J Periodontal Implant Sci.
2019 Dec;49(6):346-354. 10.5051/jpis.2019.49.6.346.
Points to consider before the insertion of maxillary implants: the otolaryngologist's perspective
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea. dohyuni9292@naver.com
- KMID: 2465379
- DOI: http://doi.org/10.5051/jpis.2019.49.6.346
Abstract
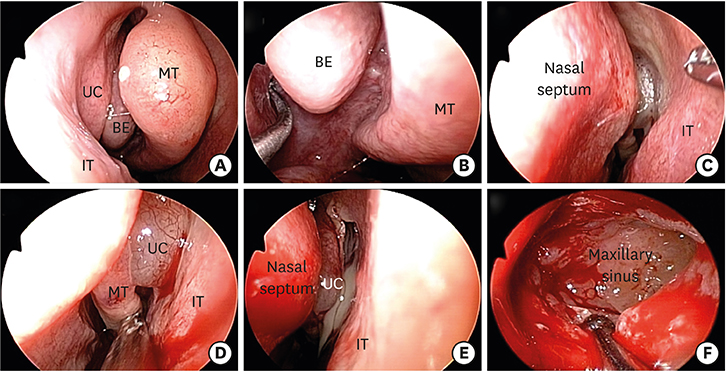
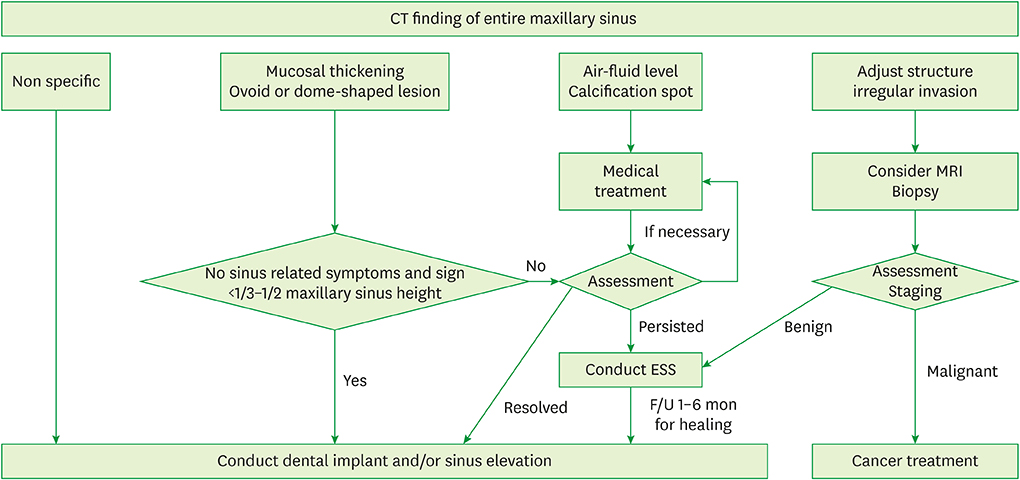
- Maxillary implants are inserted in the upward direction, meaning that they oppose gravity, and achieving stable support is difficult if the alveolar bone facing the maxillary sinus is thin. Correspondingly, several sinus-lifting procedures conducted with or without bone graft materials have been used to place implants in the posterior area of the maxilla. Even with these procedures available, it has been reported that in about 5% of cases, complications occurred after implantation, including acute and chronic sinusitis, penetration of the sinus by the implant, implant dislocation, oroantral fistula formation, infection, bone graft dislocation, foreign-body reaction, Schneiderian membrane perforation, and ostium plugging by a dislodged bone graft. This review summarizes common maxillary sinus pathologies related to implants and suggests an appropriate management plan for patients requiring dental implantation.
MeSH Terms
Figure
Reference
-
1. Hunter WL 4th, Bradrick JP, Houser SM, Patel JB, Sawady J. Maxillary sinusitis resulting from ostium plugging by dislodged bone graft: case report. J Oral Maxillofac Surg. 2009; 67:1495–1498.
Article2. Kim JW, Lee CH, Kwon TK, Kim DK. Endoscopic removal of a dental implant through a middle meatal antrostomy. Br J Oral Maxillofac Surg. 2007; 45:408–409.
Article3. Lopatin AS, Sysolyatin SP, Sysolyatin PG, Melnikov MN. Chronic maxillary sinusitis of dental origin: is external surgical approach mandatory? Laryngoscope. 2002; 112:1056–1059.
Article4. Manor Y, Mardinger O, Bietlitum I, Nashef A, Nissan J, Chaushu G. Late signs and symptoms of maxillary sinusitis after sinus augmentation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 110:e1–4.
Article5. Timmenga NM, Raghoebar GM, van Weissenbruch R, Vissink A. Maxillary sinusitis after augmentation of the maxillary sinus floor: a report of 2 cases. J Oral Maxillofac Surg. 2001; 59:200–204.
Article6. Zimbler MS, Lebowitz RA, Glickman R, Brecht LE, Jacobs JB. Antral augmentation, osseointegration, and sinusitis: the otolaryngologist's perspective. Am J Rhinol. 1998; 12:311–316.
Article7. Kim JS, Choi SM, Yoon JH, Lee EJ, Yoon J, Kwon SH, et al. What affects postoperative sinusitis and implant failure after dental implant: a meta-analysis. Otolaryngol Head Neck Surg. 2019; 160:974–984.
Article8. Kozuma A, Sasaki M, Seki K, Toyoshima T, Nakano H, Mori Y. Preoperative chronic sinusitis as significant cause of postoperative infection and implant loss after sinus augmentation from a lateral approach. Oral Maxillofac Surg. 2017; 21:193–200.
Article9. Regev E, Smith RA, Perrott DH, Pogrel MA. Maxillary sinus complications related to endosseous implants. Int J Oral Maxillofac Implants. 1995; 10:451–461.10. Small SA, Zinner ID, Panno FV, Shapiro HJ, Stein JI. Augmenting the maxillary sinus for implants: report of 27 patients. Int J Oral Maxillofac Implants. 1993; 8:523–528.11. Smiler DG, Johnson PW, Lozada JL, Misch C, Rosenlicht JL, Tatum OH Jr, et al. Sinus lift grafts and endosseous implants. Treatment of the atrophic posterior maxilla. Dent Clin North Am. 1992; 36:151–186.12. Zinreich SJ. Imaging of chronic sinusitis in adults: X-ray, computed tomography, and magnetic resonance imaging. J Allergy Clin Immunol. 1992; 90:445–451.
Article13. Mardinger O, Manor I, Mijiritsky E, Hirshberg A. Maxillary sinus augmentation in the presence of antral pseudocyst: a clinical approach. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 103:180–184.
Article14. Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F, et al. European position paper on rhinosinusitis and nasal polyps 2012. Rhinol Suppl. 2012; 23:3 p preceding table of contents1–298.15. Benninger MS, Anon J, Mabry RL. The medical management of rhinosinusitis. Otolaryngol Head Neck Surg. 1997; 117:S41–9.
Article16. Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, Brook I, Ashok Kumar K, Kramper M, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg. 2015; 152:S1–39.
Article17. Williams JW Jr, Simel DL, Roberts L, Samsa GP. Clinical evaluation for sinusitis. Making the diagnosis by history and physical examination. Ann Intern Med. 1992; 117:705–710.18. Kenealy T, Arroll B. Antibiotics for the common cold and acute purulent rhinitis. Cochrane Database Syst Rev. 2013; CD000247.
Article19. Chow AW, Benninger MS, Brook I, Brozek JL, Goldstein EJ, Hicks LA, et al. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012; 54:e72–e112.
Article20. Dhong HJ, Jung JY, Park JH. Diagnostic accuracy in sinus fungus balls: CT scan and operative findings. Am J Rhinol. 2000; 14:227–231.
Article21. Pignataro L, Mantovani M, Torretta S, Felisati G, Sambataro G. ENT assessment in the integrated management of candidate for (maxillary) sinus lift. Acta Otorhinolaryngol Ital. 2008; 28:110–119.22. Dubin MG, Liu C, Lin SY, Senior BA. American Rhinologic Society member survey on “maximal medical therapy” for chronic rhinosinusitis. Am J Rhinol. 2007; 21:483–488.
Article23. Snidvongs K, Kalish L, Sacks R, Craig JC, Harvey RJ. Topical steroid for chronic rhinosinusitis without polyps. Cochrane Database Syst Rev. 2011; CD009274.
Article24. Chong LY, Head K, Hopkins C, Philpott C, Glew S, Scadding G, et al. Saline irrigation for chronic rhinosinusitis. Cochrane Database Syst Rev. 2016; CD011995.
Article25. Chan HL, Wang HL. Sinus pathology and anatomy in relation to complications in lateral window sinus augmentation. Implant Dent. 2011; 20:406–412.
Article26. Chen YW, Lee FY, Chang PH, Huang CC, Fu CH, Huang CC, et al. A paradigm for evaluation and management of the maxillary sinus before dental implantation. Laryngoscope. 2018; 128:1261–1267.
Article27. Pazera P, Bornstein MM, Pazera A, Sendi P, Katsaros C. Incidental maxillary sinus findings in orthodontic patients: a radiographic analysis using cone-beam computed tomography (CBCT). Orthod Craniofac Res. 2011; 14:17–24.
Article28. Manji A, Faucher J, Resnik RR, Suzuki JB. Prevalence of maxillary sinus pathology in patients considered for sinus augmentation procedures for dental implants. Implant Dent. 2013; 22:428–435.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Role of Otolaryngology in Dental Implantation
- Disappearance of a dental implant after migration into the maxillary sinus: an unusual case
- A Case of Maxillary Sinusitis after Sinus Floor Augmentation
- A Retrospective study of the Cumulative Survival Rate and change of peri-implant marginal bone around implants associated with maxillary sinus augmentation
- Clinical study on success rate of microscrew implants for orthodontic anchorage