Korean J Ophthalmol.
2019 Dec;33(6):539-546. 10.3341/kjo.2019.0045.
Long-term Outcomes of Macular Hole Retinal Detachment in Highly Myopic Eyes after Surgical Reattachment
- Affiliations
-
- 1Department of Ophthalmology, Pusan National University School of Medicine, Yangsan, Korea. jlee@pusan.ac.kr
- 2Biomedical Research Institute, Pusan National University Hospital, Busan, Korea.
- 3Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea.
- KMID: 2465134
- DOI: http://doi.org/10.3341/kjo.2019.0045
Abstract
- PURPOSE
To evaluate visual acuity changes over 3 years following surgical reattachment of macular hole retinal detachment (MHRD) developed in high myopia.
METHODS
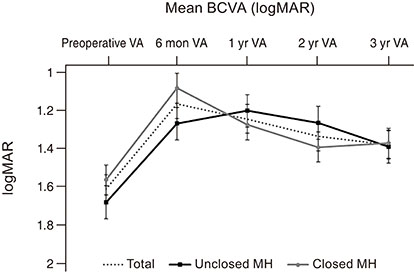
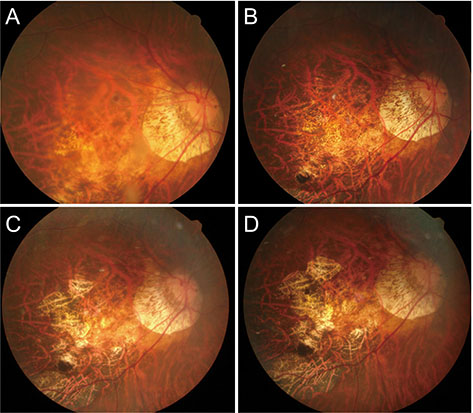
A retrospective analysis was performed using the medical records of patients with highly myopic eyes who underwent pars plana vitrectomy with internal limiting membrane peeling or the internal limiting membrane flap technique for MHRD. Changes in best-corrected visual acuity (BCVA) were measured at baseline, 6 months, 1 year, 2 years, and 3 years.
RESULTS
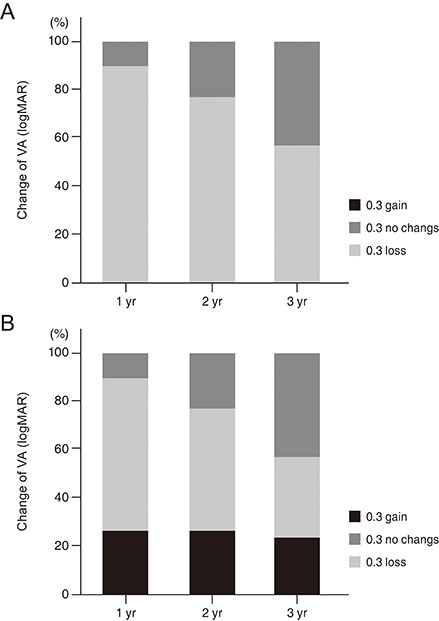
Of the 22 eyes analyzed, macular hole was closed in 13 and unclosed in nine. BCVA significantly improved from 1.61 ± 0.39 logarithm of the minimum angle of resolution (logMAR) at baseline to 1.17 ± 0.43 logMAR at 6 months and 1.33 ± 0.48 logMAR at 2 years after MHRD surgery. At 3 years, BCVA significantly decreased compared with that at 6 months, and visual improvement from baseline was not significant. BCVA and proportion of vision loss ≥0.3 logMAR were not different between the closed and unclosed macular hole groups.
CONCLUSIONS
Visual improvement after surgical reattachment of MHRD in high myopia was not maintained, and favorable macular hole closure effects were not observed at 3-year follow-up.
MeSH Terms
Figure
Reference
-
1. Siam A. Macular hole with central retinal detachment in high myopia with posterior staphyloma. Br J Ophthalmol. 1969; 53:62–63.2. Akiba J, Konno S, Yoshida A. Retinal detachment associated with a macular hole in severely myopic eyes. Am J Ophthalmol. 1999; 128:654–655.3. Kinoshita T, Onoda Y, Maeno T. Long-term surgical outcomes of the inverted internal limiting membrane f lap technique in highly myopic macular hole retinal detachment. Graefes Arch Clin Exp Ophthalmol. 2017; 255:1101–1106.4. Siam AL, El Maamoun TA, Ali MH. Macular buckling for myopic macular hole retinal detachment: a new approach. Retina. 2012; 32:748–753.5. Ripandelli G, Coppe AM, Fedeli R, et al. Evaluation of primary surgical procedures for retinal detachment with macular hole in highly myopic eyes: a comparison of vitrectomy versus poster ior episcleral buckling surgery. Ophthalmology. 2001; 108:2258–2264.6. Wolfensberger TJ, Gonvers M. Long-term follow-up of retinal detachment due to macular hole in myopic eyes treated by temporary silicone oil tamponade and laser photocoagulation. Ophthalmology. 1999; 106:1786–1791.7. Nishimura A, Kimura M, Saito Y, Sugiyama K. Efficacy of primary silicone oil tamponade for the treatment of retinal detachment caused by macular hole in high myopia. Am J Ophthalmol. 2011; 151:148–155.8. Jeon HS, Byon IS, Park SW, et al. Extramacular drainage of subretinal fluid during vitrectomy for macular hole retinal detachment in high myopia. Retina. 2014; 34:1096–1102.9. Kadonosono K, Yazama F, Itoh N, et al. Treatment of retinal detachment resulting from myopic macular hole with internal limiting membrane removal. Am J Ophthalmol. 2001; 131:203–207.10. Park DW, Sipperley JO, Sneed SR, et al. Macular hole surgery with internal-limiting membrane peeling and intravitreous air. Ophthalmology. 1999; 106:1392–1397.11. Uemoto R, Yamamoto S, Tsukahara I, Takeuchi S. Efficacy of internal limiting membrane removal for retinal detachments resulting from a myopic macular hole. Retina. 2004; 24:560–566.12. Michalewska Z, Michalewski J, Adelman RA, Nawrocki J. Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology. 2010; 117:2018–2025.13. Sasaki H, Shiono A, Kogo J, et al. Inverted internal limiting membrane flap technique as a useful procedure for macular hole-associated retinal detachment in highly myopic eyes. Eye (Lond). 2017; 31:545–550.14. Baba R, Wakabayashi Y, Umazume K, et al. Efficacy of the inverted internal limiting membrane flap technique with vitrectomy for retinal detachment associated with myopic macular holes. Retina. 2017; 37:466–471.15. Gonvers M, Machemer R. A new approach to treating retinal detachment with macular hole. Am J Ophthalmol. 1982; 94:468–472.16. Seike C, Kusaka S, Sakagami K, Ohashi Y. Reopening of macular holes in highly myopic eyes with retinal detachments. Retina. 1997; 17:2–6.17. Oshima Y, Ikuno Y, Motokura M, et al. Complete epiretinal membrane separation in highly myopic eyes with retinal detachment resulting from a macular hole. Am J Ophthalmol. 1998; 126:669–676.18. Nakanishi H, Kuriyama S, Saito I, et al. Prognostic factor analysis in pars plana vitrectomy for retinal detachment attributable to macular hole in high myopia: a multicenter study. Am J Ophthalmol. 2008; 146:198–204.19. Nadal J, Verdaguer P, Canut MI. Treatment of retinal detachment secondary to macular hole in high myopia: vitrectomy with dissection of the inner limiting membrane to the edge of the staphyloma and long-term tamponade. Retina. 2012; 32:1525–1530.20. Ikuno Y, Sayanagi K, Oshima T, et al. Optical coherence tomographic findings of macular holes and retinal detachment after vitrectomy in highly myopic eyes. Am J Ophthalmol. 2003; 136:477–481.21. Lam RF, Lai WW, Cheung BT, et al. Pars plana vitrectomy and perfluoropropane (C3F8) tamponade for retinal detachment due to myopic macular hole: a prognostic factor analysis. Am J Ophthalmol. 2006; 142:938–944.22. Cheung CM, Arnold JJ, Holz FG, et al. Myopic choroidal neovascularization: review, guidance, and consensus statement on management. Ophthalmology. 2017; 124:1690–1711.23. Park SW, Pak KY, Park KH, et al. Perfluoro-n-octane assisted free internal limiting membrane flap technique for recurrent macular hole. Retina. 2015; 35:2652–2656.24. Chen SN, Yang CM. Lens capsular flap transplantation in the management of refractory macular hole from multiple etiologies. Retina. 2016; 36:163–170.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous reattachment of retinal detachment with macular hole in nonmyopic patients
- Three Cases of Macular Buckling for Retinal Detachment due to Macular Hole in Highly Myopic Eyes
- Silicone Oil with Short-Term Prone Position in Macular Hole Retinal Detachment Surgery in High Myopia
- Treatment of Macular Hole Retinal Detachment
- Effect of Internal Limiting Membrane Removal in Treatment of Retinal Detachment Caused by Myopic Macular Hole