goyang: National Cancer Information Center;year. cited 2019 February 1. Available from: https://www.cancer.go.kr/lay1/S1T645C646/contents.do.3. National Center for Health Statistics. Health, United States, 2016: With Chartbook on Long-Term Trends in Health. Hyattsville (MD): National Center for Health Statistics;2017.4. Nagao M, Tsugane S. Cancer in Japan: prevalence, prevention and the role of heterocyclic amines in human carcinogenesis. Genes Environ. 2016; 38:16. PMID: 27375796.
Article5. Anand P, Kunnumakkara AB, Sundaram C, Harikumar KB, Tharakan ST, Lai OS, Sung B, Aggarwal BB. Cancer is a preventable disease that requires major lifestyle changes. Pharm Res. 2008; 25:2097–2116. PMID: 18626751.
Article6. Doll R, Peto R. The causes of cancer: quantitative estimates of avoidable risks of cancer in the United States today. J Natl Cancer Inst. 1981; 66:1191–1308. PMID: 7017215.
Article7. Hastert TA, Beresford SA, Sheppard L, White E. Adherence to the WCRF/AICR cancer prevention recommendations and cancer-specific mortality: results from the vitamins and lifestyle (VITAL) study. Cancer Causes Control. 2014; 25:541–552. PMID: 24557428.
Article8. McCann SE, Marshall JR, Brasure JR, Graham S, Freudenheim JL. Analysis of patterns of food intake in nutritional epidemiology: food classification in principal components analysis and the subsequent impact on estimates for endometrial cancer. Public Health Nutr. 2001; 4:989–997. PMID: 11784412.
Article9. Kerr J, Anderson C, Lippman SM. Physical activity, sedentary behaviour, diet, and cancer: an update and emerging new evidence. Lancet Oncol. 2017; 18:e457–e471. PMID: 28759385.
Article10. Schulze MB, Hoffmann K, Kroke A, Boeing H. Dietary patterns and their association with food and nutrient intake in the European prospective investigation into cancer and nutrition (EPIC)-Potsdam study. Br J Nutr. 2001; 85:363–373. PMID: 11299082.
Article11. Navarro Silvera SA, Mayne ST, Risch H, Gammon MD, Vaughan TL, Chow WH, Dubrow R, Schoenberg JB, Stanford JL, West AB, Rotterdam H, Blot WJ, Fraumeni JF Jr. Food group intake and risk of subtypes of esophageal and gastric cancer. Int J Cancer. 2008; 123:852–860. PMID: 18537156.
Article12. Rim CH. Development of quantitative index evaluating anticancer or carcinogenic potential of diet: the anti-cancer food scoring system 1.0. Nutr Res Pract. 2018; 12:52–60. PMID: 29399297.
Article13. World Cancer Research Fund/American Institute for Cancer Research. Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. Washington, D.C.: American Institute for Cancer Research;2007.14. Hensrud D, Nelson J, Forberg C, Callahan M, Giblin S. The New Mayo Clinic Cookbook: Eating Well for Better Health. Menlo Park (CA): Oxmoor House;2012.15. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, Chun C, Khang YH, Oh K. Data resource profile: the Korea national health and nutrition examination survey (KNHANES). Int J Epidemiol. 2014; 43:69–77. PMID: 24585853.
Article16. Korean Diabetes Association. Korean food exchange list [Internet]. Seoul: Korean Diabetes Association;2010. cited 2018 August 10. Available from: http://www.diabetes.or.kr/english/resource/index.php?category=3.17. Institute of Traditional Korean Food. Beautiful Korean Recipes 300 Selections. Seoul: Hallym Publishing;2008.18. World Cancer Research Fund International. Meat, Fish, and Dairy Products and the Risk of Cancer. London: World Cancer Research Fund International;2018.19. Cross AJ, Sinha R. Meat-related mutagens/carcinogens in the etiology of colorectal cancer. Environ Mol Mutagen. 2004; 44:44–55. PMID: 15199546.
Article20. Alavanja MC, Brown CC, Swanson C, Brownson RC. Saturated fat intake and lung cancer risk among nonsmoking women in Missouri. J Natl Cancer Inst. 1993; 85:1906–1916. PMID: 8230280.
Article21. Sieri S, Krogh V, Ferrari P, Berrino F, Pala V, Thiébaut AC, Tjønneland A, Olsen A, Overvad K, Jakobsen MU, Clavel-Chapelon F, Chajes V, Boutron-Ruault MC, Kaaks R, Linseisen J, Boeing H, Nöthlings U, Trichopoulou A, Naska A, Lagiou P, Panico S, Palli D, Vineis P, Tumino R, Lund E, Kumle M, Skeie G, González CA, Ardanaz E, Amiano P, Tormo MJ, Martínez-García C, Quirós JR, Berglund G, Gullberg B, Hallmans G, Lenner P, Bueno-de-Mesquita HB, van Duijnhoven FJ, Peeters PH, van Gils CH, Key TJ, Crowe FL, Bingham S, Khaw KT, Rinaldi S, Slimani N, Jenab M, Norat T, Riboli E. Dietary fat and breast cancer risk in the European prospective investigation into cancer and nutrition. Am J Clin Nutr. 2008; 88:1304–1312. PMID: 18996867.22. Reddy BS. Types and amount of dietary fat and colon cancer risk: Prevention by omega-3 fatty acid-rich diets. Environ Health Prev Med. 2002; 7:95–102. PMID: 21432290.
Article23. van Asperen IA, Feskens EJ, Bowles CH, Kromhout D. Body iron stores and mortality due to cancer and ischaemic heart disease: a 17-year follow-up study of elderly men and women. Int J Epidemiol. 1995; 24:665–670. PMID: 8550261.
Article24. Knekt P, Reunanen A, Takkunen H, Aromaa A, Heliövaara M, Hakulinen T. Body iron stores and risk of cancer. Int J Cancer. 1994; 56:379–382. PMID: 8314326.
Article25. Shi Y, Yu PW, Zeng DZ. Dose-response meta-analysis of poultry intake and colorectal cancer incidence and mortality. Eur J Nutr. 2015; 54:243–250. PMID: 24788671.
Article26. Yang WS, Wong MY, Vogtmann E, Tang RQ, Xie L, Yang YS, Wu QJ, Zhang W, Xiang YB. Meat consumption and risk of lung cancer: evidence from observational studies. Ann Oncol. 2012; 23:3163–3170. PMID: 22855553.
Article27. Chan JM, Wang F, Holly EA. Pancreatic cancer, animal protein and dietary fat in a population-based study, San Francisco Bay Area, California. Cancer Causes Control. 2007; 18:1153–1167. PMID: 17805983.
Article28. Geelen A, Schouten JM, Kamphuis C, Stam BE, Burema J, Renkema JM, Bakker EJ, van't Veer P, Kampman E. Fish consumption, n-3 fatty acids, and colorectal cancer: a meta-analysis of prospective cohort studies. Am J Epidemiol. 2007; 166:1116–1125. PMID: 17823383.
Article29. Huang RX, Duan YY, Hu JA. Fish intake and risk of liver cancer: a meta-analysis. PLoS One. 2015; 10:e0096102. PMID: 25615823.
Article30. Huang XE, Hirose K, Wakai K, Matsuo K, Ito H, Xiang J, Takezaki T, Tajima K. Comparison of lifestyle risk factors by family history for gastric, breast, lung and colorectal cancer. Asian Pac J Cancer Prev. 2004; 5:419–427. PMID: 15546249.31. World Cancer Research Fund International. Wholegrains, Vegetables and Fruit and the Risk of Cancer. London: World Cancer Research Fund International;2018.32. Slavin JL. Mechanisms for the impact of whole grain foods on cancer risk. J Am Coll Nutr. 2000; 19:300S–307S. PMID: 10875601.
Article33. Bingham SA. Mechanisms and experimental and epidemiological evidence relating dietary fibre (non-starch polysaccharides) and starch to protection against large bowel cancer. Proc Nutr Soc. 1990; 49:153–171. PMID: 2172992.
Article34. Aune D, Chan DS, Greenwood DC, Vieira AR, Rosenblatt DA, Vieira R, Norat T. Dietary fiber and breast cancer risk: a systematic review and meta-analysis of prospective studies. Ann Oncol. 2012; 23:1394–1402. PMID: 22234738.
Article35. Bradbury KE, Appleby PN, Key TJ. Fruit, vegetable, and fiber intake in relation to cancer risk: findings from the European prospective investigation into cancer and nutrition (EPIC). Am J Clin Nutr. 2014; 100 Suppl 1:394S–398S. PMID: 24920034.
Article36. Block G. Vitamin C and cancer prevention: the epidemiologic evidence. Am J Clin Nutr. 1991; 53:270S–282S. PMID: 1985398.
Article37. Byers T, Guerrero N. Epidemiologic evidence for vitamin C and vitamin E in cancer prevention. Am J Clin Nutr. 1995; 62:1385S–1392S. PMID: 7495236.
Article39. Park SM, Li T, Wu S, Li WQ, Weinstock M, Qureshi AA, Cho E. Niacin intake and risk of skin cancer in US women and men. Int J Cancer. 2017; 140:2023–2031. PMID: 28152570.
Article40. Sun NH, Huang XZ, Wang SB, Li Y, Wang LY, Wang HC, Zhang CW, Zhang C, Liu HP, Wang ZN. A dose-response meta-analysis reveals an association between vitamin B12 and colorectal cancer risk. Public Health Nutr. 2016; 19:1446–1456. PMID: 26373257.
Article41. Miranti EH, Stolzenberg-Solomon R, Weinstein SJ, Selhub J, Männistö S, Taylor PR, Freedman ND, Albanes D, Abnet CC, Murphy G. Low vitamin B12 increases risk of gastric cancer: a prospective study of one-carbon metabolism nutrients and risk of upper gastrointestinal tract cancer. Int J Cancer. 2017; 141:1120–1129. PMID: 28568053.42. Cui LH, Quan ZY, Piao JM, Zhang TT, Jiang MH, Shin MH, Choi JS. Plasma folate and vitamin B12 levels in patients with hepatocellular carcinoma. Int J Mol Sci. 2016; 17:E1032. PMID: 27376276.
Article43. D'Elia L, Galletti F, Strazzullo P. Dietary salt intake and risk of gastric cancer. Cancer Treat Res. 2014; 159:83–95. PMID: 24114476.44. World Cancer Research Fund International. Preservation and Processing of Foods and the Risk of Cancer. London: World Cancer Research Fund International;2018.45. Hutschenreuther A, Birkenmeier G, Bigl M, Krohn K, Birkemeyer C. Glycerophosphoglycerol, beta-alanine, and pantothenic acid as metabolic companions of glycolytic activity and cell migration in breast cancer cell lines. Metabolites. 2013; 3:1084–1101. PMID: 24958267.
Article46. International Agency for Research on Cancer. Agents classified by the IARC monographs, vol 1-100 [Internet]. Lyon: International Agency for Research on Cancer;year. cited 2019 May 1. Available from: https://monographs.iarc.fr/wp-content/uploads/2018/09/ClassificationsAlphaOrder.pdf.47. World Cancer Research Fund International. Judging the Evidence. London: World Cancer Research Fund International;2018.48. JH FuhrmanK Leville. Whole Foods Market, Inc.Methods for developing and conducting a nutritional treatment program. United States patent. US 20080177572A1. 2008. 7. 24.49. Katz DL, Njike VY, Rhee LQ, Reingold A, Ayoob KT. Performance characteristics of NuVal and the overall nutritional quality index (ONQI). Am J Clin Nutr. 2010; 91:1102S–1108S. PMID: 20181809.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development of quantitative index evaluating anticancer or carcinogenic potential of diet: the anti-cancer food scoring system 1.0
- Development and validation of a novel scoring system to predict the risk of uterine perforation during intracavitary brachytherapy for cervical cancer
- New Scoring System for Predicting Mortality in Patients with COVID-19
- Prediction of Oncotype DX Recurrence Score Based on Systematic Evaluation of Ki-67 Scores in Hormone ReceptorPositive Early Breast Cancer
- Update on Early Nutrition and Food Allergy in Children