Kosin Med J.
2019 Dec;34(2):138-145. 10.7180/kmj.2019.34.2.138.
The Characteristics of Staphylococcal Scalded Skin Syndrome in Atopic Dermatitis
- Affiliations
-
- 1Department of Pediatrics, Busan St. Mary's Hospital, Busan, Korea. hyh190@naver.com
- KMID: 2467974
- DOI: http://doi.org/10.7180/kmj.2019.34.2.138
Abstract
OBJECTIVES
Staphylococcal scalded skin syndrome (4S), a blistering dermatosis caused by exfoliative toxins from Staphylococcus aureus, occurs frequently in patients with atopic dermatitis (AD). However, association between 4S and AD has not rarely been reported. We investigated the characteristics of 4S according to AD status.
METHODS
The study included 146 children with 4S who visited Busan St. Mary's Hospital from 2007-2018. Clinical features were analyzed from medical records and pictures, and 4S was classified as localized or generalized. We also retrospectively investigated the preceding conditions and test results related to AD.
RESULTS
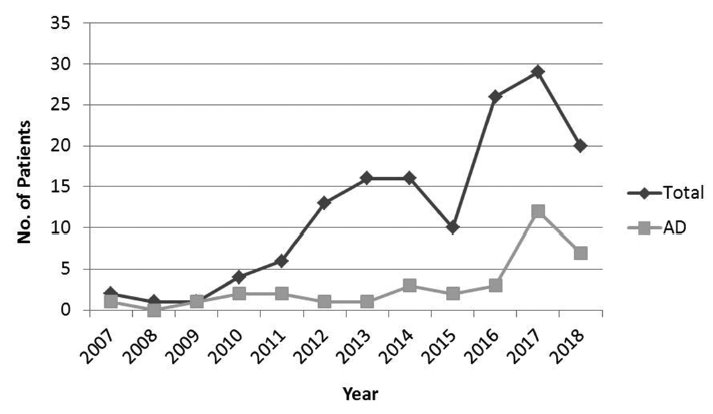
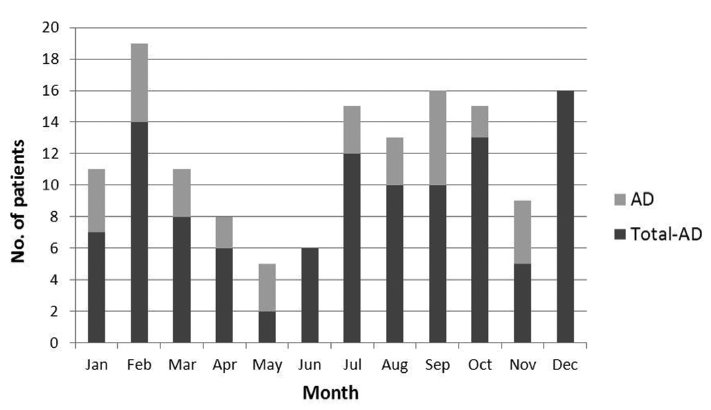
Among 146 patients with 4S, median age was 2.0 years, and 35 (24.0%) had AD. Since 2007, the incidence of both 4S and AD have increased, without obvious seasonal patterns. Generalized and localized disease occurred in 90 and 56 patients, respectively. Twenty-four of 35 patients with AD (68.6%) and 32 of 111 (28.8%) without AD had localized disease. Significant differences were observed between the groups (P = 0.000). Among those with AD, the most common preceding condition was skin infection or unknown (45.2%); however, respiratory disease was the most common (47.9%) among patients without AD. Eosinophil levels were higher in the AD group (P = 0.002), and there were no statistically significant differences in total immunoglobulin E (IgE), Dermatophagoides farinae (Df IgE), egg-white IgE, and culture results between the groups.
CONCLUSIONS
Localized 4S frequently occurred without preceding conditions in children with AD and usually arose from skin infection compared to generalized 4S.
MeSH Terms
Figure
Reference
-
1. Berk DR, Bayliss SJ. MRSA, Staphylococcal scalded skin syndrome, and other cutaneous bacterial emergencies. Pediatr Ann. 2010; 39:627.
Article2. Park CH, Na SR, Cho HM, Yoo EJ, Jung K, Kim EY, et al. Clinical features and the associated factors of staphylococcal scalded skin syndrome during the recent 10 years. Korean J Pediatr Infect Dis. 2008; 15:152–161.
Article3. Heo SY, Song YJ, Kim SJ, Park SY, Kang DC, Ma SH. A clinical review of community acquired methicillin resistant staphylococcal scalded skin syndrome. Korean J Pediatr Infect Dis. 2007; 14:83–90.
Article4. Lee JS, Kim TH, Cho GL, Jung JA, Kim JH. The classification between IgE and non-IgE mediated atopic dermatitis in Korean children. Pediatr Allergy Respir Dis. 2005; 15:352–358.
Article5. Uehara M, Izukura R, Sawai T. Blood eosinophilia in atopic dermatitis. Clin Exp Dermatol. 1990; 15:264–266.
Article6. Melish ME, Glasgow LA. The staphylococcal scalded-skin syndrome: development of an experimental model. N Engl J Med. 1970; 282:1114–1119.7. Manders SM. Toxin-mediated streptococcal and staphylococcal disease. J Am Acad Dermatol. 1998; 39:383–398.
Article8. Iwatsuki K, Yamasaki O, Morizane S, Oono T. Staphylococcal cutaneous infections: invasion, evasion and aggression. J Dermatol Sci. 2006; 42:203–214.
Article9. Handler MZ, Schwartz RA. Staphylococcal scalded skin syndrome: diagnosis and management in children and adults. J Eur Acad Dermatol Venereol. 2014; 28:1418–1423.
Article10. Staiman A, Hsu DY, Silverberg JI. Epidemiology of staphylococcal scalded skin syndrome in U.S. Children. Br J Dermatol. 2018; 178:704–708.
Article11. Arnold JD, Hoek SN, Kirkorian A. Epidemiology of staphylococcal scalded skin syndrome in the United States: A cross-sectional study, 2010-2014. J Am Acad Dermatol. 2018; 78:404–406.
Article12. Park JW, Hwang DK, Yu HJ. Staphylococcal scalded skin syndrome, review of 20 cases. Korean J Dermatol. 2002; 40:1051–1057.13. Lee SH, Choi WK, Jung CH, Chung CJ, Lee DJ. Staphylococcal scalded skin syndrome in children: comparison of the clinical features of that isolated methicilin-resistant and methicillin-sensitive Staphylococcus aureus. Korean J Pediatr Infect Dis. 2004; 11:183–191.
Article14. Kang JD, Park SD. Reclassification of staphylococcal scalded skin syndrome by clinical analysis of 25 cases. Korean J Dermatol. 2004; 42:398–405.15. Hubiche T, Bes M, Roudiere L, Langlaude F, Etienne J, Del Giudice P. Mild Staphylococcal scalded skin syndrome: an underdiagnosed clinical disorder. Br J Dermatol. 2012; 166:213–215.
Article16. Bae SH, Lee JB, Kim SJ, Lee SC, Won YH, Yun SJ. Case of bullous impetigo with enormous bulla developing into staphylococcal scalded skin syndrome. J Dermatol. 2016; 43:459–460.
Article17. Elias PM, Levy SW. Bullous impetigo: Occurrence of localized scalded skin syndrome in an adult. Arch Dermatol. 1976; 112:856–858.
Article18. Dancer SJ, Noble WC. Nasal, axillary, and perineal carriage of Staphylococcus aureus among women : identification of strains producing epidermolytic toxin. J Clin Pathol. 1991; 44:681–684.
Article19. Goolamali SI, Haddadeen C, Creamer JD, Hay R, Higgins EM, Morris-jones R. Localized staphylococcal scalded skin syndrome in five patients with atopic dermatitis. Br J Dermatol. 2010; 163:41–42.20. Simon D, Braathen LR, Simon HU. Eosinophils and atopic dermatitis. Allergy. 2004; 59:561–570.
Article