J Clin Neurol.
2019 Apr;15(2):191-204. 10.3988/jcn.2019.15.2.191.
Transient and Adult Patients with Neurologic Diseases in the Pediatric Emergency Department: Trends and Characteristics
- Affiliations
-
- 1Department of Pediatrics, Yonsei University College of Medicine, Seoul, Korea. ymleemd@yuhs.ac
- 2Epilepsy Research Institute, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2467733
- DOI: http://doi.org/10.3988/jcn.2019.15.2.191
Abstract
- BACKGROUND AND PURPOSE
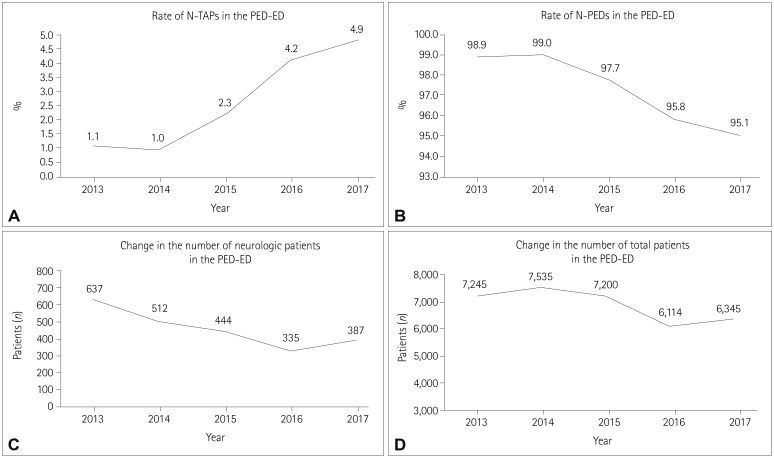
There is an increasing rate of presentations by transient and adult patients (TAPs) to pediatric emergency departments (PED-EDs). TAPs with neurologic diseases (N-TAPs) comprise most of these patients. We investigated this trend and compared the characteristics of N-TAPs with those of pediatric patients with neurologic diseases (N-PEDs) who presented to the PED-ED of a tertiary-care hospital in Korea.
METHODS
We reviewed the medical records of neurologic patients who presented to the PED-ED of a single tertiary-care hospital from 2013 to 2017. We included patients with neurologic symptoms or diseases and those who were treated in the pediatric neurology department and underwent neurologic evaluations and treatment in the PED-ED.
RESULTS
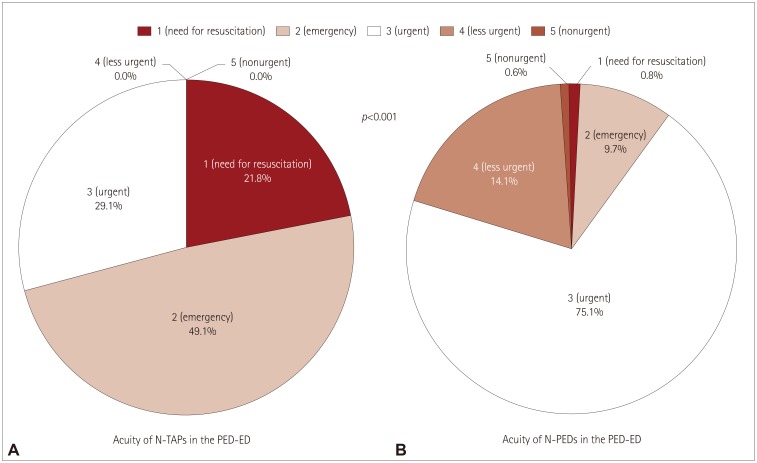
Presentations by N-TAPs to the PED-ED increased over time, whereas the number of N-PEDs gradually decreased, with a significant difference between the groups (p<0.001). The number of N-TAPs who presented to the PED-ED almost tripled from 2013 to 2017. N-TAPs had significantly more acute symptoms than N-PEDs, and a significantly higher proportion of N-TAPs were insured by Medical Aid compared to N-PEDs (p<0.001). The admission rate was significantly higher (p<0.001) and the mean hospital stay was longer (p=0.046) for N-TAPs. Epilepsy and neurometabolic diseases were mainly responsible for the increased presentations by N-TAPs.
CONCLUSIONS
We have clarified the status of N-TAPs in the PED-ER and the role of pediatric neurologists who manage them. Multidisciplinary treatments focusing on the role of pediatric neurologists should be developed to that systematic long-term care plans are applied to N-TAPs.
MeSH Terms
Figure
Reference
-
1. Camfield PR, Camfield CS. What happens to children with epilepsy when they become adults? Some facts and opinions. Pediatr Neurol. 2014; 51:17–23. PMID: 24830766.
Article2. Davis AM, Brown RF, Taylor JL, Epstein RA, McPheeters ML. Transition care for children with special health care needs. Pediatrics. 2014; 134:900–908. PMID: 25287460.
Article3. Goodman DM, Hall M, Levin A, Watson RS, Williams RG, Shah SS, et al. Adults with chronic health conditions originating in childhood: inpatient experience in children’s hospitals. Pediatrics. 2011; 128:5–13. PMID: 21708805.
Article4. Borlot F, Tellez-Zenteno JF, Allen A, Ali A, Snead OC 3rd, Andrade DM. Epilepsy transition: challenges of caring for adults with childhood-onset seizures. Epilepsia. 2014; 55:1659–1666. PMID: 25169716.
Article5. Andrade DM, Bassett AS, Bercovici E, Borlot F, Bui E, Camfield P, et al. Epilepsy: transition from pediatric to adult care. Recommendations of the Ontario epilepsy implementation task force. Epilepsia. 2017; 58:1502–1517. PMID: 28681381.
Article6. Wakamoto H, Nagao H, Hayashi M, Morimoto T. Long-term medical, educational, and social prognoses of childhood-onset epilepsy: a population-based study in a rural district of Japan. Brain Dev. 2000; 22:246–255. PMID: 10838113.
Article7. Camfield P, Camfield C, Busiah K, Cohen D, Pack A, Nabbout R. The transition from pediatric to adult care for youth with epilepsy: basic biological, sociological, and psychological issues. Epilepsy Behav. 2017; 69:170–176. PMID: 28089368.
Article8. Okumura MJ, Heisler M, Davis MM, Cabana MD, Demonner S, Kerr EA. Comfort of general internists and general pediatricians in providing care for young adults with chronic illnesses of childhood. J Gen Intern Med. 2008; 23:1621–1627. PMID: 18661191.
Article9. McDonnell WM, Kocolas I, Roosevelt GE, Yetman AT. Pediatric emergency department use by adults with chronic pediatric disorders. Arch Pediatr Adolesc Med. 2010; 164:572–576. PMID: 20530309.
Article10. Geerlings RP, Aldenkamp AP, De With PH, Zinger S, Gottmer-Welschen LM, De Louw AJ. Transition to adult medical care for adolescents with epilepsy. Epilepsy Behav. 2015; 44:127–135. PMID: 25679495.
Article11. Bourgeois FT, Shannon MW. Adult patient visits to children's hospital emergency departments. Pediatrics. 2003; 111:1268–1272. PMID: 12777540.
Article12. Little WK, Hirsh DA. Adult patients in the pediatric emergency department: presentation and disposition. Pediatr Emerg Care. 2014; 30:808–811. PMID: 25343738.13. Lee B, Kim DK, Park JD, Kwak YH. Clinical considerations when applying vital signs in pediatric Korean Triage and Acuity Scale. J Korean Med Sci. 2017; 32:1702–1707. PMID: 28875617.
Article14. Kim JH, Lee KS, Yoo KB, Park EC. The differences in health care utilization between Medical Aid and health insurance: a longitudinal study using propensity score matching. PLoS One. 2015; 10:e0119939. PMID: 25816234.
Article15. Kim JH, Kim NR, Park EC, Han KT, Choi Y, Lee SG. Impact of continuous Medical Aid utilisation on healthcare utilisation: unique insight using the 2008-2012 Korean Welfare Panel Study (KOWEPS). BMJ Open. 2016; 6:e008583.
Article16. Rhine T, Gittelman M, Timm N. Prevalence and trends of the adult patient population in a pediatric emergency department. Pediatr Emerg Care. 2012; 28:141–144. PMID: 22270503.
Article17. Nabbout R, Andrade DM, Bahi-Buisson N, Cross H, Desquerre I, Dulac O, et al. Outcome of childhood-onset epilepsy from adolescence to adulthood: transition issues. Epilepsy Behav. 2017; 69:161–169. PMID: 28256379.
Article18. Nabbout R, Camfield CS, Andrade DM, Arzimanoglou A, Chiron C, Cramer JA, et al. Treatment issues for children with epilepsy transitioning to adult care. Epilepsy Behav. 2017; 69:153–160. PMID: 28188045.
Article19. Camfield C, Camfield P. Preventable and unpreventable causes of childhood-onset epilepsy plus mental retardation. Pediatrics. 2007; 120:e52–e55. PMID: 17606549.
Article20. Statistics Korea. Final results of birth statistics in 2016 [Internet]. Daejeon: Statistics Korea;2017. cited 2018 Mar 13. Available from: http://kostat.go.kr/portal/eng/pressReleases/1/index.board?bmode=read&aSeq=363582.21. Korean Statistical Information Service. International statistical yearbook: total fertility rate OECD [Internet]. Daejeon: Statistics Korea;2018. cited 2018 Mar 13. Available from: http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_2KAA207_OECD#.22. Michihata N, Matsui H, Fushimi K, Yasunaga H. Clinical features of adult patients admitted to pediatric wards in Japan. J Adolesc Health. 2015; 57:421–424. PMID: 26403841.
Article23. Edwards JD, Vasilevskis EE, Yoo EJ, Houtrow AJ, Boscardin WJ, Dudley RA, et al. Adults with childhood-onset chronic conditions admitted to US pediatric and adult intensive care units. J Crit Care. 2015; 30:201–206. PMID: 25466316.
Article24. Chiron C, An I. Pharmacology aspects during transition and at transfer in patients with epilepsy. Epilepsia. 2014; 55:8–11. PMID: 25209078.
Article25. Affdal AO, Moutard ML, Billette de Villemeur T, Duchange N, Hervé C, Moutel G. A difficult transition from childhood to adult healthcare: the case of epilepsy. Arch Pediatr. 2015; 22:337–342. PMID: 25727476.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Out-of-hospital cardiac arrest: incidence, patient characteristics, outcomes, and trends over time between 2012 and 2018 in an urban city
- A Case of Transient Cortical Blindness after Cardiopulmonary Resuscitation
- The Impact of Middle East Respiratory Syndrome Outbreak on Trends in Emergency Department Utilization Patterns
- The Baiscs and the Prospect of Stem Cells for Pediatric Neurologic Diseases
- Statistical Studies of Pediatrics Emergency Room Patients