Korean J Radiol.
2017 Feb;18(1):180-193. 10.3348/kjr.2017.18.1.180.
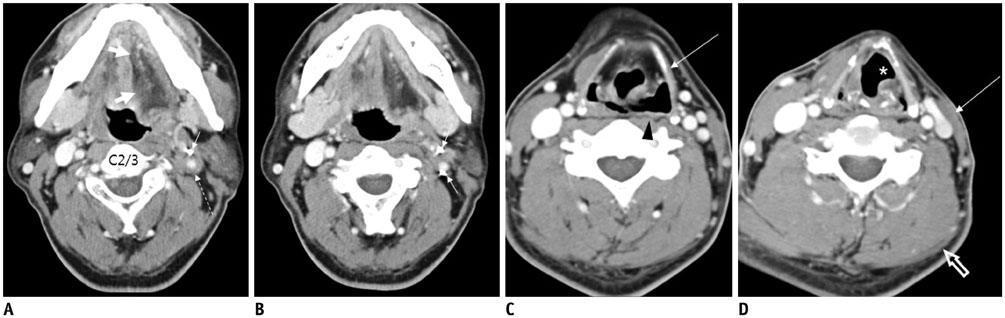
High-resolution Imaging of Neural Anatomy and Pathology of the Neck
- Affiliations
-
- 1Department of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul 05505, Korea. jeonghlee@amc.seoul.kr
- 2Department of Medical Imaging, Chung Shan Medical University Hospital, Taichung 402, Taiwan.
- 3School of Medical Imaging and Radiological Sciences, Chung Shan Medical University, Taichung 402, Taiwan.
- 4Department of Veterinary Medicine, National Chung Hsing University, Taichung 402, Taiwan.
- KMID: 2468132
- DOI: http://doi.org/10.3348/kjr.2017.18.1.180
Abstract
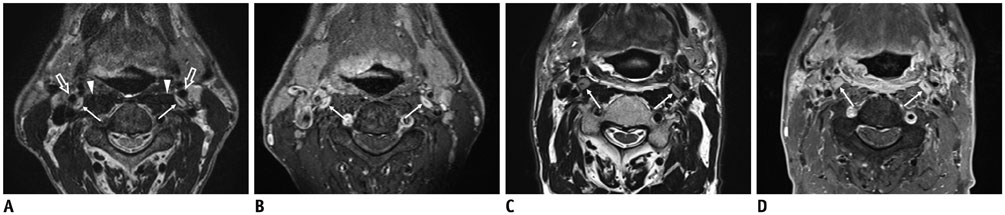
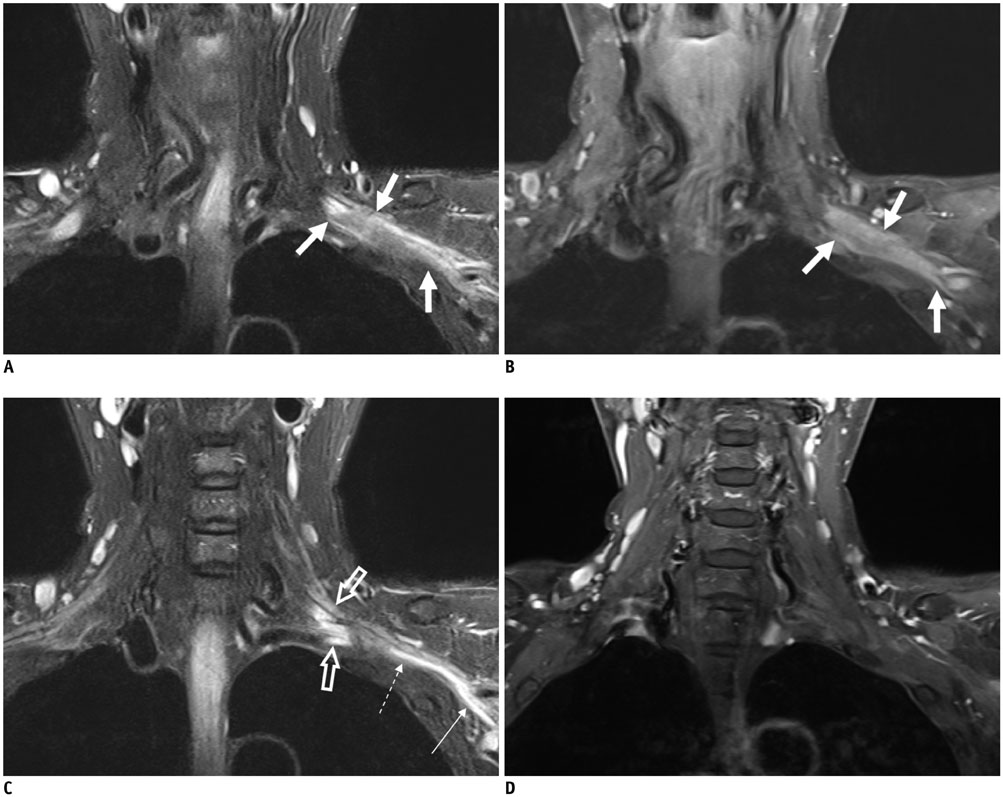
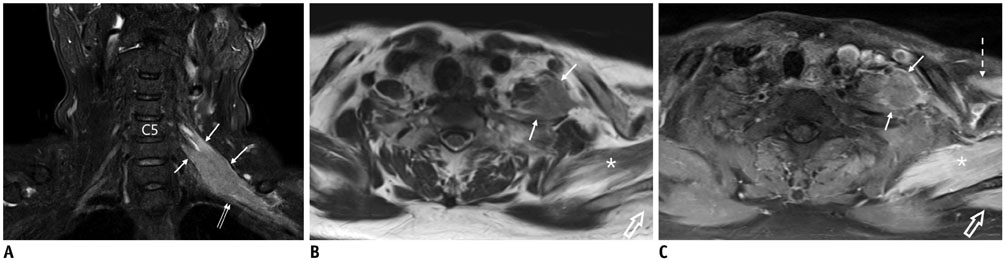
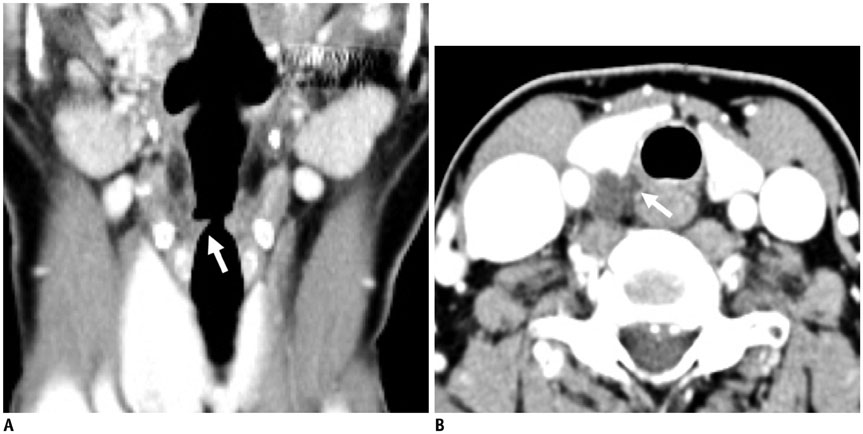
- The neck has intricately connected neural structures, including cervical and brachial plexi, the sympathetic system, lower cranial nerves, and their branches. Except for brachial plexus, there has been little research regarding the normal imaging appearance or corresponding pathologies of neural structures in the neck. The development in imaging techniques with better spatial resolution and signal-to-noise ratio has made it possible to see many tiny nerves to predict complications related to image-guided procedures and to better assess treatment response, especially in the management of oncology patients. The purposes of this review is to present imaging-based anatomy of major nerves in the neck and explain their relevant clinical significance according to representative pathologies of regarded nerves in the neck.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Use of Magnetic Resonance Neurography for Evaluating the Distribution and Patterns of Chronic Inflammatory Demyelinating Polyneuropathy
Xiaoyun Su, Xiangquan Kong, Zuneng Lu, Min Zhou, Jing Wang, Xiaoming Liu, Xiangchuang Kong, Huiting Zhang, Chuansheng Zheng
Korean J Radiol. 2020;21(4):483-493. doi: 10.3348/kjr.2019.0739.
Reference
-
1. Kiray A, Arman C, Naderi S, Güvencer M, Korman E. Surgical anatomy of the cervical sympathetic trunk. Clin Anat. 2005; 18:179–185.2. Saylam CY, Ozgiray E, Orhan M, Cagli S, Zileli M. Neuroanatomy of cervical sympathetic trunk: a cadaveric study. Clin Anat. 2009; 22:324–330.3. Lee JH, Lee HK, Lee DH, Choi CG, Kim SJ, Suh DC. Neuroimaging strategies for three types of Horner syndrome with emphasis on anatomic location. AJR Am J Roentgenol. 2007; 188:W74–W81.4. Lee JY, Lee JH, Song JS, Song MJ, Hwang SJ, Yoon RG, et al. Superior cervical sympathetic ganglion: normal imaging appearance on 3T-MRI. Korean J Radiol. 2016; 17:e72.5. Hogan QH, Erickson SJ. MR imaging of the stellate ganglion: normal appearance. AJR Am J Roentgenol. 1992; 158:655–659.6. Shin JE, Baek JH, Ha EJ, Choi YJ, Choi WJ, Lee JH. Ultrasound features of middle cervical sympathetic ganglion. Clin J Pain. 2015; 31:909–913.7. Mancall EL, Brock DG. Cervical plexus. In : Mancall EL, Brock DG, editors. Gray's clinical neuroanatomy: the anatomic basis for clinical neuroscience. Philadelphia: Elsevier Health Sciences;2011. p. 315–317.8. Bowen BC, Pattany PM, Saraf-Lavi E, Maravilla KR. The brachial plexus: normal anatomy, pathology, and MR imaging. Neuroimaging Clin N Am. 2004; 14:59–85. vii–viii.9. Aralasmak A, Karaali K, Cevikol C, Uysal H, Senol U. MR imaging findings in brachial plexopathy with thoracic outlet syndrome. AJNR Am J Neuroradiol. 2010; 31:410–417.10. van Es HW, Bollen TL, van Heesewijk HP. MRI of the brachial plexus: a pictorial review. Eur J Radiol. 2010; 74:391–402.11. Ha EJ, Lee JH, Lim HK, Bae Kim W, Baek JH. Identification of continuity of transected nerve on sonography after neck dissection: direct sign of traumatic neuroma. Thyroid. 2011; 21:1385–1387.12. Ha EJ, Baek JH, Lee JH, Kim YJ, Kim JK, Kim TY, et al. Characteristic ultrasound feature of traumatic neuromas after neck dissection: direct continuity with the cervical plexus. Thyroid. 2012; 22:820–826.13. Ha EJ, Baek JH, Lee JH, Kim JK, Shong YK. Clinical significance of vagus nerve variation in radiofrequency ablation of thyroid nodules. Eur Radiol. 2011; 21:2151–2157.14. Felten DL, O'Banion MK, Maida ME. Brain stem and cerebellum. In : Felten DL, O'Banion MK, Maida ME, editors. Netter's atlas of neuroscience. Philadelphia: Elsevier Health Sciences;2015. p. 247–287.15. Park JK, Jeong SY, Lee JH, Lim GC, Chang JW. Variations in the course of the cervical vagus nerve on thyroid ultrasonography. AJNR Am J Neuroradiol. 2011; 32:1178–1181.16. Henry JF, Audiffret J, Denizot A, Plan M. The nonrecurrent inferior laryngeal nerve: review of 33 cases, including two on the left side. Surgery. 1988; 104:977–984.17. Toniato A, Mazzarotto R, Piotto A, Bernante P, Pagetta C, Pelizzo MR. Identification of the nonrecurrent laryngeal nerve during thyroid surgery: 20-year experience. World J Surg. 2004; 28:659–661.18. Chen CC, Huang YC, Lee ST, Chen JF, Wu CT, Tu PH. Long-term result of vocal cord paralysis after anterior cervical disectomy. Eur Spine J. 2014; 23:622–626.19. Jung A, Schramm J. How to reduce recurrent laryngeal nerve palsy in anterior cervical spine surgery: a prospective observational study. Neurosurgery. 2010; 67:10–15. discussion 15.20. Saman M, Etebari P, Pakdaman MN, Urken ML. Anatomic relationship between the spinal accessory nerve and the jugular vein: a cadaveric study. Surg Radiol Anat. 2011; 33:175–179.21. Hong MJ, Baek JH, Kim DY, Ha EJ, Choi WJ, Choi YJ, et al. Spinal accessory nerve: ultrasound findings and correlations with neck lymph node levels. Ultraschall Med. 2014; 12. 17. [Epub]. DOI: 10.1055/s-0034-1385673.22. Kim DH, Cho YJ, Tiel RL, Kline DG. Surgical outcomes of 111 spinal accessory nerve injuries. Neurosurgery. 2003; 53:1106–1112. discussion 1102-1103.23. Cappiello J, Piazza C, Nicolai P. The spinal accessory nerve in head and neck surgery. Curr Opin Otolaryngol Head Neck Surg. 2007; 15:107–111.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- High-Resolution Finger MRI: What Should You Look for in Trauma of the Fingers?
- Ansa cervicalis: a comprehensive review of its anatomy, variations, pathology, and surgical applications
- Imaging of the Brachial Plexus
- Magnetic Resonance Imaging in Diplopia: Neural Pathway, Imaging, and Clinical Correlation
- Anatomy and Pathology of the L5 Exiting Nerve in the Lumbosacral Spine