Clin Orthop Surg.
2019 Sep;11(3):344-351. 10.4055/cios.2019.11.3.344.
Secondary Cervicothoracic Scoliosis in Congenital Muscular Torticollis
- Affiliations
-
- 1Department of Orthopedic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jss3505@skku.edu
- KMID: 2462565
- DOI: http://doi.org/10.4055/cios.2019.11.3.344
Abstract
- BACKGROUND
Although secondary cervicothoracic scoliosis frequently occurs in patients with congenital muscular torticollis (CMT), the relationship between scoliosis and CMT has not been evaluated. This study aims to evaluate the effects of surgical release of sternocleidomastoid (SCM) muscle on secondary cervicothoracic scoliosis in patients with CMT and determine factors affecting the improvement of scoliosis after surgical release of SCM muscle.
METHODS
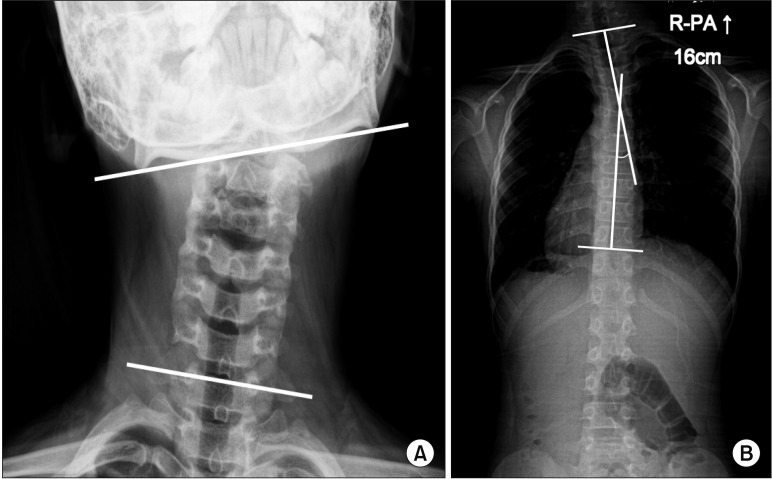
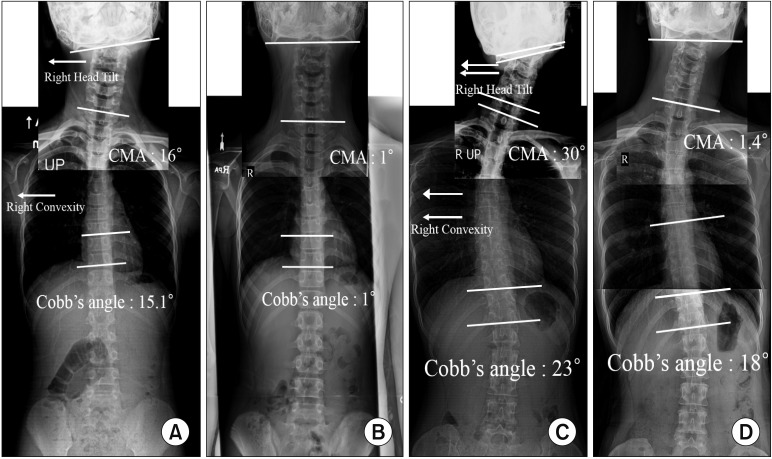
Eighty-seven of the 106 patients, confirmed as having secondary cervicothoracic scoliosis with CMT with a minimum 1-year follow-up, were included in this study. Preoperative and last follow-up radiologic outcomes were assessed for the cervicomandibular angle (CMA), Cobb angle of the cervicothoracic scoliosis, and direction of convexity in the scoliosis curve. Patients were divided into two groups to assess the improvement of Cobb angle according to residual growth potential; age ≤ 15 years and > 15 years. The improvement of Cobb angle after surgical release was compared in the two groups. Correlation analysis and multivariable regression analysis were performed to determine the factors affecting the improvement of scoliosis.
RESULTS
All the radiologic parameters, such as the Cobb angle and CMA, improved significantly after surgical release (p < 0.001). The improvement of Cobb angle was significantly higher in age ≤ 15 years than in age > 15 years (p < 0.001). The improvement of Cobb angle was significantly correlated with age (r = −0.474, p < 0.001) and the preoperative Cobb angle (r = 0.221, p = 0.036). In multivariable regression analysis, age and preoperative Cobb angle were shown to be predisposing factors affecting the improvement of scoliosis.
CONCLUSIONS
The results showed that SCM release can be a beneficial treatment for secondary cervicothoracic scoliosis. The improvement of scoliosis was greater when the SCM release was performed before the patient reached the end of growth.
Keyword
Figure
Reference
-
1. Ta JH, Krishnan M. Management of congenital muscular torticollis in a child: a case report and review. Int J Pediatr Otorhinolaryngol. 2012; 76(11):1543–1546. PMID: 22889576.
Article2. Hussein MA, Yun IS, Park H, Kim YO. Cervical spine deformity in long-standing, untreated congenital muscular torticollis. J Craniofac Surg. 2017; 28(1):46–50. PMID: 27922967.
Article3. Lee JK, Moon HJ, Park MS, Yoo WJ, Choi IH, Cho TJ. Change of craniofacial deformity after sternocleidomastoid muscle release in pediatric patients with congenital muscular torticollis. J Bone Joint Surg Am. 2012; 94(13):e93. PMID: 22760394.
Article4. Seo SJ, Kim JH, Joh YH, et al. Change of facial asymmetry in patients with congenital muscular torticollis after surgical release. J Craniofac Surg. 2016; 27(1):64–69. PMID: 26745190.
Article5. Seo SJ, Yim SY, Lee IJ, et al. Is craniofacial asymmetry progressive in untreated congenital muscular torticollis? Plast Reconstr Surg. 2013; 132(2):407–413. PMID: 23584628.
Article6. Lim KS, Shim JS, Lee YS. Is sternocleidomastoid muscle release effective in adults with neglected congenital muscular torticollis? Clin Orthop Relat Res. 2014; 472(4):1271–1278. PMID: 24258687.
Article7. Canale ST, Griffin DW, Hubbard CN. Congenital muscular torticollis: a long-term follow-up. J Bone Joint Surg Am. 1982; 64(6):810–816. PMID: 7085709.
Article8. Omidi-Kashani F, Hasankhani EG, Sharifi R, Mazlumi M. Is surgery recommended in adults with neglected congenital muscular torticollis? A prospective study. BMC Musculoskelet Disord. 2008; 9:158. PMID: 19036153.
Article9. Mogaadi M, Ben Omrane L, Hammou A. Effective dose for scoliosis patients undergoing full spine radiography. Radiat Prot Dosimetry. 2012; 149(3):297–303. PMID: 21737443.
Article10. Newton PO, Khandwala Y, Bartley CE, Reighard FG, Bastrom TP, Yaszay B. New EOS imaging protocol allows a substantial reduction in radiation exposure for scoliosis patients. Spine Deform. 2016; 4(2):138–144. PMID: 27927546.
Article11. Danielsson AJ, Nachemson AL. Back pain and function 22 years after brace treatment for adolescent idiopathic scoliosis: a case-control study-part I. Spine (Phila Pa 1976). 2003; 28(18):2078–2085. PMID: 14501917.12. Patwardhan S, Shyam AK, Sancheti P, Arora P, Nagda T, Naik P. Adult presentation of congenital muscular torticollis: a series of 12 patients treated with a bipolar release of sternocleidomastoid and Z-lengthening. J Bone Joint Surg Br. 2011; 93(6):828–832. PMID: 21586785.13. Goldstein LA, Waugh TR. Classification and terminology of scoliosis. Clin Orthop Relat Res. 1973; (93):10–22. PMID: 4722939.
Article14. Keynan O, Fisher CG, Vaccaro A, et al. Radiographic measurement parameters in thoracolumbar fractures: a systematic review and consensus statement of the spine trauma study group. Spine (Phila Pa 1976). 2006; 31(5):E156–E165. PMID: 16508540.
Article15. Shim JS, Jang HP. Operative treatment of congenital torticollis. J Bone Joint Surg Br. 2008; 90(7):934–939. PMID: 18591606.
Article16. Cobb JR. Outline for the study of scoliosis. Am Acad Orthop Surg Instr Course Lect. 1948; 5:261–275.17. Cheng JC, Tang SP. Outcome of surgical treatment of congenital muscular torticollis. Clin Orthop Relat Res. 1999; (362):190–200.
Article18. Jones KB, Sponseller PD, Hobbs W, Pyeritz RE. Leg-length discrepancy and scoliosis in Marfan syndrome. J Pediatr Orthop. 2002; 22(6):807–812. PMID: 12409912.
Article19. Papaioannou T, Stokes I, Kenwright J. Scoliosis associated with limb-length inequality. J Bone Joint Surg Am. 1982; 64(1):59–62. PMID: 7054204.
Article20. Walker AP, Dickson RA. School screening and pelvic tilt scoliosis. Lancet. 1984; 2(8395):152–153. PMID: 6146046.
Article21. Danielsson AJ, Nachemson AL. Back pain and function 23 years after fusion for adolescent idiopathic scoliosis: a case-control study-part II. Spine (Phila Pa 1976). 2003; 28(18):E373–E383. PMID: 14501939.
Article22. Mesfin A, Bakhsh WR, Chuntarapas T, Riew KD. Cervical scoliosis: clinical and radiographic outcomes. Global Spine J. 2016; 6(1):7–13. PMID: 26835196.
Article23. Fowles JV, Drummond DS, L'Ecuyer S, Roy L, Kassab MT. Untreated scoliosis in the adult. Clin Orthop Relat Res. 1978; (134):212–217.
Article24. Nachemson A. A long term follow-up study of non-treated scoliosis. Acta Orthop Scand. 1968; 39(4):466–476. PMID: 5726117.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Familial Congenital Muscular Torticollis: A Case Report
- Two Cases of Sternomastoid Tumor
- Congenital Torticollis with Bilateral Sternocleidomastoid Muscle Contracture
- Biterminal Sternocleidomastoid Tenotomy for the Treatment of Congenital Muscular Torticollis in Children
- Unipolar Release of the Sternocleidomastoideus in Congenital Muscular Torticollis in Children