Ann Pediatr Endocrinol Metab.
2019 Sep;24(3):164-171. 10.6065/apem.2019.24.3.164.
Basal serum luteinizing hormone value as the screening biomarker in female central precocious puberty
- Affiliations
-
- 1Department of Pediatrics, Dankook University Hospital, Dankook University College of Medicine, Cheonan, Korea. dryujs@dankook.ac.kr
- 2Department of Diagnostic Radiology, Dankook University Hospital, Dankook University College of Medicine, Cheonan, Korea.
- KMID: 2460763
- DOI: http://doi.org/10.6065/apem.2019.24.3.164
Abstract
- PURPOSE
Precocious puberty refers to the development of secondary sex characteristics before ages 8 and 9 years in girls and boys, respectively. Central precocious puberty (CPP) is caused by premature activation of the hypothalamus-pituitary-gonadal (HPG) axis and causes thelarche in girls before the age of 8. A gonadotropin-releasing hormone (GnRH) stimulation test is the standard diagnostic modality for diagnosing CPP. However, the test cannot always be used for screening because it is expensive and time-consuming. This study aimed to find alternative reliable screening parameters to identify HPG axis activation in girls <8 years old (CPP) and for girls 8-9 years old (early puberty, EP).
METHODS
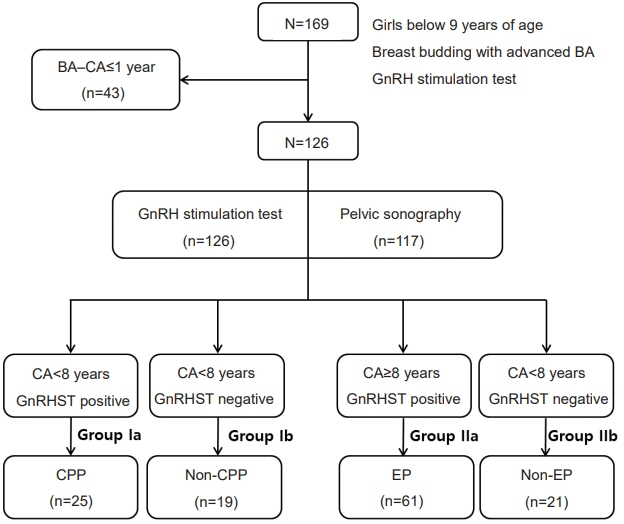
From January 2013 to June 2015, medical records from 196 girls younger than 9 years old with onset of breast development were reviewed, including 126 girls who had a bone age (BA) 1 year above their chronological age. All patients underwent a GnRH stimulation test, and 117 underwent pelvic sonography. The girls were divided into 4 groups based on age and whether the GnRH stimulation test showed evidence of central puberty. Subanalyses were also conducted within each group based on peak luteinizing hormone (LH) level quartiles.
RESULTS
Basal serum LH level was the most sensitive marker for screening CPP and EP. The cutoff values were 0.245 IU/L for CPP under 8 years old (P=0.049, area under the curve [AUC]=0.764, 88% sensitivity, 48% specificity) and 0.275 IU/L for EP between 8-9 years old (P=0.005, AUC=0.813, 79% sensitivity, 77% specificity). Peak LH level decreased as BMI z-score among subgroups increased when there was no difference in BA; however, higher BA eliminated this effect.
CONCLUSION
Basal serum LH level is a useful screening parameter for diagnosing CPP and EP in girls. Peak LH levels were lower with increasing BMI z-score, although older BA eliminated this effect.
MeSH Terms
Figure
Cited by 3 articles
-
Efficacy of Triptorelin 3-Month Depot Compared to 1-Month Depot for the Treatment of Korean Girls with Central Precocious Puberty in Single Tertiary Center
Lindsey Yoojin Chung, Eungu Kang, Hyo-Kyoung Nam, Young-Jun Rhie, Kee-Hyoung Lee
J Korean Med Sci. 2021;36(34):e219. doi: 10.3346/jkms.2021.36.e219.Diagnosis and Treatment of Central Precocious Puberty
Han Saem Choi, Ho-Seong Kim, Hyun Wook Chae
Ewha Med J. 2021;44(4):117-121. doi: 10.12771/emj.2021.44.4.117.Gonadotropin-releasing hormone stimulation test and diagnostic cutoff in precocious puberty: a mini review
Siti Nadirah Ab Rahim, Julia Omar, Tuan Salwani Tuan Ismail
Ann Pediatr Endocrinol Metab. 2020;25(3):152-155. doi: 10.6065/apem.2040004.002.
Reference
-
References
1. Partsch CJ, Sippell WG. Pathogenesis and epidemiology of precocious puberty. Effects of exogenous oestrogens. Hum Reprod Update. 2001; 7:292–302.2. Teilmann G, Pedersen CB, Jensen TK, Skakkebaek NE, Juul A. Prevalence and incidence of precocious pubertal development in Denmark: an epidemiologic study based on national registries. Pediatrics. 2005; 116:1323–8.3. Sørensen K, Mouritsen A, Aksglaede L, Hagen CP, Mogensen SS, Juul A. Recent secular trends in pubertal timing: implications for evaluation and diagnosis of precocious puberty. Horm Res Paediatr. 2012; 77:137–45.4. Aksglaede L, Sørensen K, Petersen JH, Skakkebaek NE, Juul A. Recent decline in age at breast development: the Copenhagen Puberty Study. Pediatrics. 2009; 123:e932–9.5. Willemsen RH, Elleri D, Williams RM, Ong KK, Dunger DB. Pros and cons of GnRHa treatment for early puberty in girls. Nat Rev Endocrinol. 2014; 10:352–63.6. Lakshman R, Forouhi NG, Sharp SJ, Luben R, Bingham SA, Khaw KT, et al. Early age at menarche associated with cardiovascular disease and mortality. J Clin Endocrinol Metab. 2009; 94:4953–60.7. Prentice P, Viner RM. Pubertal timing and adult obesity and cardiometabolic risk in women and men: a systematic review and meta-analysis. Int J Obes (Lond). 2013; 37:1036–43.8. Pescovitz OH, Hench KD, Barnes KM, Loriaux DL, Cutler GB Jr. Premature thelarche and central precocious puberty: the relationship between clinical presentation and the gonadotropin response to luteinizing hormone-releasing hormone. J Clin Endocrinol Metab. 1988; 67:474–9.9. Kim HK, Kee SJ, Seo JY, Yang EM, Chae HJ, Kim CJ. Gonadotropin-releasing hormone stimulation test for precocious puberty. Korean J Lab Med. 2011; 31:244–9.10. Lee DS, Ryoo NY, Lee SH, Kim S, Kim JH. Basal luteinizing hormone and follicular stimulating hormone: is it sufficient for the diagnosis of precocious puberty in girls? Ann Pediatr Endocrinol Metab. 2013; 18:196–201.11. Lee HS, Park HK, Ko JH, Kim YJ, Hwang JS. Utility of Basal luteinizing hormone levels for detecting central precocious puberty in girls. Horm Metab Res. 2012; 44:851–4.12. Pasternak Y, Friger M, Loewenthal N, Haim A, Hershkovitz E. The utility of basal serum LH in prediction of central precocious puberty in girls. Eur J Endocrinol. 2012; 166:295–9.13. Çatlı G, Erdem P, Anık A, Abacı A, Böber E. Clinical and laboratory findings in the differential diagnosis of central precocious puberty and premature thelarche. Turk Pediatri Ars. 2015; 50:20–6.14. Yu J, Shin HY, Lee SH, Kim YS, Kim JH. Usefulness of pelvic ultrasonography for the diagnosis of central precocious puberty in girls. Korean J Pediatr. 2015; 58:294–300.15. Lee SH, Joo EY, Lee JE, Jun YH, Kim MY. The diagnostic value of pelvic ultrasound in girls with central precocious puberty. Chonnam Med J. 2016; 52:70–4.16. de Vries L, Horev G, Schwartz M, Phillip M. Ultrasonographic and clinical parameters for early differentiation between precocious puberty and premature thelarche. Eur J Endocrinol. 2006; 154:891–8.17. Neely EK, Wilson DM, Lee PA, Stene M, Hintz RL. Spontaneous serum gonadotropin concentrations in the evaluation of precocious puberty. J Pediatr. 1995; 127:47–52.18. Lee PA. Laboratory monitoring of children with precocious puberty. Arch Pediatr Adolesc Med. 1994; 148:369–76.19. Suh J, Choi MH, Kwon AR, Kim YJ, Jeong JW, Ahn JM, et al. Factors that predict a positive response on gonadotropinreleasing hormone stimulation test for diagnosing central precocious puberty in girls. Ann Pediatr Endocrinol Metab. 2013; 18:202–7.20. Supornsilchai V, Hiranrat P, Wacharasindhu S, Srivuthana S, Aroonparkmongkol S. Basal luteinizing hormone/follicle stimulating hormone ratio in diagnosis of central precocious puberty. J Med Assoc Thai. 2003; 86 Suppl 2:S145–51.21. Fu JF, Liang JF, Zhou XL, Prasad HC, Jin JH, Dong GP, et al. Impact of BMI on gonadorelin-stimulated LH peak in premenarcheal girls with idiopathic central precocious puberty. Obesity (Silver Spring). 2015; 23:637–43.22. Lee HS, Park HK, Ko JH, Kim YJ, Hwang JS. Impact of body mass index on luteinizing hormone secretion in gonadotropin-releasing hormone stimulation tests of boys experiencing precocious puberty. Neuroendocrinology. 2013; 97:225–31.23. Lee HS, Yoon JS, Hwang JS. Luteinizing hormone secretion during gonadotropin-releasing hormone stimulation tests in obese girls with central precocious puberty. J Clin Res Pediatr Endocrinol. 2016; 8:392–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of idiopathic precocious puberty treated with a luteinizing hormone relaeasing hormone analog
- The Utility of Basal Serum Luteinizing Hormone Levels for Screening Central Precocious Puberty in Girls
- Diurnal variation of gonadotropin levels in girls with early stages of puberty
- The Influence of Body Mass Index on Luteinizing Hormone Levels after Gonadotropin-Releasing Hormone Stimulation in Girls with Precocious and Advanced Puberty
- Morning basal luteinizing hormone, a good screening tool for diagnosing central precocious puberty