Obstet Gynecol Sci.
2019 Nov;62(6):411-419. 10.5468/ogs.2019.62.6.411.
Prevalence and oncologic outcomes of BRCA1/2 mutation and variant of unknown significance in epithelial ovarian carcinoma patients in Korea
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. chelhun.choi@samsung.com
- KMID: 2462119
- DOI: http://doi.org/10.5468/ogs.2019.62.6.411
Abstract
OBJECTIVE
BRCA mutational status is important in the management of ovarian cancer, but there is a lack of evidence supporting genetic testing in Asian populations. This study was performed to investigate the prevalence and prognostic outcomes of BRCA1/2 mutation and variant of unknown significance (VUS) in Korean patients diagnosed with epithelial ovarian cancer (EOC).
METHODS
Among patients newly diagnosed with EOC between January 2007 and January 2017, those tested for germline BRCA1/2 mutation were studied, regardless of family history. Overall survival (OS) and progression-free survival (PFS) were compared between the patients with and without BRCA1/2 mutation and VUS.
RESULTS
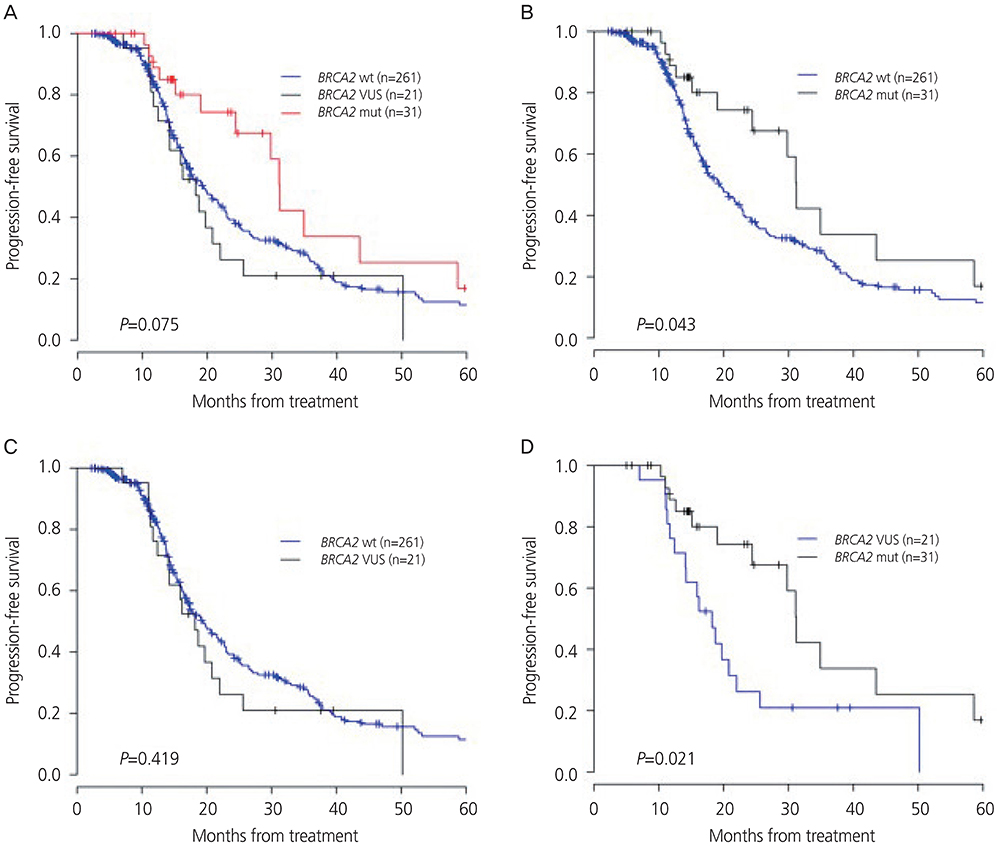
A total of 313 patients underwent BRCA testing: 88 patients had a BRCA1/2 mutation and 48 patients had a BRCA1/2 VUS (28.1% and 15.3%, respectively). There were no significant associations between BRCA1/2 mutation, BRCA1/2 wild-type, or BRCA1/2 VUS with age at diagnosis, histologic distribution, or residual disease status after primary cytoreductive surgery. BRCA1 mutation, including BRCA1 VUS, showed no difference in PFS or OS compared to BRCA1 wild-type. In contrast, BRCA2 mutation showed longer PFS than that of BRCA2 wild-type (P=0.04) or BRCA2 VUS (P=0.02). BRCA2 mutation, including BRCA2 VUS, did not show any difference in OS compared to BRCA2 wild-type.
CONCLUSION
BRCA mutation and BRCA VUS had similar clinical characteristics and survival outcomes, except that BRCA2 mutation showed better PFS. The results of this study will help to understand the prognostic significance of BRCA mutation and VUS in Korean patients.
MeSH Terms
Figure
Reference
-
1. Banerjee S, Kaye SB. New strategies in the treatment of ovarian cancer: current clinical perspectives and future potential. Clin Cancer Res. 2013; 19:961–968.
Article2. George SH, Shaw P. BRCA and early events in the development of serous ovarian cancer. Front Oncol. 2014; 4:5.3. Hyman DM, Zhou Q, Iasonos A, Grisham RN, Arnold AG, Phillips MF, et al. Improved survival for BRCA2-associated serous ovarian cancer compared with both BRCA-negative and BRCA1-associated serous ovarian cancer. Cancer. 2012; 118:3703–3709.4. Yang D, Khan S, Sun Y, Hess K, Shmulevich I, Sood AK, et al. Association of BRCA1 and BRCA2 mutations with survival, chemotherapy sensitivity, and gene mutator phenotype in patients with ovarian cancer. JAMA. 2011; 306:1557–1565.5. Lim MC, Kang S, Seo SS, Kong SY, Lee BY, Lee SK, et al. BRCA1 and BRCA2 germline mutations in Korean ovarian cancer patients. J Cancer Res Clin Oncol. 2009; 135:1593–1599.6. Kim YT, Nam EJ, Yoon BS, Kim SW, Kim SH, Kim JH, et al. Germline mutations of BRCA1 and BRCA2 in Korean sporadic ovarian carcinoma. Gynecol Oncol. 2005; 99:585–590.7. Eoh KJ, Park HS, Park JS, Lee ST, Han J, Lee JY, et al. Comparison of clinical outcomes of BRCA1/2 pathologic mutation, variants of unknown significance, or wild type epithelial ovarian cancer patients. Cancer Res Treat. 2017; 49:408–415.8. Kim SI, Lee M, Kim HS, Chung HH, Kim JW, Park NH, et al. Effect of BRCA mutational status on survival outcome in advanced-stage high-grade serous ovarian cancer. J Ovarian Res. 2019; 12:40.
Article9. Calò V, Bruno L, La Paglia L, Perez M, Margarese N, Di Gaudio F, et al. The clinical significance of unknown sequence variants in BRCA genes. Cancers (Basel). 2010; 2:1644–1660.10. Aida H, Takakuwa K, Nagata H, Tsuneki I, Takano M, Tsuji S, et al. Clinical features of ovarian cancer in Japanese women with germ-line mutations of BRCA1 . Clin Cancer Res. 1998; 4:235–240.11. Ben David Y, Chetrit A, Hirsh-Yechezkel G, Friedman E, Beck BD, Beller U, et al. Effect of BRCA mutations on the length of survival in epithelial ovarian tumors. J Clin Oncol. 2002; 20:463–466.12. Tan DS, Rothermundt C, Thomas K, Bancroft E, Eeles R, Shanley S, et al. “BRCAness” syndrome in ovarian cancer: a case-control study describing the clinical features and outcome of patients with epithelial ovarian cancer associated with BRCA1 and BRCA2 mutations. J Clin Oncol. 2008; 26:5530–5536.13. Frank TS, Deffenbaugh AM, Reid JE, Hulick M, Ward BE, Lingenfelter B, et al. Clinical characteristics of individuals with germline mutations in BRCA1 and BRCA2: analysis of 10,000 individuals. J Clin Oncol. 2002; 20:1480–1490.14. Easton DF, Deffenbaugh AM, Pruss D, Frye C, Wenstrup RJ, Allen-Brady K, et al. A systematic genetic assessment of 1,433 sequence variants of unknown clinical significance in the BRCA1 and BRCA2 breast cancer-predisposition genes. Am J Hum Genet. 2007; 81:873–883.15. Lindor NM, Goldgar DE, Tavtigian SV, Plon SE, Couch FJ. BRCA1/2 sequence variants of uncertain significance: a primer for providers to assist in discussions and in medical management. Oncologist. 2013; 18:518–524.16. Chern JY, Lee SS, Frey MK, Lee J, Blank SV. The influence of BRCA variants of unknown significance on cancer risk management decision-making. J Gynecol Oncol. 2019; 30:e60.
Article17. Radice P, De Summa S, Caleca L, Tommasi S. Unclassified variants in BRCA genes: guidelines for interpretation. Ann Oncol. 2011; 22:Suppl 1. i18–23.18. Pujade-Lauraine E, Ledermann JA, Selle F, Gebski V, Penson RT, Oza AM, et al. Olaparib tablets as maintenance therapy in patients with platinum-sensitive, relapsed ovarian cancer and a BRCA1/2 mutation (SOLO2/ENGOT-Ov21): a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 2017; 18:1274–1284.19. Stavropoulou AV, Fostira F, Pertesi M, Tsitlaidou M, Voutsinas GE, Triantafyllidou O, et al. Prevalence of BRCA1 mutations in familial and sporadic greek ovarian cancer cases. PLoS One. 2013; 8:e58182.
Article20. Janavičius R, Rudaitis V, Mickys U, Elsakov P, Griškevičius L. Comprehensive BRCA1 and BRCA2 mutational profile in Lithuania. Cancer Genet. 2014; 207:195–205.21. Lee JS, John EM, McGuire V, Felberg A, Ostrow KL, DiCioccio RA, et al. Breast and ovarian cancer in relatives of cancer patients, with and without BRCA mutations. Cancer Epidemiol Biomarkers Prev. 2006; 15:359–363.22. Modan B, Hartge P, Hirsh-Yechezkel G, Chetrit A, Lubin F, Beller U, et al. Parity, oral contraceptives, and the risk of ovarian cancer among carriers and noncarriers of a BRCA1 or BRCA2 mutation. N Engl J Med. 2001; 345:235–240.23. Boyd J, Sonoda Y, Federici MG, Bogomolniy F, Rhei E, Maresco DL, et al. Clinicopathologic features of BRCA-linked and sporadic ovarian cancer. JAMA. 2000; 283:2260–2265.24. Rodríguez AO, Llacuachaqui M, Pardo GG, Royer R, Larson G, Weitzel JN, et al. BRCA1 and BRCA2 mutations among ovarian cancer patients from Colombia. Gynecol Oncol. 2012; 124:236–243.25. Zhang S, Royer R, Li S, McLaughlin JR, Rosen B, Risch HA, et al. Frequencies of BRCA1 and BRCA2 mutations among 1,342 unselected patients with invasive ovarian cancer. Gynecol Oncol. 2011; 121:353–357.26. Tonin PN, Mes-Masson AM, Narod SA, Ghadirian P, Provencher D. Founder BRCA1 and BRCA2 mutations in French Canadian ovarian cancer cases unselected for family history. Clin Genet. 1999; 55:318–324.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Clinical Outcomes of BRCA1/2 Pathologic Mutation, Variants of Unknown Significance, or Wild Type Epithelial Ovarian Cancer Patients
- Prevalence of germline BRCA mutations among women with carcinoma of the peritoneum or fallopian tube
- Frequency of BRCA1 and BRCA2 Germline Mutations Detected by Protein Truncation Test and Cumulative Risks of Breast and Ovarian Cancer among Mutation Carriers in Japanese Breast Cancer Families
- Germline Mutations and polymorphisms of BRCA1 and BRCA2 in Sporadic Ovarian Carcinoma
- Reclassification of BRCA1 and BRCA2 variants found in ovarian epithelial, fallopian tube, and primary peritoneal cancers