J Pathol Transl Med.
2019 Sep;53(5):332-336. 10.4132/jptm.2019.07.12.
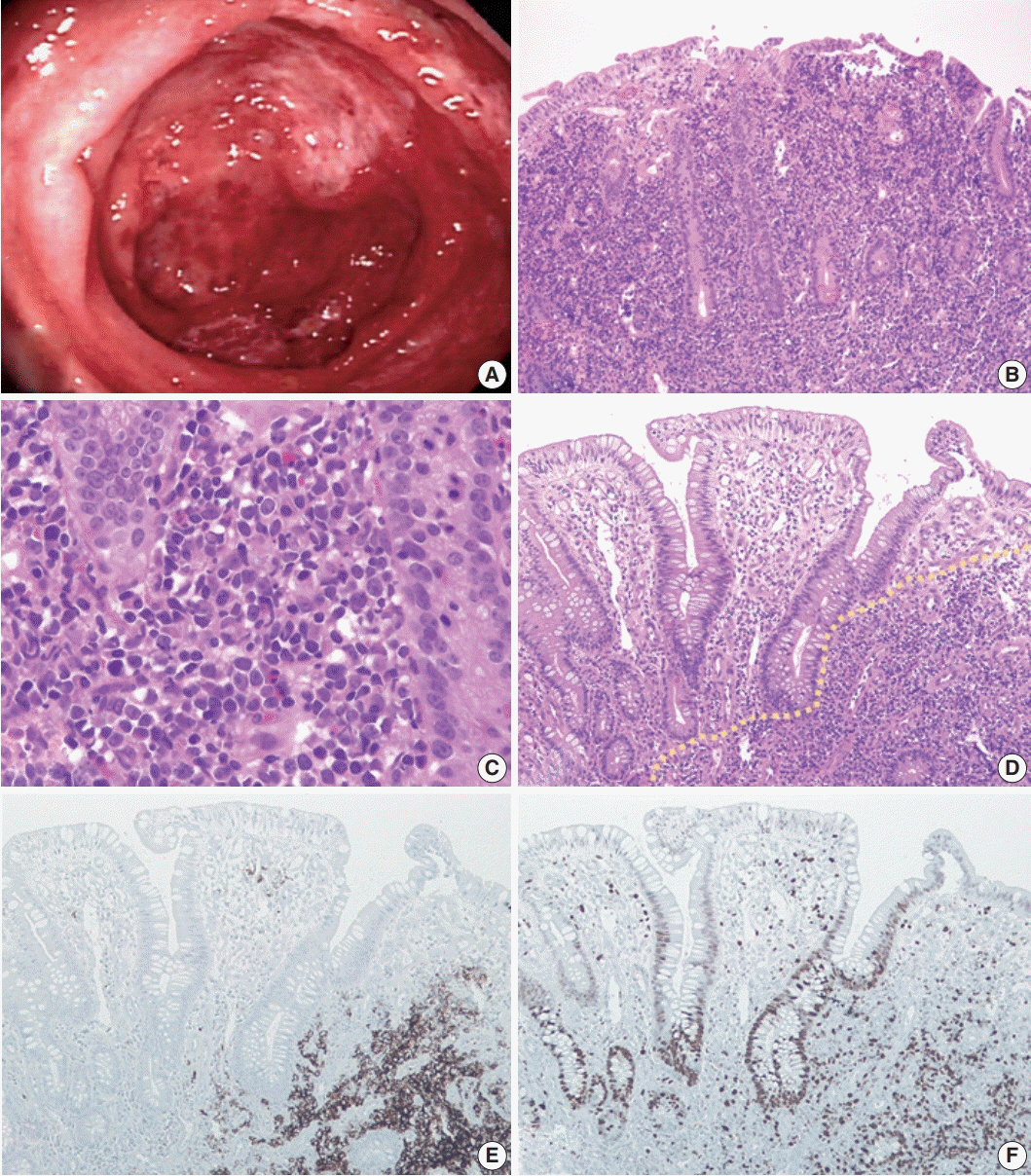
Diffuse Involvement of Primary Colorectal Lymphoma Simulating Ulcerative Colitis
- Affiliations
-
- 1Department of Pathology, Inje University Ilsan Paik Hospital, Goyang, Korea. mjoo@paik.ac.kr
- KMID: 2459582
- DOI: http://doi.org/10.4132/jptm.2019.07.12
Abstract
- Diffuse involvement of colorectal lymphoma masquerading as colitis is a very rare presentation of primary colorectal lymphoma. Detecting occult lymphoma is difficult in the setting of diffuse colonic involvement with no definite mass and inflammatory mucosal changes. We encountered a case of diffuse-type primary colorectal lymphoma simulating ulcerative colitis in a previously healthy 31-year-old woman. Despite multiple mucosal biopsies, the biopsy diagnosis was not made due to unawareness of atypical lymphocytes admixed with dense lymphoplasmacytic infiltration. The present case emphasizes the importance of being aware of this rare presentation of primary colorectal lymphoma in order to avoid misdiagnosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Wong MT, Eu KW. Primary colorectal lymphomas. Colorectal Dis. 2006; 8:586–91.
Article2. Friedman HB, Silver GM, Brown CH. Lymphoma of the colon simulating ulcerative colitis: report of four cases. Am J Dig Dis. 1968; 13:910–7.3. Weir AB, Poon MC, Groarke JF, Wilkerson JA. Lymphoma simulating Crohn’s colitis. Dig Dis Sci. 1980; 25:69–72.
Article4. McCullough JE, Kim CH, Banks PM. Mantle zone lymphoma of the colon simulating diffuse inflammatory bowel disease: role of immunohistochemistry in establishing the diagnosis. Dig Dis Sci. 1992; 37:934–8.5. Lenzen R, Borchard F, Lübke H, Strohmeyer G. Colitis ulcerosa complicated by malignant lymphoma: case report and analysis of published works. Gut. 1995; 36:306–10.
Article6. Robert ME, Kuo FC, Longtine JA, Sklar JL, Schrock T, Weidner N. Diffuse colonic mantle cell lymphoma in a patient with presumed ulcerative colitis: detection of a precursor monoclonal lymphoid population using polymerase chain reaction and immunohistochemistry. Am J Surg Pathol. 1996; 20:1024–31.7. Hirakawa K, Fuchigami T, Nakamura S, et al. Primary gastrointestinal T-cell lymphoma resembling multiple lymphomatous polyposis. Gastroenterology. 1996; 111:778–82.
Article8. Son HJ, Rhee PL, Kim JJ, et al. Primary T-cell lymphoma of the colon. Korean J Intern Med. 1997; 12:238–41.
Article9. Isomoto H, Furusu H, Onizuka Y, et al. Colonic involvement by adult T-cell leukemia/lymphoma mimicking ulcerative colitis. Gastrointest Endosc. 2003; 58:805–8.
Article10. Payne S, Phillips M, Reffitt D, et al. An unusual case of colitis. Gut. 2004; 53:1824.
Article11. Tamura S, Ohkawauchi K, Yokoyama Y, et al. Non-multiple lymphomatous polyposis form of mantle cell lymphoma in the gastrointestinal tract. J Gastroenterol. 2004; 39:995–1000.
Article12. Berkelhammer C, Mohammed A, Zalzaleh G, Grela J, Blumstein A, Stein R. Spontaneous multiperforation in lymphomatous colitis masquerading as Crohn’s disease: 2 cases. Inflamm Bowel Dis. 2008; 14:1172–3.
Article13. Koksal AS, Taskiran I, Kalkan IH, Kayacetin E. A rare endoscopic appearance of primary gastrointestinal mantle cell lymphoma resembling ulcerative colitis. Bratisl Lek Listy. 2014; 115:800–1.
Article14. Zaheen A, Delabie J, Vajpeyi R, Frost DW. The first report of a previously undescribed EBV-negative NK-cell lymphoma of the GI tract presenting as chronic diarrhoea with eosinophilia. BMJ Case Rep. 2015; 2015:bcr2015212103.
Article15. Wu PH, Chu KE, Lin YM, Huang SH, Wu CC. T-cell lymphomas presenting as colon ulcers and eosinophilia. Case Rep Gastroenterol. 2015; 9:246–52.
Article16. Cheung FM, Tong Y, Wang Y, et al. Epstein-Barr virus-positive T-cell-associated colitis mimicking inflammatory bowel disease: clinicopathological study of two cases. Histopathology. 2016; 68:465–8.
Article17. Zenda T, Nakagawa N, Maruyama H, et al. Follicular lymphoma-related colitis resembling ulcerative colitis. Clin J Gastroenterol. 2017; 10:147–53.
Article18. Farrell RJ, Ang Y, Kileen P, et al. Increased incidence of non-Hodgkin’s lymphoma in inflammatory bowel disease patients on immunosuppressive therapy but overall risk is low. Gut. 2000; 47:514–9.
Article19. Dawson IM, Cornes JS, Morson BC. Primary malignant lymphoid tumours of the intestinal tract. Report of 37 cases with a study of factors influencing prognosis. Br J Surg. 1961; 49:80–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Non-Hodgkin's Lymphoma in Ulcerative Colitis
- A Case of Malignant Lymphoma in Patient with Ulcerative Colitis
- Crossroad between inflammation and carcinogenesis in colon
- Recent Advances in Understanding Colorectal Cancer and Dysplasia Related to Ulcerative Colitis
- Risks of colorectal cancer and biliary cancer according to accompanied primary sclerosing cholangitis in Korean patients with ulcerative colitis: a nationwide population-based study