J Korean Assoc Oral Maxillofac Surg.
2018 Dec;44(6):289-292. 10.5125/jkaoms.2018.44.6.289.
Gingival crevicular fluid levels of sclerostin in chronic periodontitis and healthy subjects
- Affiliations
-
- 1Department of Periodontics, School of Dentistry, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
- 2Department of Dental Biomaterials, School of Dentistry, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
- 3School of Dentistry, Shahid Beheshti University of Medical Sciences, Tehran, Iran. s.kazemiveysari@gmail.com
- KMID: 2467176
- DOI: http://doi.org/10.5125/jkaoms.2018.44.6.289
Abstract
OBJECTIVES
Chronic periodontitis is a common inflammatory disease of the oral cavity that causes destruction of periodontal tissues and bone around the teeth. Sclerostin is a protein encoded by the SOST gene. In this study, gingival crevicular fluid (GCF) levels of sclerostin in patients with chronic periodontitis were compared with those of healthy subjects.
MATERIALS AND METHODS
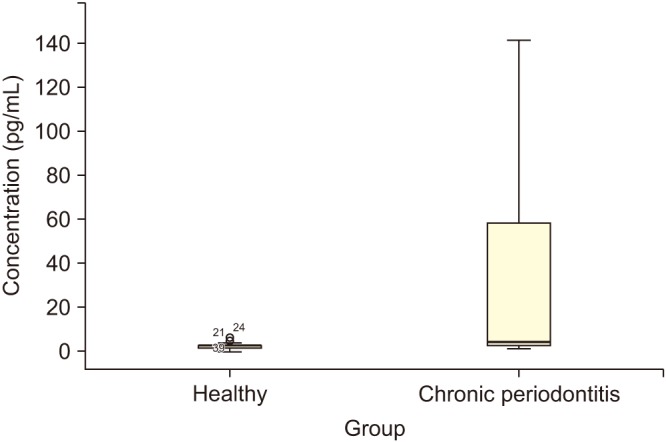
In this case-control study, a total of 40 subjects were enrolled and divided into the healthy group (n=23) and chronic periodontitis group (n=17). GCF samples were collected, and the concentration of sclerostin was evaluated using enzyme-linked immunosorbent assay. Comparison of significance between groups was assessed using Mann-Whitney U test.
RESULTS
Sclerostin concentration was significantly higher in the chronic periodontitis group compared with the healthy group (P < 0.005).
CONCLUSION
Despite the limitations of this study, sclerostin can be a possible marker for assessment of periodontal health status.
Keyword
MeSH Terms
Figure
Reference
-
1. Kornman KS, Page RC, Tonetti MS. The host response to the microbial challenge in periodontitis: assembling the players. Periodontol 2000. 1997; 14:33–53. PMID: 9567965.
Article2. Bascones-Martínez A, Muñoz-Corcuera M, Noronha S, Mota P, Bascones-Ilundain C, Campo-Trapero J. Host defence mechanisms against bacterial aggression in periodontal disease: basic mechanisms. Med Oral Patol Oral Cir Bucal. 2009; 14:e680–e685. PMID: 19680192.3. Kumar PS, Griffen AL, Barton JA, Paster BJ, Moeschberger ML, Leys EJ. New bacterial species associated with chronic periodontitis. J Dent Res. 2003; 82:338–344. PMID: 12709498.
Article4. Buduneli N, Kinane DF. Host-derived diagnostic markers related to soft tissue destruction and bone degradation in periodontitis. J Clin Periodontol. 2011; 38(Suppl 11):85–105. PMID: 21323706.
Article5. Champagne CM, Buchanan W, Reddy MS, Preisser JS, Beck JD, Offenbacher S. Potential for gingival crevice fluid measures as predictors of risk for periodontal diseases. Periodontol 2000. 2003; 31:167–180. PMID: 12657001.
Article6. Robling AG, Niziolek PJ, Baldridge LA, Condon KW, Allen MR, Alam I, et al. Mechanical stimulation of bone in vivo reduces osteocyte expression of Sost/sclerostin. J Biol Chem. 2008; 283:5866–5875. PMID: 18089564.
Article7. Winkler DG, Sutherland MK, Geoghegan JC, Yu C, Hayes T, Skonier JE, et al. Osteocyte control of bone formation via sclerostin, a novel BMP antagonist. EMBO J. 2003; 22:6267–6276. PMID: 14633986.
Article9. Poole KE, van Bezooijen RL, Loveridge N, Hamersma H, Papapoulos SE, Löwik CW, et al. Sclerostin is a delayed secreted product of osteocytes that inhibits bone formation. FASEB J. 2005; 19:1842–1844. PMID: 16123173.
Article10. Atkins GJ, Rowe PS, Lim HP, Welldon KJ, Ormsby R, Wijenayaka AR, et al. Sclerostin is a locally acting regulator of late-osteoblast/preosteocyte differentiation and regulates mineralization through a MEPE-ASARM-dependent mechanism. J Bone Miner Res. 2011; 26:1425–1436. PMID: 21312267.
Article11. Ren Y, Han X, Ho SP, Harris SE, Cao Z, Economides AN, et al. Removal of SOST or blocking its product sclerostin rescues defects in the periodontitis mouse model. FASEB J. 2015; 29:2702–2711. PMID: 25757567.
Article12. Balli U, Aydogdu A, Dede FO, Turer CC, Guven B. Gingival crevicular fluid levels of sclerostin, osteoprotegerin, and receptor activator of nuclear factor-κB ligand in periodontitis. J Periodontol. 2015; 86:1396–1404. PMID: 26367496.
Article13. Li X, Ominsky MS, Niu QT, Sun N, Daugherty B, D'Agostin D, et al. Targeted deletion of the sclerostin gene in mice results in increased bone formation and bone strength. J Bone Miner Res. 2008; 23:860–869. PMID: 18269310.
Article14. Griffiths GS. Formation, collection and significance of gingival crevice fluid. Periodontol 2000. 2003; 31:32–42. PMID: 12656994.
Article15. Li X, Ominsky MS, Warmington KS, Morony S, Gong J, Cao J, et al. Sclerostin antibody treatment increases bone formation, bone mass, and bone strength in a rat model of postmenopausal osteoporosis. J Bone Miner Res. 2009; 24:578–588. PMID: 19049336.
Article16. Ominsky MS, Vlasseros F, Jolette J, Smith SY, Stouch B, Doellgast G, et al. Two doses of sclerostin antibody in cynomolgus monkeys increases bone formation, bone mineral density, and bone strength. J Bone Miner Res. 2010; 25:948–959. PMID: 20200929.
Article17. Yang X, Han X, Shu R, Jiang F, Xu L, Xue C, et al. Effect of sclerostin removal in vivo on experimental periodontitis in mice. J Oral Sci. 2016; 58:271–276. PMID: 27349550.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Visualization of periodontopathic bacteria within crevicular epithelial cells with fluorescence in situ hybridization
- The Relationship between Periodontal Status and Alkaline Phosphatase Levels in Gingival Crevicular Fluid in Men with Hypergonadotropic Hypogonadism
- Effects of scaling and root planing with or without a local drug delivery system on the gingival crevicular fluid leptin level in chronic periodontitis patients: a clinico-biochemical study
- Analysis of Periodontitis Biomarker Expression in Gingival Crevicular Fluids
- The effect of vitamin-C containing neutraceutical on periodontal wound healing as an adjunct to non-surgical or surgical periodontal treatment