J Korean Ophthalmol Soc.
2019 Dec;60(12):1295-1300. 10.3341/jkos.2019.60.12.1295.
Loss of Reflex Tearing after Maxillary Orthognathic Surgery Case Report and Literature Review
- Affiliations
-
- 1Department of Ophthalmology, Chonbuk National University Medical School, Jeonju, Korea. ahnmin@jbnu.ac.kr
- 2Research Institute of Clinical Medicine, Chonbuk National University, Jeonju, Korea.
- 3Biomedical Research Institute, Chonbuk National University Hospital, Jeonju, Korea.
- KMID: 2466185
- DOI: http://doi.org/10.3341/jkos.2019.60.12.1295
Abstract
- PURPOSE
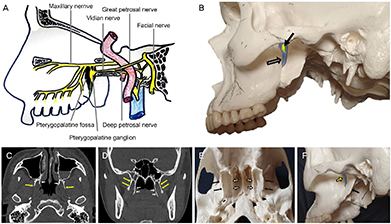
To report a case of unilateral loss of reflex tearing after double-jaw surgery with anatomy and mechanism.
CASE SUMMARY
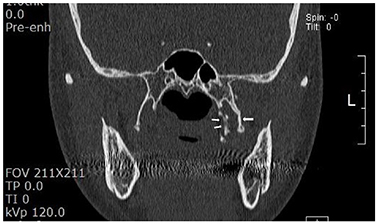
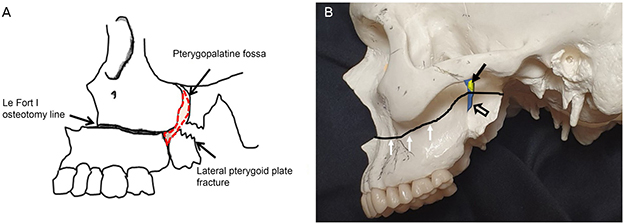
A 32-year-old woman complained of a 3-year history of loss of tearing in her left eye. She had undergone double-jaw surgery 3 years prior to correct her malocclusion. In orbital computed tomography (CT) images, there were no specific findings, with the exception of a fractured left pterygoid plate, possibly caused by the double-jaw surgery. The tear break-up times of both eyes were similar, with non-specific findings on slit lamp examination. We diagnosed loss of reflex tearing due to pterygopalatine ganglion injury based on her history, physical examination and orbital CT findings.
CONCLUSIONS
Nerve damage due to artificial fracture may occur during double-jaw surgery and may result in loss of reflex tearing, thus, pre-operative evaluation of basic lacrimal secretion and a reflex tearing test are important. Once the loss of reflex tearing due to nerve injury occurrs, orbital CT scans are needed for diagnosis. Ophthalmologist examination is necessary to confirm the mechanism of loss of reflex tearing and changes in the anatomical structure.
MeSH Terms
Figure
Reference
-
1. Buchanan EP, Hyman CH. LeFort I osteotomy. Semin Plast Surg. 2013; 27:149–154.2. Lanigan DT, Hey JH, West RA. Major vascular complications of orthognathic surgery: hemorrhage associated with Le Fort I osteotomies. J Oral Maxillofac Surg. 1990; 48:561–573.3. Kim S, Kim SY, Kim GJ, et al. Partial necrosis of the mandibular proximal segment following transoral vertical ramus osteotomy. Maxillofac Plast Reconstr Surg. 2014; 36:131–134.4. Lanigan DT, Romanchuk K, Olson CK. Ophthalmic complications associated with orthognathic surgery. J Oral Maxillofac Surg. 1993; 51:480–494.5. Tomasetti BJ, Broutsas M, Gormley M, Jarrett W. Lack of tearing after Le Fort I osteotomy. J Oral Surg. 1976; 34:1095–1097.6. Ord RA. Post-operative retrobulbar haemorrhage and blindness complicating trauma surgery. Br J Oral Surg. 1981; 19:202–207.7. Agbaje JO, Salem AS, Lambrichts I, et al. Systematic review of the incidence of inferior alveolar nerve injury in bilateral sagittal split osteotomy and the assessment of neurosensory disturbances. Int J Oral Maxillofac Surg. 2015; 44:447–451.8. Kang S, Jang SY, Lee A, Jang JW. Loss of reflex tearing after maxillary orthognathic surgery: a report of two cases. BMC Ophthalmol. 2014; 14:37.9. Koizumi K, Suda I. Induced modulation in autonomic efferent neuron activity. Am J Physiol. 1963; 205:738–744.10. Langley JN, Dickinson WL. On the local paralysis of the peripheral ganglia and on the connection of different classes of nerve fibres with them. Proc R Soc Lond. 1890; 46:423–431.11. Shoshani Y, Samet N, Ardekian L, Taicher S. Nasolacrimal duct injury after Le Fort I osteotomy. J Oral Maxillofac Surg. 1994; 52:406–407.12. Jang SY, Kim MK, Choi SM, Jang JW. Nasolacrimal duct obstruction after maxillary orthognathic surgery. J Oral Maxillofac Surg. 2013; 71:1085–1098.13. Kim JW, Chin BR, Park HS, et al. Cranial nerve injury after Le Fort I osteotomy. Int J Oral Maxillofac Surg. 2011; 40:327–329.14. Chrcanovic BR, Custódio AL. Optic, oculomotor, abducens, and facial nerve palsies after combined maxillary and mandibular osteotomy: case report. J Oral Maxillofac Surg. 2011; 69:e234–e241.15. Cruz AA, dos Santos AC. Blindness after Le Fort I osteotomy: a possible complication associated with pterygomaxillary separation. J Craniomaxillofac Surg. 2006; 34:210–216.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical ciliated cyst of the mandible after orthognathic surgery: a case report with review of the literature
- Removal of fungus ball of the right maxillary sinus via LeFort I osteotomy: A case report
- Bilateral postoperative maxillary cysts after orthognathic surgery: A case report
- Massive Postoperative Bleeding: A Case Report
- Post-Operative Maxillary Cyst after Maxillary Orthognathic Surgery: Report of an Unusual Case