Clin Nutr Res.
2019 Oct;8(4):329-335. 10.7762/cnr.2019.8.4.329.
Nutritional Intervention of a Pediatric Patient with Congenital Bronchomalacia and Gastroesophageal Reflux Disease: a Case Report
- Affiliations
-
- 1Department of Nutrition Care, Severance Hospital, Yonsei University Health System, Seoul 03772, Korea. hslee0730@yuhs.ac
- 2Department of Pediatrics, Severance Hospital, Yonsei University College of Medicine, Seoul 03772, Korea.
- KMID: 2461100
- DOI: http://doi.org/10.7762/cnr.2019.8.4.329
Abstract
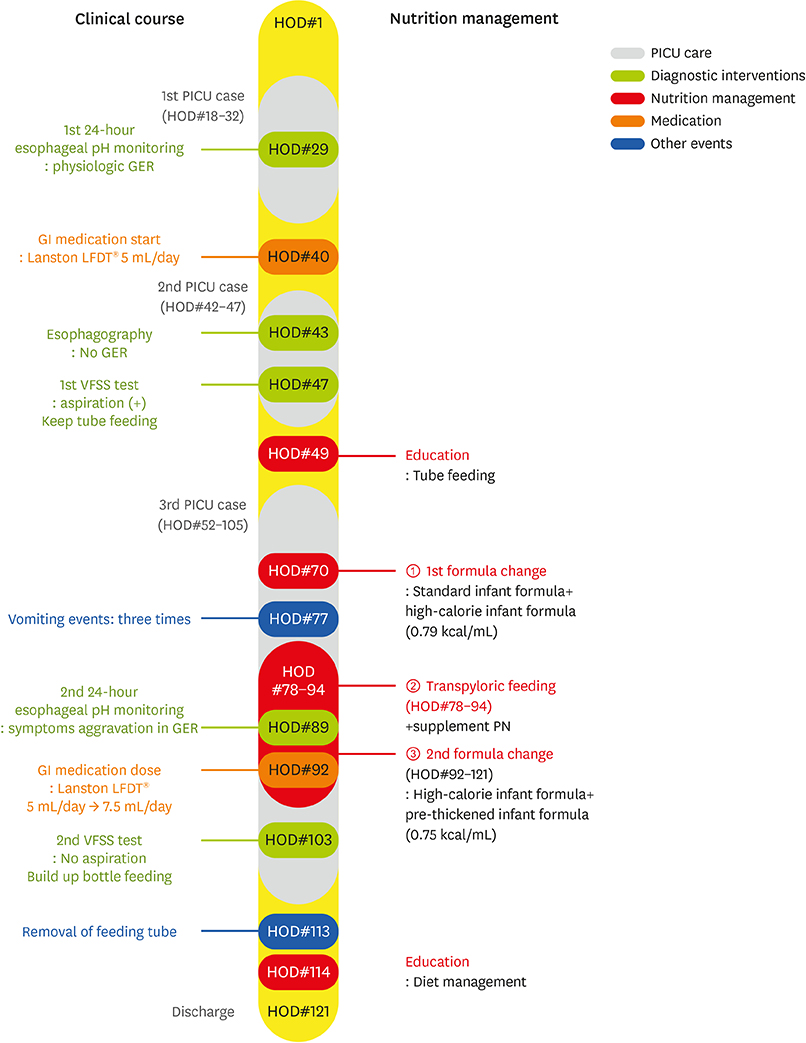
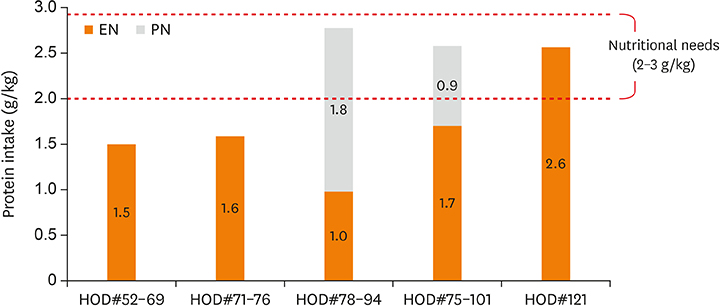
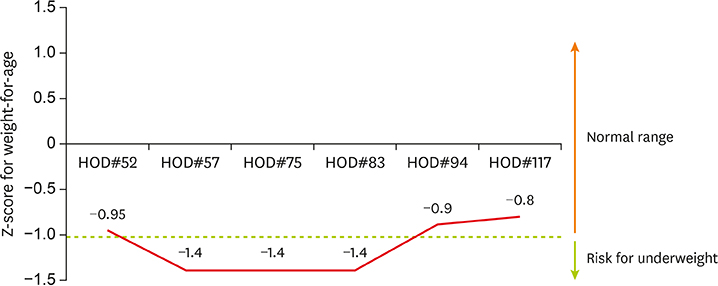
- Gastroesophageal reflux disease (GERD) is closely related to respiratory issues. We reported the case about the nutrition intervention given to a male infant with congenital bronchomalacia, GERD, and recurrent pneumonia. During the first and second pediatric intensive care unit (PICU) stays, his nutrition status and nutrient intake were good. However, during the 18 days of the third PICU admission, his nutrient intake decreased to 75%-80% of his estimated calorie requirement and his Z-score for weight-for-age dropped to −1.4. We conducted nutritional interventions to improve GERD symptoms and nutritional status include avoiding overfeeding by feeding small amounts frequently, using a pre-thickened formula mixed with a high-calorie formula, and feeding through transpyloric tube. As a result, his daily nutrient intakes gradually increased and his Z-score for weight-for-age was normal. In conclusion, it is important to implement individualized intensive nutritional management to ensure adequate nutrition and growth status in infants with lung disease and GERD.
Keyword
MeSH Terms
Figure
Reference
-
1. Rosen R, Vandenplas Y, Singendonk M, Cabana M, DiLorenzo C, Gottrand F, Gupta S, Langendam M, Staiano A, Thapar N, Tipnis N, Tabbers M. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr. 2018; 66:516–554.
Article2. American Society for Parenteral and Enteral Nutrition. The A.S.P.E.N. Pediatric nutrition support core curriculum. 2nd ed. Silver Spring (MD): American Society for Parenteral and Enteral Nutrition;2015. p. 390–392.3. Omari T, Barnett C, Snel A, Davidson G, Haslam R, Bakewell M, Dent J. Mechanism of gastroesophageal reflux in premature infants with chronic lung disease. J Pediatr Surg. 1999; 34:1795–1798.
Article4. Korean Dietetic Association. Manual of medical nutrition therapy. 3rd ed. Seoul: Korean Dietetic Association;2008. p. 194–195.5. Sondheimer JM. Gastroesophageal reflux: update on pathogenesis and diagnosis. Pediatr Clin North Am. 1988; 35:103–116.
Article6. Horvath A, Dziechciarz P, Szajewska H. The effect of thickened-feed interventions on gastroesophageal reflux in infants: systematic review and meta-analysis of randomized, controlled trials. Pediatrics. 2008; 122:e1268–77.
Article7. Chao HC, Vandenplas Y. Comparison of the effect of a cornstarch thickened formula and strengthened regular formula on regurgitation, gastric emptying and weight gain in infantile regurgitation. Dis Esophagus. 2007; 20:155–160.
Article8. Academy of Nutrition and Dietetics. Pediatric nutrition care manual [Internet]. 2019. cited 2019 October 15. Available from http://www.nutritioncaremanual.org.9. Malcolm WF, Smith PB, Mears S, Goldberg RN, Cotten CM. Transpyloric tube feeding in very low birthweight infants with suspected gastroesophageal reflux: impact on apnea and bradycardia. J Perinatol. 2009; 29:372–375.
Article10. Romano C, van Wynckel M, Hulst J, Broekaert I, Bronsky J, Dall'Oglio L, Mis NF, Hojsak I, Orel R, Papadopoulou A, Schaeppi M, Thapar N, Wilschanski M, Sullivan P, Gottrand F. European Society for Paediatric Gastroenterology, Hepatology and Nutrition guidelines for the evaluation and treatment of gastrointestinal and nutritional complications in children with neurological impairment. J Pediatr Gastroenterol Nutr. 2017; 65:242–264.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Sliding Hiatal Hernia associated with Bochdalek Hernia Repair
- A Case of Congenital Hypertrophic Pylocric Stenosis Associated with Gastroesophageal Reflux
- A case of bronchomalacia due to endobronchial tuberculosis
- A case of recurrent pneumonia due to gastroesophageal reflux after repair of TEF
- Percutaneous Endoscopic Jejunostomy in a Traumatic Brain Injured Patient with Subtotal Gastrectomy; A case report