J Korean Soc Radiol.
2019 Nov;80(6):1145-1159. 10.3348/jksr.2019.80.6.1145.
Diagnosis of Spinal Metastasis: Usefulness of Additional Diffusion-Weighted Imaging
- Affiliations
-
- 1Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Korea. joonwoo2@gmail.com
- 2Department of Radiology, Pusan National University College of Medicine, Pusan National University Yangsan Hospital, Yangsan, Korea.
- KMID: 2464913
- DOI: http://doi.org/10.3348/jksr.2019.80.6.1145
Abstract
- PURPOSE
To determine the usefulness of diffusion weighted-MRI (DW-MRI) in the evaluation of spinal metastasis.
MATERIALS AND METHODS
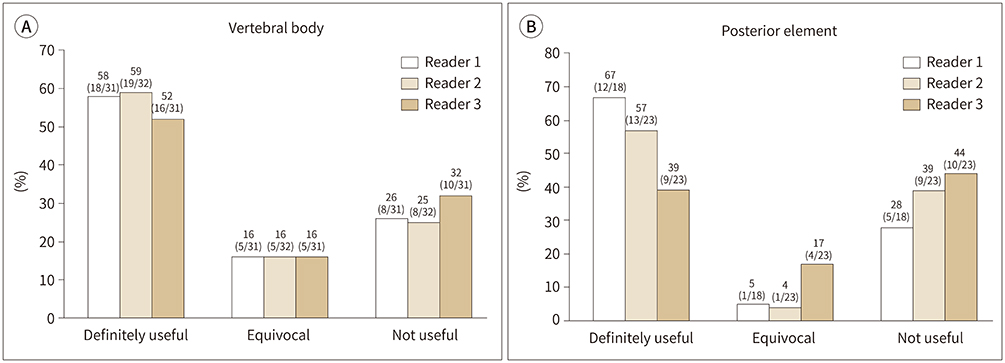
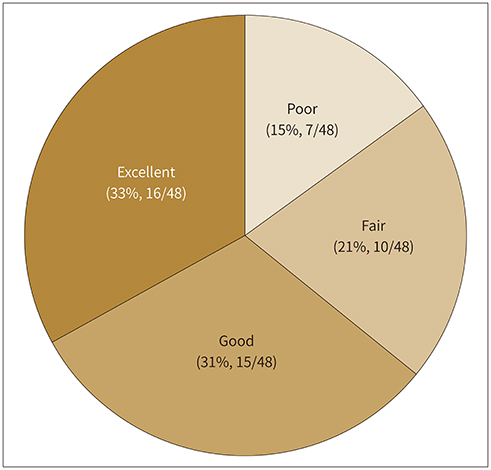
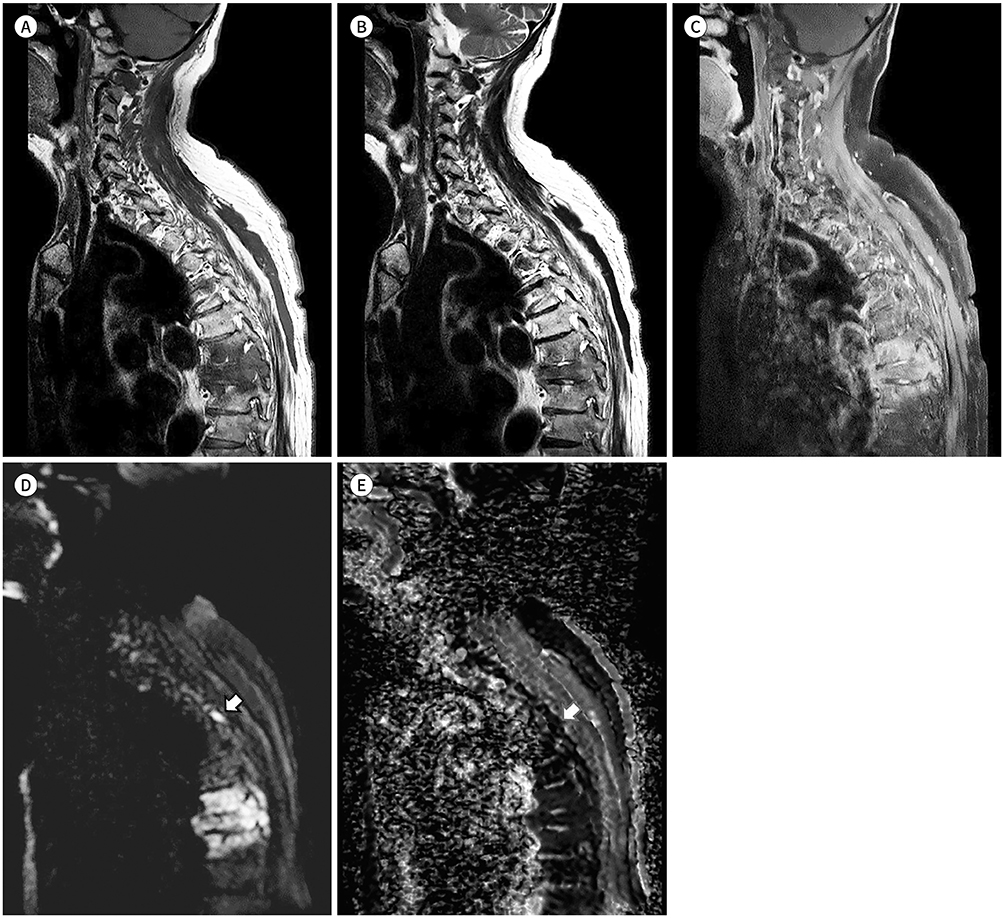
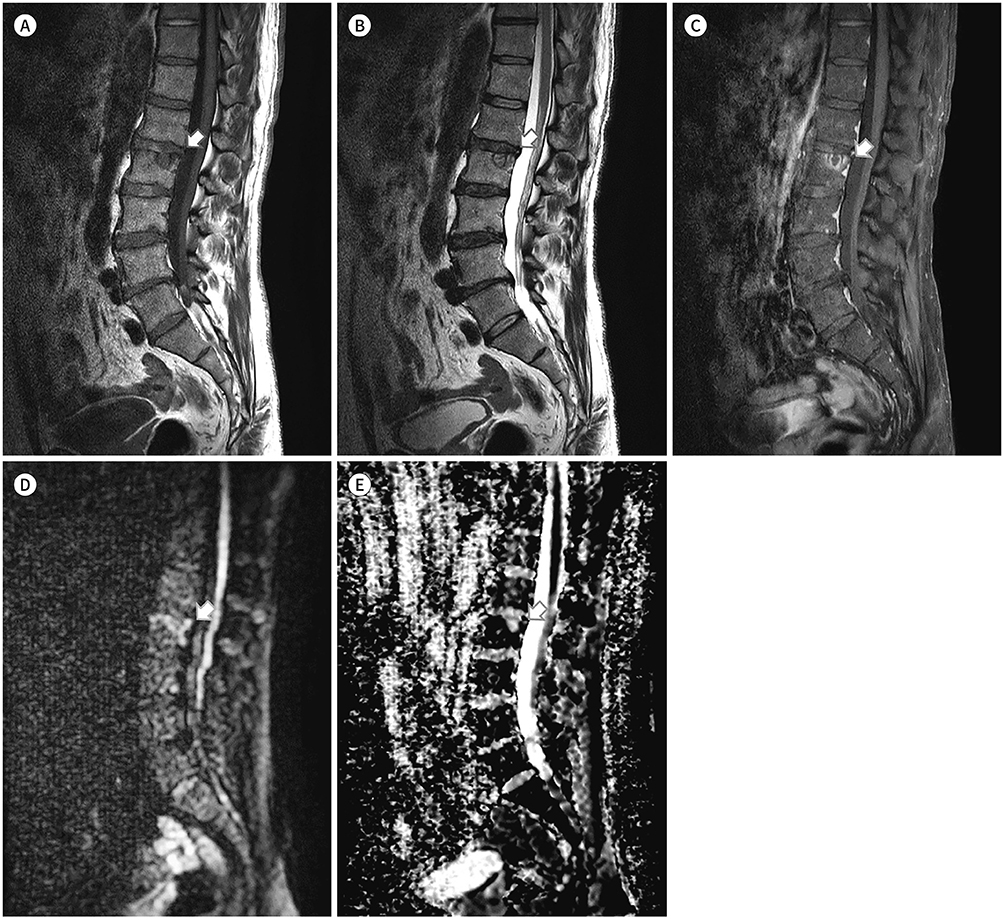
From July to August 2017, 48 whole-spine DW-MRI to detect metastasis in patients with extra-spinal tumors were retrospectively evaluated by three radiologists. The usefulness of DW-MRI was evaluated in four groups based on the change in confidence rating between two sessions: 1 (T1- and T2-weighted and contrast-enhanced images) and 2 (additional DW-MRI). The associations of the usefulness with age, sex, primary cancer, bone type with metastasis, number of probable metastatic segments in session 1, and anatomic locations were assessed in vertebral body and posterior element cases.
RESULTS
According to the readers 1, 2, and 3, there were 18, 19, and 16 vertebral body cases, respectively, and 12, 13, and 9 posterior element cases, respectively. In the group with no excepted metastasis, DW-MRI was useful in 52-59% of vertebral body cases and 39-67% of posterior element cases. There were no significant differences in the usefulness with respect to the number of probable metastatic segments in session 1, age, sex, primary cancer, bone type with metastasis, or anatomic location.
CONCLUSION
DW-MRI could be used to evaluate spinal metastasis. However, there were no differences in the usefulness with respect to the anatomic location.
MeSH Terms
Figure
Reference
-
1. Böhm P, Huber J. The surgical treatment of bony metastases of the spine and limbs. J Bone Joint Surg Br. 2002; 84:521–529.2. Witham TF, Khavkin YA, Gallia GL, Wolinsky JP, Gokaslan ZL. Surgery insight: current management of epidural spinal cord compression from metastatic spine disease. Nat Clin Pract Neurol. 2006; 2:87–94. quiz 116.3. Perrin RG. Metastatic tumors of the axial spine. Curr Opin Oncol. 1992; 4:525–532.4. Keogh C, Bergin D, Brennan D, Eustace S. MR imaging of bone tumors of the cervical spine. Magn Reson Imaging Clin N Am. 2000; 8:513–528.5. Avrahami E, Tadmor R, Dally O, Hadar H. Early MR demonstration of spinal metastases in patients with normal radiographs and CT and radionuclide bone scans. J Comput Assist Tomogr. 1989; 13:598–602.6. Algra PR, Bloem JL, Tissing H, Falke TH, Arndt JW, Verboom LJ. Detection of vertebral metastases: comparison between MR imaging and bone scintigraphy. Radiographics. 1991; 11:219–232.7. Smoker WR, Godersky JC, Knutzon RK, Keyes WD, Norman D, Bergman W. The role of MR imaging in evaluating metastatic spinal disease. AJR Am J Roentgenol. 1987; 149:1241–1248.8. Roberts CC, Daffner RH, Weissman BN, Bancroft L, Bennett DL, Blebea JS, et al. ACR appropriateness criteria on metastatic bone disease. J Am Coll Radiol. 2010; 7:400–409.9. Expert Panel on Radiation Oncology-Bone Metastases. Lo SS, Ryu S, Chang EL, Galanopoulos N, Jones J, et al. ACR Appropriateness Criteria® metastatic epidural spinal cord compression and recurrent spinal metastasis. J Palliat Med. 2015; 18:573–584.10. Patel ND, Broderick DF, Burns J, Deshmukh TK, Fries IB, Harvey HB, et al. ACR appropriateness criteria low back pain. J Am Coll Radiol. 2016; 13:1069–1078.11. Namimoto T, Yamashita Y, Sumi S, Tang Y, Takahashi M. Focal liver masses: characterization with diffusion-weighted echo-planar MR imaging. Radiology. 1997; 204:739–744.12. Woodhams R, Matsunaga K, Iwabuchi K, Kan S, Hata H, Kuranami M, et al. Diffusion-weighted imaging of malignant breast tumors: the usefulness of apparent diffusion coefficient (ADC) value and ADC map for the detection of malignant breast tumors and evaluation of cancer extension. J Comput Assist Tomogr. 2005; 29:644–649.13. Sung JK, Jee WH, Jung JY, Choi M, Lee SY, Kim YH, et al. Differentiation of acute osteoporotic and malignant compression fractures of the spine: use of additive qualitative and quantitative axial diffusion-weighted MR imaging to conventional MR imaging at 3.0 T. Radiology. 2014; 271:488–498.14. Nakanishi K, Kobayashi M, Nakaguchi K, Kyakuno M, Hashimoto N, Onishi H, et al. Whole-body MRI for detecting metastatic bone tumor: diagnostic value of diffusion-weighted images. Magn Reson Med Sci. 2007; 6:147–155.15. Byun WM, Shin SO, Chang Y, Lee SJ, Finsterbusch J, Frahm J. Diffusion-weighted MR imaging of metastatic disease of the spine: assessment of response to therapy. AJNR Am J Neuroradiol. 2002; 23:906–912.16. Daffner RH, Lupetin AR, Dash N, Deeb ZL, Sefczek RJ, Schapiro RL. MRI in the detection of malignant infiltration of bone marrow. AJR Am J Roentgenol. 1986; 146:353–358.17. Carroll KW, Feller JF, Tirman PF. Useful internal standards for distinguishing infiltrative marrow pathology from hematopoietic marrow at MRI. J Magn Reson Imaging. 1997; 7:394–398.18. Chen YC, Sosnoski DM, Mastro AM. Breast cancer metastasis to the bone: mechanisms of bone loss. Breast Cancer Res. 2010; 12:215.19. Shah LM, Salzman KL. Imaging of spinal metastatic disease. Int J Surg Oncol. 2011; 2011:769753.20. An C, Lee YH, Kim S, Cho HW, Suh JS, Song HT. Characteristic MRI findings of spinal metastases from various primary cancers: retrospective study of pathologically-confirmed cases. J Korean Soc Magn Reson Med. 2013; 17:8–18.21. Fisher CG, DiPaola CP, Ryken TC, Bilsky MH, Shaffrey CI, Berven SH, et al. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine (Phila Pa 1976). 2010; 35:E1221–E1229.22. Bilsky MH, Lis E, Raizer J, Lee H, Boland P. The diagnosis and treatment of metastatic spinal tumor. Oncologist. 1999; 4:459–469.23. Georgy BA. Metastatic spinal lesions: state-of-the-art treatment options and future trends. AJNR Am J Neuroradiol. 2008; 29:1605–1611.24. Jacobs WB, Perrin RG. Evaluation and treatment of spinal metastases: an overview. Neurosurg Focus. 2001; 11:e10.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Spinal Cord Infarction: Diffusion-Weighted MR Imaging: Case Report
- Evaluation of Treatment Response Using Diffusion-Weighted MRI in Metastatic Spines
- Diffusion-Weighted Magnetic Resonance Imaging of Spine
- RE: Diffusion-Weighted Imaging of Prostate Cancer: How Can We Use It Accurately?
- Diffusion-Weighted MR Imaging of Spinal Cord Infarction