Clin Orthop Surg.
2019 Dec;11(4):409-415. 10.4055/cios.2019.11.4.409.
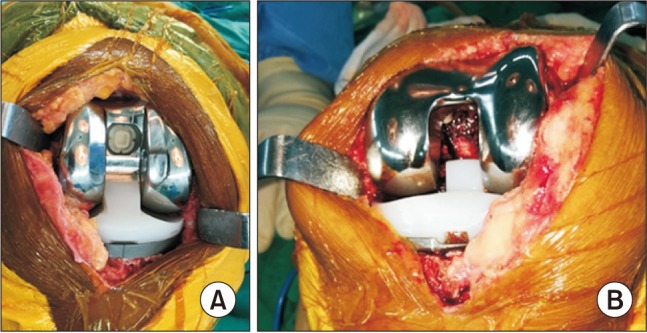
The Effect of Prosthesis Design on Blood Loss in Simultaneous Bilateral Total Knee Arthroplasty: Closed-Box versus Open-Box Prosthesis
- Affiliations
-
- 1Department of Orthopedics, Faculty of Medicine, Naresuan University, Phitsanulok, Thailand. pt-rp@hotmail.com
- 2Department of Preventive and Social Medicine, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand.
- KMID: 2462534
- DOI: http://doi.org/10.4055/cios.2019.11.4.409
Abstract
- BACKGROUND
Various pre- and perioperative risk factors have been reported in association with blood loss in knee arthroplasty. However, the effect of the uncovered cancellous surface on blood loss in simultaneous bilateral total knee arthroplasty (SBTKA) by different prosthetic designs is not well elucidated. Therefore, this study aimed to compare the blood loss and transfusion rate between different knee prostheses in SBTKA and to identify risk factors that influence blood loss and transfusion after SBTKA.
METHODS
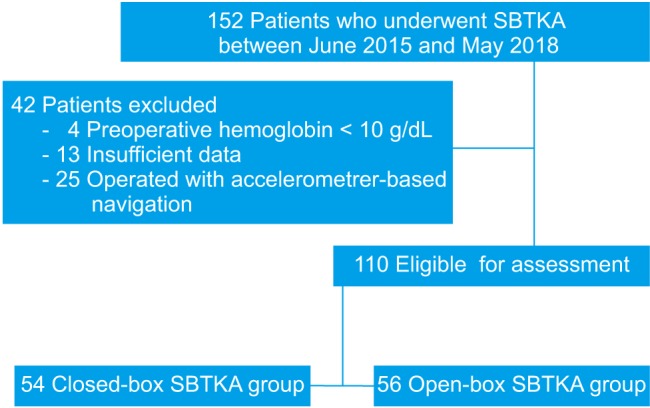
Demographic and perioperative data of patients who underwent SBTKA using either a closed-box or an open-box femoral component of posterior-stabilized fixed-bearing (PS FB) knee system were retrospectively reviewed. The calculated blood loss (CBL) and blood transfusion rate were compared by using Student t-test and confirmed with multivariate regression analysis.
RESULTS
There was no significant difference in preoperative parameters between 54 closed-box and 56 open-box PS FB TKAs. The CBL of the closed-box TKA group was 135.23 mL less (95% confidence interval [CI], −215.30 to −55.16; p = 0.001) than that of the open-box TKA group. However, the blood transfusion rates of the closed- and open-box TKA groups were not significantly different (24.1% and 38.5%, p = 0.11). For each additional minute of total operative time, 3.75 mL (95% CI, 1.75 to 5.76; p < 0.001) of blood loss was anticipated. For each additional mg/dL of preoperative hemoglobin, 71% (p < 0.001) reduction of blood transfusion probability was predicted.
CONCLUSIONS
The use of closed- and open-box knee prostheses resulted in a significant difference in blood loss in SBTKA. Prolonged operative time also significantly increased CBL. Therefore, strategies to control the bleeding surface and shorten operative duration may be considered if blood loss is of special concern. The preoperative hemoglobin was the only factor that affects the probability of blood transfusion in SBTKA.
Keyword
MeSH Terms
Figure
Reference
-
1. Walmsley P, Murray A, Brenkel IJ. The practice of bilateral, simultaneous total knee replacement in Scotland over the last decade: data from the Scottish Arthroplasty Project. Knee. 2006; 13(2):102–105. PMID: 16481171.
Article2. Kulshrestha V, Kumar S, Datta B, Sinha VK, Mittal G. Ninety-day morbidity and mortality in risk-screened and optimized patients undergoing two-team fast-track simultaneous bilateral TKA compared with unilateral TKA-A prospective study. J Arthroplasty. 2018; 33(3):752–760. PMID: 29102512.
Article3. Fu D, Li G, Chen K, Zeng H, Zhang X, Cai Z. Comparison of clinical outcome between simultaneous-bilateral and staged-bilateral total knee arthroplasty: a systematic review of retrospective studies. J Arthroplasty. 2013; 28(7):1141–1147. PMID: 23518424.
Article4. Mylod AG Jr, France MP, Muser DE, Parsons JR. Perioperative blood loss associated with total knee arthroplasty: a comparison of procedures performed with and without cementing. J Bone Joint Surg Am. 1990; 72(7):1010–1012. PMID: 2384499.
Article5. Raut VV, Stone MH, Wroblewski BM. Reduction of postoperative blood loss after press-fit condylar knee arthroplasty with use of a femoral intramedullary plug. J Bone Joint Surg Am. 1993; 75(9):1356–1357. PMID: 8408156.
Article6. Levy O, Martinowitz U, Oran A, Tauber C, Horoszowski H. The use of fibrin tissue adhesive to reduce blood loss and the need for blood transfusion after total knee arthroplasty: a prospective, randomized, multicenter study. J Bone Joint Surg Am. 1999; 81(11):1580–1588. PMID: 10565650.
Article7. Mahringer-Kunz A, Efe T, Fuchs-Winkelmann S, Schuttler KF, Paletta JR, Heyse TJ. Bleeding in TKA: posterior stabilized vs. cruciate retaining. Arch Orthop Trauma Surg. 2015; 135(6):867–870. PMID: 25917192.
Article8. Slover J, Lavery JA, Schwarzkopf R, Iorio R, Bosco J, Gold HT. Incidence and risk factors for blood transfusion in total joint arthroplasty: analysis of a statewide database. J Arthroplasty. 2017; 32(9):2684–2687. PMID: 28579446.
Article9. Jenny JY, Trojani C, Prudhon JL, et al. Simultaneous bilateral total knee arthroplasty: a multicenter feasibility study. Orthop Traumatol Surg Res. 2013; 99(2):191–195. PMID: 23465514.
Article10. Friedman R, Homering M, Holberg G, Berkowitz SD. Allogeneic blood transfusions and postoperative infections after total hip or knee arthroplasty. J Bone Joint Surg Am. 2014; 96(4):272–278. PMID: 24553882.
Article11. Silliman CC, Fung YL, Ball JB, Khan SY. Transfusion-related acute lung injury (TRALI): current concepts and misconceptions. Blood Rev. 2009; 23(6):245–255. PMID: 19699017.
Article12. Yoshihara H, Yoneoka D. Predictors of allogeneic blood transfusion in total hip and knee arthroplasty in the United States, 2000-2009. J Arthroplasty. 2014; 29(9):1736–1740. PMID: 24891002.
Article13. Frisch NB, Wessell NM, Charters MA, Yu S, Jeffries JJ, Silverton CD. Predictors and complications of blood transfusion in total hip and knee arthroplasty. J Arthroplasty. 2014; 29(9 Suppl):189–192. PMID: 25007727.
Article14. Cankaya D, Ozkurt B, Aydin C, Tabak AY. No difference in blood loss between posterior-cruciate-ligament-retaining and posterior-cruciate-ligament-stabilized total knee arthroplasties. Knee Surg Sports Traumatol Arthrosc. 2014; 22(8):1865–1869. PMID: 24384945.
Article15. Nadler SB, Hidalgo JH, Bloch T. Prediction of blood volume in normal human adults. Surgery. 1962; 51(2):224–232. PMID: 21936146.16. Chen JY, Chin PL, Moo IH, et al. Intravenous versus intraarticular tranexamic acid in total knee arthroplasty: a double-blinded randomised controlled noninferiority trial. Knee. 2016; 23(1):152–156. PMID: 26746044.
Article17. Qi Y, Tie K, Wang H, et al. Perioperative comparison of blood loss and complications between simultaneous bilateral and unilateral total knee arthroplasty for knee osteoarthritis. Knee. 2017; 24(6):1422–1427. PMID: 28974399.
Article18. Kalairajah Y, Simpson D, Cossey AJ, Verrall GM, Spriggins AJ. Blood loss after total knee replacement: effects of computer-assisted surgery. J Bone Joint Surg Br. 2005; 87(11):1480–1482. PMID: 16260662.19. Torres-Claramunt R, Hinarejos P, Perez-Prieto D, et al. Sealing of the intramedullar femoral canal in a TKA does not reduce postoperative blood loss: a randomized prospective study. Knee. 2014; 21(4):853–857. PMID: 24842494.
Article20. Moo IH, Chen JY, Pagkaliwaga EH, Tan SW, Poon KB. Bone wax is effective in reducing blood loss after total knee arthroplasty. J Arthroplasty. 2017; 32(5):1483–1487. PMID: 28089184.
Article21. Aggarwal AK, Shashikanth VS, Marwaha N. Platelet-rich plasma prevents blood loss and pain and enhances early functional outcome after total knee arthroplasty: a prospective randomised controlled study. Int Orthop. 2014; 38(2):387–395. PMID: 24114251.
Article22. Gardner MJ, Demetrakopoulos D, Klepchick PR, Mooar PA. The efficacy of autologous platelet gel in pain control and blood loss in total knee arthroplasty: an analysis of the haemoglobin, narcotic requirement and range of motion. Int Orthop. 2007; 31(3):309–313. PMID: 16816947.23. Cushner FD, Friedman RJ. Blood loss in total knee arthroplasty. Clin Orthop Relat Res. 1991; (269):98–101.
Article24. Prasad N, Padmanabhan V, Mullaji A. Blood loss in total knee arthroplasty: an analysis of risk factors. Int Orthop. 2007; 31(1):39–44. PMID: 16568327.
Article25. Noticewala MS, Nyce JD, Wang W, Geller JA, Macaulay W. Predicting need for allogeneic transfusion after total knee arthroplasty. J Arthroplasty. 2012; 27(6):961–967. PMID: 22608172.
Article26. Chen X, Cao X, Yang C, Guo K, Zhu Q, Zhu J. Effectiveness and safety of fixed-dose tranexamic acid in simultaneous bilateral total knee arthroplasty: a randomized double-blind controlled trial. J Arthroplasty. 2016; 31(11):2471–2475. PMID: 27167769.
Article27. Bagsby DT, Samujh CA, Vissing JL, Empson JA, Pomeroy DL, Malkani AL. Tranexamic acid decreases incidence of blood transfusion in simultaneous bilateral total knee arthroplasty. J Arthroplasty. 2015; 30(12):2106–2109. PMID: 26235522.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cement Mantle Thickness at the Bone Cement Interface in Total Knee Arthroplasty: Comparison of PS150 RP and LPS-Flex Knee Implants
- Effect of Closed Suction Drain on Blood Loss and Transfusion Rates in Simultaneous Bilateral Total Knee Arthroplasty: A Prospective Randomized Study
- The Effect of Intraoperative Tourniquet Deflation in Total Knee Arthroplasty
- Diagnosis, Causes and Treatments of Instability Following Total Knee Arthroplasty
- Anthropometric Study of Distal Femur & Compatibility of Gender Knee Prosthesis in Total Knee Replacement