J Korean Ophthalmol Soc.
2015 Oct;56(10):1566-1571. 10.3341/jkos.2015.56.10.1566.
Silicone Oil with Short-Term Prone Position in Macular Hole Retinal Detachment Surgery in High Myopia
- Affiliations
-
- 1Department of Ophthalmology, Yeungnam University College of Medicine, Daegu, Korea. changwh@ynu.ac.kr
- KMID: 2214416
- DOI: http://doi.org/10.3341/jkos.2015.56.10.1566
Abstract
- PURPOSE
To evaluate the result of vitrectomy with internal limiting membrane peeling and silicone oil tamponade with short term face-down positioning in highly myopic patients with retinal detachment due to macular hole.
METHODS
Eleven eyes of highly myopic patients with retinal detachment caused by macular hole were retrospectively reviewed. All patients underwent pars plana vitrectomy, internal limiting membrane peeling, and silicone oil tamponade with short term (1-3 days) face-down positioning. Silicone oil was removed between 6 and 12 months postoperatively. Outcomes included best-corrected visual acuity, retinal reattachment rate, macular hole closure, and complications.
RESULTS
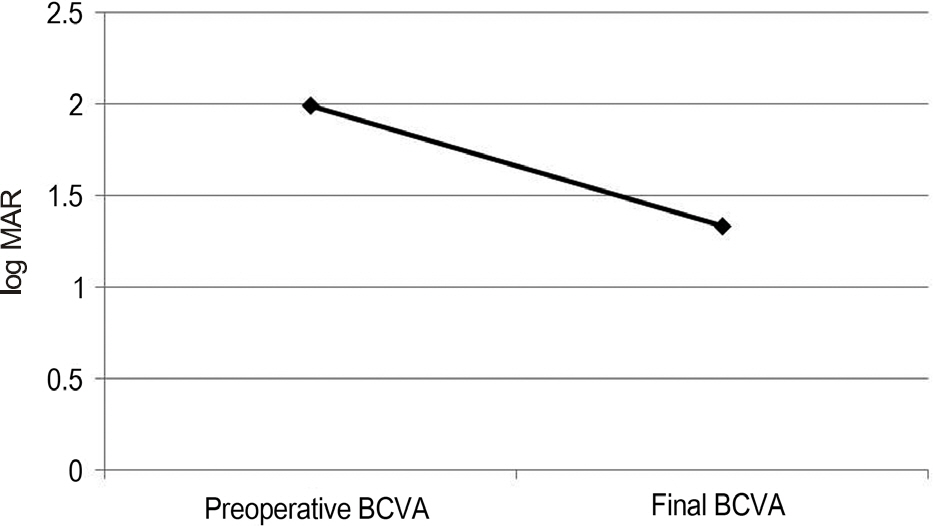
The mean age of patients was 63.3 +/- 8.3 years. During the silicone oil period, all 11 eyes (100%) had complete retinal attachment. After silicone oil removal, retinal detachment recurred in 2 eyes (18.2%). Macular hole closure was observed in 8 eyes (72.7%). The best corrected visual acuity (log MAR) improved from 1.99 +/- 0.94 before surgery to 1.33 +/- 0.62 at final visit.
CONCLUSIONS
Pars plana vitrectomy, internal limiting membrane peeling and silicone oil tamponade with short term face-down positioning was effective in treating retinal detachment caused by macular hole in highly myopic eyes.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Li X, Wang W, Tang S, Zhao J. Gas injection versus vitrectomy with gas for treating retinal detachment owing to macular hole in high myopes. Ophthalmology. 2009; 116:1182–7.e1.
Article2. Cheung BT, Lai TY, Yuen CY. . Results of high-density sili-cone oil as a tamponade agent in macular hole retinal detachment in patients with high myopia. Br J Ophthalmol. 2007; 91:719–21.
Article3. Kadonosono K, Yazama F, Itoh N. . Treatment of retinal de-tachment resulting from myopic macular hole with internal limit-ing membrane removal. Am J Ophthalmol. 2001; 131:203–7.
Article4. Oshima Y, Ikuno Y, Motokura M. . Complete epiretinal mem-brane separation in highly myopic eyes with retinal detachment re-sulting from a macular hole. Am J Ophthalmol. 1998; 126:669–76.5. Gonvers M, Machemer R. A new approach to treating retinal de-tachment with macular hole. Am J Ophthalmol. 1982; 94:468–72.
Article6. Mitamura Y, Takeuchi S, Tsuruoka M. Macular buckling combined with pars plana vitrectomy for complicated retinal detachment due to macular hole. Retina. 2000; 20:669–72.
Article7. Ripandelli G, Parisi V, Friberg TR. . Retinal detachment asso-ciated with macular hole in high myopia: using the vitreous anat-omy to optimize the surgical approach. Ophthalmology. 2004; 111:726–31.8. Ichibe M, Yoshizawa T, Murakami K. . Surgical management of retinal detachment associated with myopic macular hole: ana-tomic and functional status of the macula. Am J Ophthalmol. 2003; 136:277–84.
Article9. Uemoto R, Yamamoto S, Tsukahara I, Takeuchi S. Efficacy of in-ternal limiting membrane removal for retinal detachments result-ing from a myopic macular hole. Retina. 2004; 24:560–6.
Article10. Lam RF, Lai WW, Cheung BT. . Pars plana vitrectomy and per-fluoropropane (C3F8) tamponade for retinal detachment due to myopic macular hole: a prognostic factor analysis. Am J Ophthal-mol. 2006; 142:938–44.
Article11. Oie Y, Emi K, Takaoka G, Ikeda T. Effect of indocyanine green staining in peeling of internal limiting membrane for retinal de-tachment resulting from macular hole in myopic eyes. Ophthal-mology. 2007; 114:303–6.
Article12. Park DY, Kim JH, Ha HS, Kang SW. The macular buckling proce-dure for retinal detachment associated with a macular hole in high myopia. J Korean Ophthalmol Soc. 2012; 53:969–76.
Article13. Scholda C, Wirtitsch M, Biowski R, Stur M. Primary silicone oil tamponade without retinopexy in highly myopic eyes with central macular hole detachments. Retina. 2005; 25:141–6.
Article14. Kim IT, Roh YJ. Primary silicone oil tamponade with vitrectomy in macular hole retinal detachment of highly myopic eyes. J Korean Ophthalmol Soc. 2008; 49:1263–8.
Article15. Ishida S, Yamazaki K, Shinoda K. . Macular hole retinal de-tachment in highly myopic eyes: ultrastructure of surgically re-moved epiretinal membrane and clinicopathologic correlation. Retina. 2000; 20:176–83.
Article16. Wolfensberger TG, Gonvers M. Long-term follow-up of retinal de-tachment due to macular hole in myopic eyes treated by temporary silicone oil tamponade and laser photocoagulation. Ophthalmol-ogy. 1999; 106:1786–91.
Article17. Ripandelli G, Coppé AM, Fedeli R. . Evaluation of primary surgical procedures for retinal detachment with macular hole in highly myopic eyes: a comparison [corrected] of vitrectomy versus posterior episcleral buckling surgery. Ophthalmology. 2001; 108:2258–64. discussion 2265.18. Chen YP, Chen TL, Yang KR. . Treatment of retinal detach-ment resulting from posterior staphyloma-associated macular hole in highly myopic eyes. Retina. 2006; 26:25–31.
Article19. Krohn J. Duration of face-down positioning after macular hole sur-gery: a comparison between 1 week and 3 days. Acta Ophthalmol Scand. 2005; 83:289–92.20. Tornambe PE, Poliner LS, Grote K. Macular hole surgery without face-down positioning. A pilot study. Retina. 1997; 17:179–85.21. Holekamp NM, Meredith TA, Landers MB. . Ulnar neuropathy as a complication of macular hole surgery. Arch Ophthalmol. 1999; 117:1607–10.
Article22. Jumper JM, Gallemore RP, McCuen BW. 2nd. Toth CA. Features of macular hole closure in the early postoperative period using optical coherence tomography. Retina. 2000; 20:232–7.
Article23. Karia N, Laidlaw A, West J. . Macular hole surgery using sili-cone oil tamponade. Br J Ophthalmol. 2001; 85:1320–3.
Article24. Demols P, Schrooyen M. Analysis of optical coherence tomog-raphy for macular hole closure after surgery. Bull Soc Belge Ophtalmol. 2003; ((288)):25–9.25. Matsumura N, Ikuno Y, Tano Y. Posterior vitreous detachment and macular hole formation in myopic foveoschisis. Am J Ophthalmol. 2004; 138:1071–3.
Article26. Abdelkader E, Lois N. Internal limiting membrane peeling in vit-reo-retinal surgery. Surv Ophthalmol. 2008; 53:368–96.
Article27. Christensen UC, Krøyer K, Sander B. . Value of internal limit-ing membrane peeling in surgery for idiopathic macular hole stage 2 and 3: a randomised clinical trial. Br J Ophthalmol. 2009; 93:1005–15.
Article28. Nishimura A, Kimura M, Saito Y, Sugiyama K. Efficacy of pri-mary silicone oil tamponade for the treatment of retinal detachment caused by macular hole in high myopia. Am J Ophthalmol. 2011; 151:148–55.
Article29. Honavar SG, Goyal M, Majji AB. . Glaucoma after pars plana vitrectomy and silicone oil injection for complicated retinal detachments. Ophthalmology. 1999; 106:169–76. discussion 177.30. Budenz DL, Taba KE, Feuer WJ. . Surgical management of secondary glaucoma after pars plana vitrectomy and silicone oil in-jection for complex retinal detachment. Ophthalmology. 2001; 108:1628–32.31. Gonvers M, Andenmatten R. Temporary silicone oil tamponade and intraocular pressure: an 11-year retrospective study. Eur J Ophthalmol. 1996; 6:74–80.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Silicone Oil Tamponade with Vitrectomy in Macular Hole Retinal Detachment of Highly Myopic Eyes
- Prognosis of Retinal Detachment Caused by Macular Hole according to the Refractive Power
- The Macular Buckling Procedure for Retinal Detachment Associated with a Macular Hole in High Myopia
- Autologous Retinal Free Flap Transplantation for Recurrent Giant Macular Hole Retinal Detachment in High Myopia
- Spontaneous reattachment of retinal detachment with macular hole in nonmyopic patients