J Endocr Surg.
2019 Dec;19(4):126-135. 10.16956/jes.2019.19.4.126.
Changing Trends in Preoperative Localization and Surgical Techniques for the Treatment of Primary Hyperparathyroidism in a Single Tertiary Center
- Affiliations
-
- 1Department of Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. kyueunlee@snu.ac.kr
- 2Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- 3Division of Surgery, Thyroid Center, Seoul National University Cancer Hospital, Seoul, Korea.
- 4Department of Surgery, Seoul National University Bundang Hospital, Seongnam, Korea.
- 5Department of Surgery, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea.
- KMID: 2466238
- DOI: http://doi.org/10.16956/jes.2019.19.4.126
Abstract
- PURPOSE
Primary hyperparathyroidism (PHPT) is caused by the oversecretion of parathyroid hormone (PTH), resulting in increased serum calcium levels. The aim of this study was to analyze changing trends in preoperative localization and surgical techniques for the treatment of PHPT in a single tertiary center in Korea.
METHODS
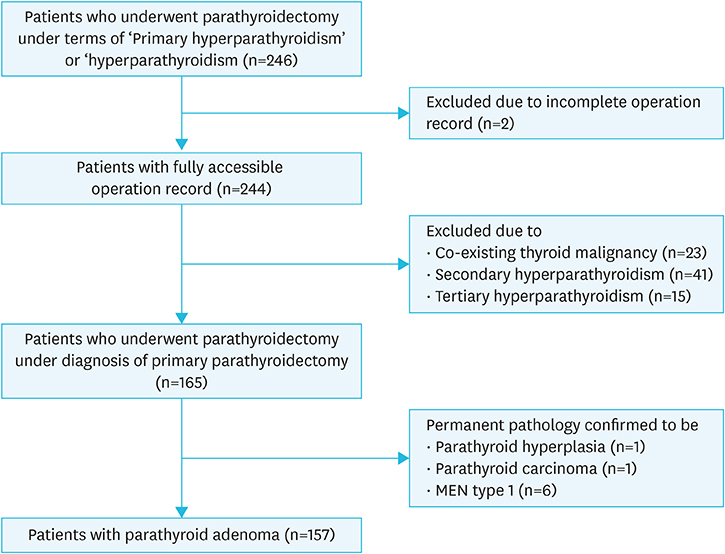
Data from patients with PHPT who had undergone parathyroidectomy between January 2000 and December 2016 were evaluated in this retrospective analysis.
RESULTS
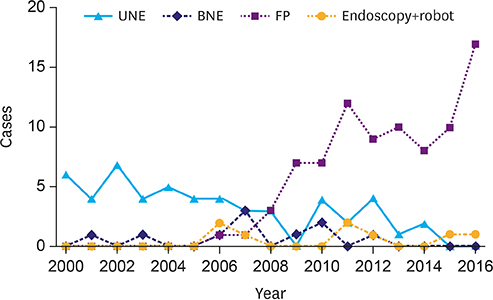
Data from 157 patients were included in this analysis (single adenoma n=156, double adenoma n=1). A total of 134 patients underwent ultrasonography for preoperative localization, 110 of which were marked preoperatively. Preoperative localization by sonographic marking increased over time following its introduction in 2006. Intraoperative PTH assay was used in 80 patients, with its use also increasing each year since it was introduced in 2011. In addition, 150 patients underwent 99mTc-sestamibi scan and 148 underwent computed tomography (CT) scanning. Four-dimensional CT and 99mTc-sestamibi SPECT/CT (SeS) was introduced in 2011 and replaced the use of 2-dimensional CT and 99mTc-sestamibi scan over time. Statistical analysis revealed that sonographic marking, SeS, CT, intraoperative PTH significantly reduce operation time. Surgical techniques used were bilateral neck exploration (n=11), unilateral neck exploration (n=54), focused parathyroidectomy (n=84), and others (n=8). Among 5 surgical technique, focused parathyroidectomy took significantly lesser operation time than other surgical methods.
CONCLUSION
In order to reduce operation time, sonographic marking, SeS, CT, intraoperative PTH should be performed perioperatively, and focused parathyroidectomy could be the first choice of surgical methods.
MeSH Terms
Figure
Reference
-
1. Marcocci C, Cetani F. Clinical practice. Primary hyperparathyroidism. N Engl J Med. 2011; 365:2389–2397.2. Wermers RA, Khosla S, Atkinson EJ, Achenbach SJ, Oberg AL, Grant CS, et al. Incidence of primary hyperparathyroidism in Rochester, Minnesota, 1993–2001: an update on the changing epidemiology of the disease. J Bone Miner Res. 2006; 21:171–177.
Article3. Kim JK, Chai YJ, Chung JK, Hwang KT, Heo SC, Kim SJ, et al. The prevalence of primary hyperparathyroidism in Korea: a population-based analysis from patient medical records. Ann Surg Treat Res. 2018; 94:235–239.
Article4. Ciappuccini R, Morera J, Pascal P, Rame JP, Heutte N, Aide N, et al. Dual-phase 99mTc sestamibi scintigraphy with neck and thorax SPECT/CT in primary hyperparathyroidism: a single-institution experience. Clin Nucl Med. 2012; 37:223–228.
Article5. Bilezikian JP, Khan AA, Potts JT Jr. Third International Workshop on the Management of Asymptomatic Primary Hyperthyroidism. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the third international workshop. J Clin Endocrinol Metab. 2009; 94:335–339.
Article6. Langdahl BL, Ralston SH. Diagnosis and management of primary hyperparathyroidism in Europe. QJM. 2012; 105:519–525.
Article7. Mohebati A, Shaha AR. Imaging techniques in parathyroid surgery for primary hyperparathyroidism. Am J Otolaryngol. 2012; 33:457–468.
Article8. Yen TW, Wang TS, Doffek KM, Krzywda EA, Wilson SD. Reoperative parathyroidectomy: an algorithm for imaging and monitoring of intraoperative parathyroid hormone levels that results in a successful focused approach. Surgery. 2008; 144:611–619.
Article9. Suh YJ, Kim SJ, Lee KE, Youn YK. Localization of parathyroid adenoma and minimally invasive parathyroidectomy: a review. Korean J Endocr Surg. 2014; 14:138–143.
Article10. Kunstman JW, Udelsman R. Superiority of minimally invasive parathyroidectomy. Adv Surg. 2012; 46:171–189.
Article11. Udelsman R, Lin Z, Donovan P. The superiority of minimally invasive parathyroidectomy based on 1650 consecutive patients with primary hyperparathyroidism. Ann Surg. 2011; 253:585–591.
Article12. Miccoli P, Materazzi G, Baggiani A, Miccoli M. Mini-invasive video-assisted surgery of the thyroid and parathyroid glands: a 2011 update. J Endocrinol Invest. 2011; 34:473–480.
Article13. D'Agostino J, Diana M, Vix M, Nicolau S, Soler L, Bourhala K, et al. Three-dimensional metabolic and radiologic gathered evaluation using VR-RENDER fusion: a novel tool to enhance accuracy in the localization of parathyroid adenomas. World J Surg. 2013; 37:1618–1625.14. Suh YJ, Choi JY, Kim SJ, Chun IK, Yun TJ, Lee KE, et al. Comparison of 4D CT, ultrasonography, and 99mTc sestamibi SPECT/CT in localizing single-gland primary hyperparathyroidism. Otolaryngol Head Neck Surg. 2015; 152:438–443.
Article15. Irvin GL, Molinari AS, Carneiro DM, Rivabem F, Ruel MM, Boggs JE. Parathyroidectomy: new criteria for evaluating outcome. Am Surg. 1999; 65:1186–1188.16. Scott-Conner CE, Dawson DL. Operative Anatomy. 1st ed. Philadelphia (PA): J.B. Lippincott Company;1993.17. Slepavicius A, Beisa V, Janusonis V, Strupas K. Focused versus conventional parathyroidectomy for primary hyperparathyroidism: a prospective, randomized, blinded trial. Langenbecks Arch Surg. 2008; 393:659–666.
Article18. Abbott DE, Cantor SB, Grubbs EG, Santora R, Gomez HF, Evans DB, et al. Outcomes and economic analysis of routine preoperative 4-dimensional CT for surgical intervention in de novo primary hyperparathyroidism: does clinical benefit justify the cost? J Am Coll Surg. 2012; 214:629–637.
Article19. Rodgers SE, Hunter GJ, Hamberg LM, Schellingerhout D, Doherty DB, Ayers GD, et al. Improved preoperative planning for directed parathyroidectomy with 4-dimensional computed tomography. Surgery. 2006; 140:932–940.
Article20. LeBlanc RA, Isaac A, Abele J, Biron VL, Côté DW, Hearn M, et al. Validation of a novel method for localization of parathyroid adenomas using SPECT/CT. J Otolaryngol Head Neck Surg. 2018; 47:65.
Article21. Moreno MA, Callender GG, Woodburn K, Edeiken-Monroe BS, Grubbs EG, Evans DB, et al. Common locations of parathyroid adenomas. Ann Surg Oncol. 2011; 18:1047–1051.
Article22. Kluijfhout WP, Pasternak JD, Beninato T, Drake FT, Gosnell JE, Shen WT, et al. Diagnostic performance of computed tomography for parathyroid adenoma localization; a systematic review and meta-analysis. Eur J Radiol. 2017; 88:117–128.
Article23. Dasgupta DJ, Navalkissoor S, Ganatra R, Buscombe J. The role of single-photon emission computed tomography/computed tomography in localizing parathyroid adenoma. Nucl Med Commun. 2013; 34:621–626.
Article24. Cheung K, Wang TS, Farrokhyar F, Roman SA, Sosa JA. A meta-analysis of preoperative localization techniques for patients with primary hyperparathyroidism. Ann Surg Oncol. 2012; 19:577–583.
Article25. Butt HZ, Husainy MA, Bolia A, London NJ. Ultrasonography alone can reliably locate parathyroid tumours and facilitates minimally invasive parathyroidectomy. Ann R Coll Surg Engl. 2015; 97:420–424.
Article26. Ruda JM, Hollenbeak CS, Stack BC Jr. A systematic review of the diagnosis and treatment of primary hyperparathyroidism from 1995 to 2003. Otolaryngol Head Neck Surg. 2005; 132:359–372.
Article27. Lappas D, Noussios G, Anagnostis P, Adamidou F, Chatzigeorgiou A, Skandalakis P. Location, number and morphology of parathyroid glands: results from a large anatomical series. Anat Sci Int. 2012; 87:160–164.
Article28. Phitayakorn R, McHenry CR. Incidence and location of ectopic abnormal parathyroid glands. Am J Surg. 2006; 191:418–423.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Parathyroidectomy without an Intraoperative i-PTH Test for Patients with Primary Hyperparathyroidism
- Clinical Review of Primary Hyperparathyroidism
- A Case of Primary Hyperparathyroidism Caused by Solitary Parathyroid Adenoma That was Not Detected by Both Ultrasonography and Sestamibi Scan
- Update on Preoperative Parathyroid Localization in Primary Hyperparathyroidism
- Minimally Invasive Focused Parathyroidectomy (MIFP)