Allergy Asthma Immunol Res.
2020 Jan;12(1):164-170. 10.4168/aair.2020.12.1.164.
Bronchial Response to High and Low Molecular Weight Occupational Inhalant Allergens
- Affiliations
-
- 1Department of Occupational Diseases and Environmental Health, Nofer Institute of Occupational Medicine, Lodz, Poland. Ewa.Nowakowska-Swirta@imp.lodz.pl
- KMID: 2462580
- DOI: http://doi.org/10.4168/aair.2020.12.1.164
Abstract
- PURPOSE
Occupational asthma may be induced by high- or low-molecular weight allergens (HMWA or LMWA, respectively). The study was conducted to compare the pattern of bronchial response in 200 HMWA-induced asthmatics (n = 130) and LMWA-induced asthmatics (n = 70).
METHODS
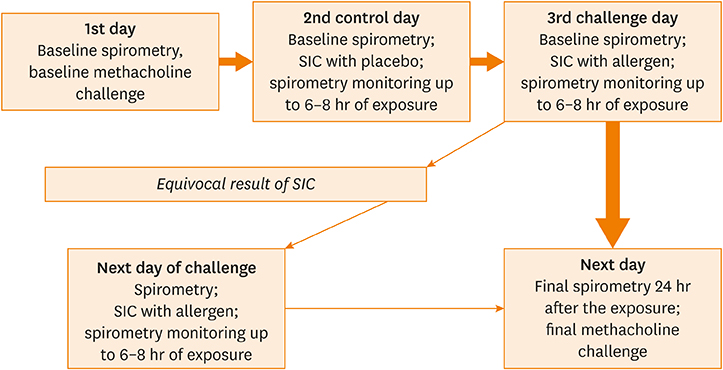
The study participants underwent a single-blind, placebo-controlled specific inhalation challenge (SIC) with workplace allergens, accompanied by evaluation of non-specific bronchial hyperresponsiveness (NSBHR) with methacholine before and after the SIC.
RESULTS
A single early bronchial response more frequently occurred in HMWA-induced asthmatics than in LMWA-induced asthmatics (86.2% vs. 20%). An isolated late bronchial response or atypical patterns were more frequently observed in LMWA-induced asthmatics than in LMWA-induced asthmatics (45.7% vs. 3.8% or 34.3% vs. 10%, respectively). Baseline NSBHR before SIC was more often detected in LMWA-induced asthmatics than in HMWA-induced asthmatics (81.4% vs. 54.6%), and the median value of the provocation concentration of methacholine was relevantly lower in these patients before and after SIC. A significant 3-fold increase in NSBHR after SIC was observed more often in LMWA-induced asthmatics than in HMWA-induced asthmatics (82.8% vs. 66.1%). In addition, compared to LMWA-induced asthmatics, HMWA-induced asthmatics were older, were more frequently active smokers, showed lower level of NSBHR, and more frequently continued their work in harmful occupational exposure.
CONCLUSIONS
The results of this study suggest that HMWA-induced asthmatics may have milder clinical courses and that there is a possibility of job continuation despite asthma exacerbation requiring medical surveillance.
Keyword
MeSH Terms
Figure
Reference
-
1. Johansson SG, Hourihane JO, Bousquet J, Bruijnzeel-Koomen C, Dreborg S, Haahtela T, et al. A revised nomenclature for allergy. An EAACI position statement from the EAACI nomenclature task force. Allergy. 2001; 56:813–824.
Article2. Rabatin JT, Cowl CT. A guide to the diagnosis and treatment of occupational asthma. Mayo Clin Proc. 2001; 76:633–640.
Article3. Tarlo SM, Balmes J, Balkissoon R, Beach J, Beckett W, Bernstein D, et al. Diagnosis and management of work-related asthma: American college of chest physicians consensus statement. Chest. 2008; 134:Suppl. 1S–41S.4. Moscato G, Pala G, Barnig C, De Blay F, Del Giacco SR, Folletti I, et al. EAACI consensus statement for investigation of work-related asthma in non-specialized centres. Allergy. 2012; 67:491–501.
Article5. Bardana EJ Jr. 8. Occupational asthma and allergies. J Allergy Clin Immunol. 2003; 111:S530–S539.
Article6. Kaplan AP. A new mechanism for immunologic initiation of asthma. Proc Natl Acad Sci U S A. 2005; 102:1267–1268.
Article7. Chapman MD. Allergen nomenclature. Clin Allergy Immunol. 2008; 21:47–58.8. Kimber I, Dearman RJ. What makes a chemical a respiratory sensitizer? Curr Opin Allergy Clin Immunol. 2005; 5:119–124.
Article9. Baldo BA, Pham NH, Zhao Z. Chemistry of drug allergenicity. Curr Opin Allergy Clin Immunol. 2001; 1:327–335.
Article10. Larsen ST, Hansen R, Poulsen OM, Nielsen GD. Adjuvant effect of benzalkonium chloride on the allergen-specific IgE, IgG1 and IgG2a antibody formation in BALB/cJ mice. Basic Clin Pharmacol Toxicol. 2004; 95:94–96.
Article11. Kramps JA, van Toorenenbergen AW, Vooren PH, Dijkman JH. Occupational asthma due to inhalation of chloramine-T. II. Demonstration of specific IgE antibodies. Int Arch Allergy Appl Immunol. 1981; 64:428–438.12. Zock JP, Kogevinas M, Sunyer J, Almar E, Muniozguren N, Payo F, et al. Asthma risk, cleaning activities and use of specific cleaning products among Spanish indoor cleaners. Scand J Work Environ Health. 2001; 27:76–81.
Article13. Vandenplas O, Suojalehto H, Aasen TB, Baur X, Burge PS, de Blay F, et al. Specific inhalation challenge in the diagnosis of occupational asthma: consensus statement. Eur Respir J. 2014; 43:1573–1587.
Article14. Vandenplas O, Godet J, Hurdubaea L, Rifflart C, Suojalehto H, Wiszniewska M, et al. Are high- and low-molecular-weight sensitizing agents associated with different clinical phenotypes of occupational asthma? Allergy. 2019; 74:261–272.
Article15. Baur X, Sigsgaard T, Aasen TB, Burge PS, Heederik D, Henneberger P, et al. Guidelines for the management of work-related asthma. Eur Respir J. 2012; 39:529–545.
Article16. Klusáčková P, Pelclová D, Jindriska Levedova D, Mareckova H, Brabec M. Occupational asthma after withdrawal from the occupational allergen exposure. Ind Health. 2006; 44:629–638.
Article17. Chapman DG, Irvin CG. Mechanisms of airway hyper-responsiveness in asthma: the past, present and yet to come. Clin Exp Allergy. 2015; 45:706–719.
Article18. Coates AL, Wanger J, Cockcroft DW, Culver BH. Bronchoprovocation Testing Task Force: Kai-Håkon Carlsen. Diamant Z, et al. ERS technical standard on bronchial challenge testing: general considerations and performance of methacholine challenge tests. Eur Respir J. 2017; 49:1601526.
Article19. Crapo RO, Casaburi R, Coates AL, Enright PL, Hankinson JL, Irvin CG, et al. Guidelines for methacholine and exercise challenge testing-1999. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. Am J Respir Crit Care Med. 2000; 161:309–329.20. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005; 26:319–338.21. Vandenplas O, Suojalehto H, Cullinan P. Diagnosing occupational asthma. Clin Exp Allergy. 2017; 47:6–18.
Article22. Wiszniewska M, Nowakowska-Świrta E, Pałczyński C, Walusiak-Skorupa J. Diagnosing of bakers' respiratory allergy: is specific inhalation challenge test essential? Allergy Asthma Proc. 2011; 32:111–118.
Article23. Tarlo SM, Lemiere C. Occupational asthma. N Engl J Med. 2014; 370:640–649.
Article24. Tan J, Bernstein JA. Occupational asthma: an overview. Curr Allergy Asthma Rep. 2014; 14:431.
Article25. Bernstein IL, Bernstein DI, Chan-Yeung M, Malo JL. Definition and classification of asthma in the workplace. In : Malo JL, Chan-Yeung M, Bernstein DI, editors. Asthma in the workplace. Boca Raton (FL): CRC Press;2013. p. 1–5.26. Malo JL, Vandenplas O. Definitions and classification of work-related asthma. Immunol Allergy Clin North Am. 2011; 31:645–662.
Article27. Dufour MH, Lemière C, Prince P, Boulet LP. Comparative airway response to high- versus low-molecular weight agents in occupational asthma. Eur Respir J. 2009; 33:734–739.
Article28. Talini D, Novelli F, Bacci E, Dente FL, De Santis M, Di Franco A, et al. Comparison between airway responses to high versus low molecular weight compounds in occupational asthma. J Allergy (Cairo). 2011; 2011:781470.
Article29. Meca O, Cruz MJ, Sánchez-Ortiz M, González-Barcala FJ, Ojanguren I, Munoz X. Do low molecular weight agents cause more severe asthma than high molecular weight agents? PLoS One. 2016; 11:e0156141.
Article30. Pralong JA, Lemière C, Rochat T, L'Archevêque J, Labrecque M, Cartier A. Predictive value of nonspecific bronchial responsiveness in occupational asthma. J Allergy Clin Immunol. 2016; 137:412–416.
Article31. Lemiere C, NGuyen S, Sava F, D'Alpaos V, Huaux F, Vandenplas O. Occupational asthma phenotypes identified by increased fractional exhaled nitric oxide after exposure to causal agents. J Allergy Clin Immunol. 2014; 134:1063–1067.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Newly sensitization to house dust mite in an isocyanate-induced asthmatic patient
- A comparison of Sensitization to Major Indoor & Outdoor Inhalant Allergens in Children with Respiratory Allergic Diseases
- A case of Tetranychus urticae - induced asthma in an inhabitant around pear orchard
- Early Exposure to Inhalant Allergens and Sensitization
- Changing patterns of skin reactivity to inhalant allergens in asthmatic patients