Korean J Radiol.
2020 Jan;21(1):15-24. 10.3348/kjr.2019.0176.
Automated Breast Ultrasound Screening for Dense Breasts
- Affiliations
-
- 1Department of Radiology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. rad-ksh@catholic.ac.kr
- 2Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 3Department of Radiology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2467038
- DOI: http://doi.org/10.3348/kjr.2019.0176
Abstract
- Mammography is the primary screening method for breast cancers. However, the sensitivity of mammographic screening is lower for dense breasts, which are an independent risk factor for breast cancers. Automated breast ultrasound (ABUS) is used as an adjunct to mammography for screening breast cancers in asymptomatic women with dense breasts. It is an effective screening modality with diagnostic accuracy comparable to that of handheld ultrasound (HHUS). Radiologists should be familiar with the unique display mode, imaging features, and artifacts in ABUS, which differ from those in HHUS. The purpose of this study was to provide a comprehensive review of the clinical significance of dense breasts and ABUS screening, describe the unique features of ABUS, and introduce the method of use and interpretation of ABUS.
Keyword
MeSH Terms
Figure
Reference
-
1. Niell BL, Freer PE, Weinfurtner RJ, Arleo EK, Drukteinis JS. Screening for breast cancer. Radiol Clin North Am. 2017; 55:1145–1162.
Article2. Oeffinger KC, Fontham ET, Etzioni R, Herzig A, Michaelson JS, Shih YC, et al. American Cancer Society. Breast cancer screening for women at average risk: 2015 guideline update From the American Cancer Society. JAMA. 2015; 314:1599–1614.3. Kim SH. A systematic review on radiologists' knowledge of breast cancer screening. J Korean Soc Radiol. 2019; 80:8–18.
Article4. Boyd NF, Martin LJ, Yaffe MJ, Minkin S. Mammographic density and breast cancer risk: current understanding and future prospects. Breast Cancer Res. 2011; 13:223.
Article5. Rajaram N, Mariapun S, Eriksson M, Tapia J, Kwan PY, Ho WK, et al. Differences in mammographic density between Asian and Caucasian populations: a comparative analysis. Breast Cancer Res Treat. 2017; 161:353–362.
Article6. Brem RF, Lenihan MJ, Lieberman J, Torrente J. Screening breast ultrasound: past, present, and future. AJR Am J Roentgenol. 2015; 204:234–240.
Article7. Kim SH, Kang BJ, Choi BG, Choi JJ, Lee JH, Song BJ, et al. Radiologists' performance for detecting lesions and the interobserver variability of automated whole breast ultrasound. Korean J Radiol. 2013; 14:154–163.
Article8. Kaplan SS. Automated whole breast ultrasound. Radiol Clin North Am. 2014; 52:539–546.
Article9. Rella R, Belli P, Giuliani M, Bufi E, Carlino G, Rinaldi P, et al. Automated breast ultrasonography (ABUS) in the screening and diagnostic setting: indications and practical use. Acad Radiol. 2018; 25:1457–1470.10. Kim SH. Image quality and artifacts in automated breast ultrasonography. Ultrasonography. 2019; 38:83–91.
Article11. Sprague BL, Gangnon RE, Burt V, Trentham-Dietz A, Hampton JM, Wellman RD, et al. Prevalence of mammographically dense breasts in the United States. J Natl Cancer Inst. 2014; 106:dju255.
Article12. Kim YJ, Lee EH, Jun JK, Shin DR, Park YM, Kim HW, et al. Alliance for Breast Cancer Screening in Korea (ABCS-K). Analysis of participant factors that affect the diagnostic performance of screening mammography: a report of the Alliance for Breast Cancer Screening in Korea. Korean J Radiol. 2017; 18:624–631.
Article13. Freer PE. Mammographic breast density: impact on breast cancer risk and implications for screening. Radiographics. 2015; 35:302–315.
Article14. Sprague BL, Conant EF, Onega T, Garcia MP, Beaber EF, Herschorn SD, et al. PROSPR Consortium. Variation in mammographic breast density assessments among radiologists in clinical practice: a multicenter observational study. Ann Intern Med. 2016; 165:457–464.15. Yaghjyan L, Colditz GA, Rosner B, Tamimi RM. Mammographic breast density and breast cancer risk: interactions of percent density, absolute dense, and non-dense areas with breast cancer risk factors. Breast Cancer Res Treat. 2015; 150:181–189.
Article16. Boyd NF, Byng JW, Jong RA, Fishell EK, Little LE, Miller AB, et al. Quantitative classification of mammographic densities and breast cancer risk: results from the Canadian National Breast Screening Study. J Natl Cancer Inst. 1995; 87:670–675.
Article17. McCormack VA, dos Santos Silva I. Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2006; 15:1159–1169.
Article18. Park B, Cho HM, Lee EH, Song S, Suh M, Choi KS, et al. Does breast density measured through population-based screening independently increase breast cancer risk in Asian females? Clin Epidemiol. 2018; 10:61–70.
Article19. Weigert J, Steenbergen S. The Connecticut experiment: the role of ultrasound in the screening of women with dense breasts. Breast J. 2012; 18:517–522.
Article20. Expert Panel on Breast Imaging. Mainiero MB, Moy L, Baron P, Didwania AD, diFlorio RM, Green ED, et al. ACR Appropriateness Criteria® breast cancer screening. J Am Coll Radiol. 2017; 14:S383–S390.21. Lee EH, Park B, Kim NS, Seo HJ, Ko KL, Min JW, et al. The Korean guideline for breast cancer screening. J Korean Med Assoc. 2015; 58:408–419.
Article22. Ohuchi N, Suzuki A, Sobue T, Kawai M, Yamamoto S, Zheng YF, et al. J-START investigator groups. Sensitivity and specificity of mammography and adjunctive ultrasonography to screen for breast cancer in the Japan strategic anti-cancer randomized trial (J-START): a randomised controlled trial. Lancet. 2016; 387:341–348.
Article23. Berg WA, Zhang Z, Lehrer D, Jong RA, Pisano ED, Barr RG, et al. ACRIN 6666 Investigators. Detection of breast cancer with addition of annual screening ultrasound or a single screening MRI to mammography in women with elevated breast cancer risk. JAMA. 2012; 307:1394–1404.
Article24. Kelly KM, Dean J, Comulada WS, Lee SJ. Breast cancer detection using automated whole breast ultrasound and mammography in radiographically dense breasts. Eur Radiol. 2010; 20:734–742.
Article25. Brem RF, Tabár L, Duffy SW, Inciardi MF, Guingrich JA, Hashimoto BE, et al. Assessing improvement in detection of breast cancer with three-dimensional automated breast US in women with dense breast tissue: the SomoInsight study. Radiology. 2015; 274:663–673.
Article26. Wilczek B, Wilczek HE, Rasouliyan L, Leifland K. Adding 3D automated breast ultrasound to mammography screening in women with heterogeneously and extremely dense breasts: report from a hospital-based, high-volume, single-center breast cancer screening program. Eur J Radiol. 2016; 85:1554–1563.
Article27. Giuliano V, Giuliano C. Improved breast cancer detection in asymptomatic women using 3D-automated breast ultrasound in mammographically dense breasts. Clin Imaging. 2013; 37:480–486.
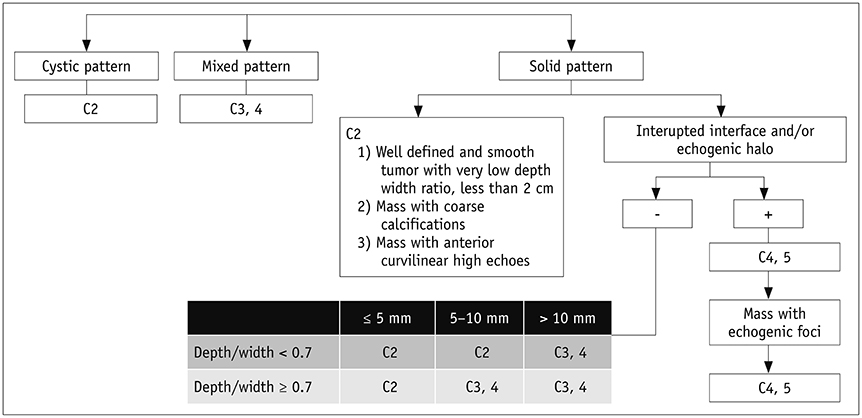
Article28. Japanese Association of Breast and Thyroid Sonology. Guidelines for breast ultrasound diagnosis. 3rd ed. Tokyo: Nankodo;2014. p. 111–123.29. Ban K, Tsunoda H, Suzuki S, Takaki R, Sasaki K, Nakagawa M. Verification of recall criteria for masses detected on ultrasound breast cancer screening. J Med Ultrason (2001). 2018; 45:65–73.
Article30. Barr RG, Zhang Z, Cormack JB, Mendelson EB, Berg WA. Probably benign lesions at screening breast US in a population with elevated risk: prevalence and rate of malignancy in the ACRIN 6666 trial. Radiology. 2013; 269:701–712.
Article31. Berg WA, Zhang Z, Cormack JB, Mendelson EB. Multiple bilateral circumscribed masses at screening breast US: consider annual follow-up. Radiology. 2013; 268:673–683.
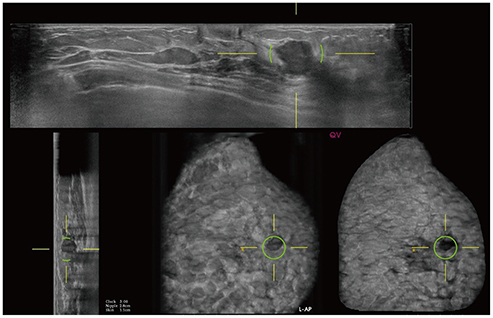
Article32. Gazhonova V. 3D automated breast volume sonography: a practical guide. Berlin: Springer;2015. p. 11–12.33. Chae EY, Shin HJ, Kim HJ, Yoo H, Baek S, Cha JH, et al. Diagnostic performance of automated breast ultrasound as a replacement for a hand-held second-look ultrasound for breast lesions detected initially on magnetic resonance imaging. Ultrasound Med Biol. 2013; 39:2246–2254.
Article34. Li N, Jiang YX, Zhu QL, Zhang J, Dai Q, Liu H, et al. Accuracy of an automated breast volume ultrasound system for assessment of the pre-operative extent of pure ductal carcinoma in situ: comparison with a conventional handheld ultrasound examination. Ultrasound Med Biol. 2013; 39:2255–2263.
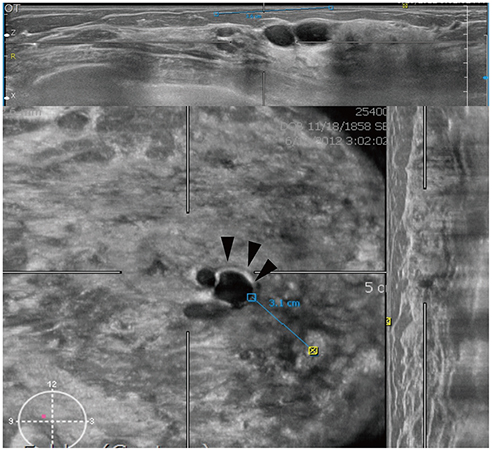
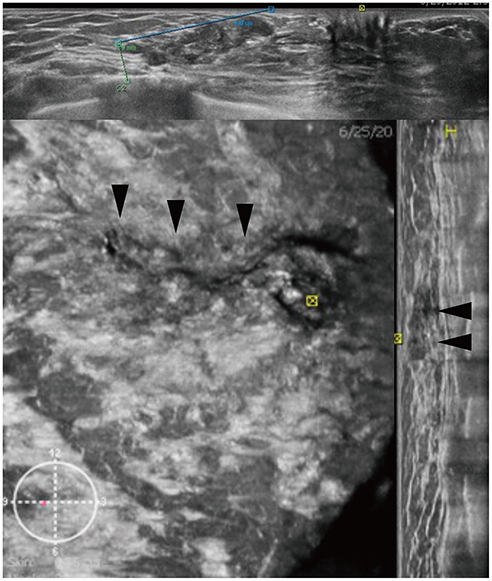
Article35. van Zelst JCM, Mann RM. Automated three-dimensional breast US for screening: technique, artifacts, and lesion characterization. Radiographics. 2018; 38:663–683.
Article36. Skaane P, Gullien R, Eben EB, Sandhaug M, Schulz-Wendtland R, Stoeblen F. Interpretation of automated breast ultrasound (ABUS) with and without knowledge of mammography: a reader performance study. Acta Radiol. 2015; 56:404–412.
Article37. Chae EY, Cha JH, Kim HH, Shin HJ. Comparison of lesion detection in the transverse and coronal views on automated breast sonography. J Ultrasound Med. 2015; 34:125–135.
Article38. Vourtsis A, Kachulis A. The performance of 3D ABUS versus HHUS in the visualisation and BI-RADS characterisation of breast lesions in a large cohort of 1,886 women. Eur Radiol. 2018; 28:592–601.
Article39. Zheng FY, Yan LX, Huang BJ, Xia HS, Wang X, Lu Q, et al. Comparison of retraction phenomenon and BI-RADS-US descriptors in differentiating benign and malignant breast masses using an automated breast volume scanner. Eur J Radiol. 2015; 84:2123–2129.
Article40. Zhang J, Lai XJ, Zhu QL, Wang HY, Jiang YX, Liu H, et al. Interobserver agreement for sonograms of breast lesions obtained by an automated breast volume scanner. Eur J Radiol. 2012; 81:2179–2183.
Article41. Grubstein A, Rapson Y, Gadiel I, Cohen M. Analysis of false-negative readings of automated breast ultrasound studies. J Clin Ultrasound. 2017; 45:245–251.
Article42. van Zelst JCM, Tan T, Platel B, de Jong M, Steenbakkers A, Mourits M, et al. Improved cancer detection in automated breast ultrasound by radiologists using computer aided detection. Eur J Radiol. 2017; 89:54–59.
Article43. Jiang Y, Inciardi MF, Edwards AV, Papaioannou J. Interpretation time using a concurrent-read computer-aided detection system for automated breast ultrasound in breast cancer screening of women with dense breast tissue. AJR Am J Roentgenol. 2018; 211:452–461.
Article44. Xu X, Bao L, Tan Y, Zhu L, Kong F, Wang W. 1000-case reader study of radiologists' performance in interpretation of automated breast volume scanner images with a computer-aided detection system. Ultrasound Med Biol. 2018; 44:1694–1702.
Article45. van Zelst JCM, Tan T, Clauser P, Domingo A, Dorrius MD, Drieling D, et al. Dedicated computer-aided detection software for automated 3D breast ultrasound; an efficient tool for the radiologist in supplemental screening of women with dense breasts. Eur Radiol. 2018; 28:2996–3006.
Article46. Weigert JM. The Connecticut experiment; the third installment: 4 years of screening women with dense breasts with bilateral ultrasound. Breast J. 2017; 23:34–39.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Automated Breast Ultrasound
- Breast Cancer Screening in Korean Woman with Dense Breast Tissue
- Clinical Application of Automated Breast Ultrasound
- Distribution of dense breasts using screening mammography in Korean women: a retrospective observational study
- A Technical Note on a Novel Technique for the Evaluation of Breast Excision Specimen: Automated Breast Ultrasound System