Ann Surg Treat Res.
2019 Oct;97(4):168-175. 10.4174/astr.2019.97.4.168.
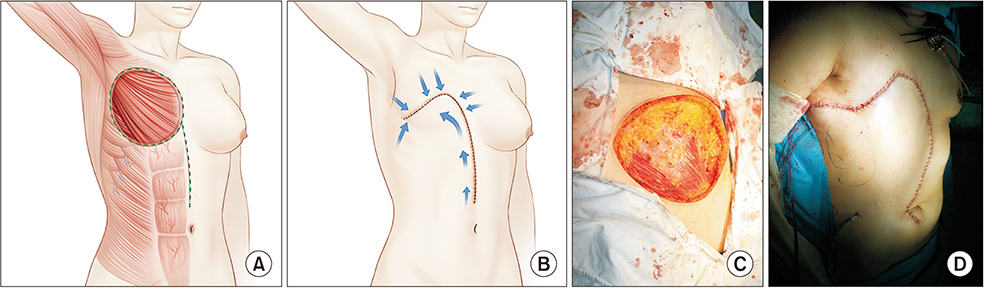
Single vertical incision thoracoabdominal flap for chest wall reconstruction following mastectomy of locally advanced breast cancer
- Affiliations
-
- 1Department of Plastic Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. nicekek@korea.com
- 2Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2459314
- DOI: http://doi.org/10.4174/astr.2019.97.4.168
Abstract
- PURPOSE
Skin grafts have been widely used in managing extensive chest wall defects after mastectomy for advanced breast cancer. However, their durability and tolerability to radiotherapy is still controversial. A thoracoabdominal (TA) flap with a few technical refinements can safely transfer a larger flap while minimizing complications.
METHODS
From January 2007 to February 2018, a retrospective review was performed to compare 2 groups after wide breast excision: skin graft group (group 1) and lateral-based, single vertical incision rotation-advancement TA flap (group 2). Patients' demographics, operative details, complications, hospital stay, postoperative outpatient visits, cost, and start of adjuvant therapy were analyzed between the 2 groups.
RESULTS
During the study period, 34 patients received skin graft and 41 patients received TA flap. group 2 had a shorter hospital stay (6.41 ± 2.64 days vs. 12.62 ± 4.60 days, P < 0.001) and shorter time to complete wound healing (29.27 ± 18.68 days vs. 39.24 ± 27.70 days, P = 0.03) than group 1. There was also a difference in the period from surgery to initiation of adjuvant therapy (group 1, 45.04 days ± 17.79 days; group 2, 37.07 ± 15.38 days, P = 0.073). Although limitation in shoulder motion was more frequent in group 2, limitation of motion for >1 year was observed in 4 patients in only group 1 (43.90% vs. 38.24%, P = 0.613).
CONCLUSION
TA flap has a simple design that minimizes concerns involving the donor site. Moreover, it does not require complicated procedures and allows for re-elevation whenever necessary. Finally, it guarantees faster wound recovery than skin graft with fewer complications.
Keyword
MeSH Terms
Figure
Reference
-
1. Woo E, Tan BK, Koong HN, Yeo A, Chan MY, Song C. Use of the extended V-Y latissimus dorsi myocutaneous flap for chest wall reconstruction in locally advanced breast cancer. Ann Thorac Surg. 2006; 82:752–755.
Article2. Charanek AM. A bilobed thoracoabdominal myocutaneous flap for large thoracic defects. Ann Plast Surg. 2014; 72:451–456.
Article3. Davis WM, McCraw JB, Carraway JH. Use of a direct, transverse, thoracoabdominal flap to close difficult wounds of the thorax and upper extremity. Plast Reconstr Surg. 1977; 60:526–533.
Article4. Baroudi R, Pinotti JA, Keppke EM. A transverse thoracoabdominal skin flap for closure after radical mastectomy. Plast Reconstr Surg. 1978; 61:547–554.
Article5. Park JS, Ahn SH, Son BH, Kim EK. Using local flaps in a chest wall reconstruction after mastectomy for locally advanced breast cancer. Arch Plast Surg. 2015; 42:288–294.
Article6. Bui DT, Chunilal A, Mehrara BJ, Disa JJ, Alektiar KM, Cordeiro PG. Outcome of split-thickness skin grafts after external beam radiotherapy. Ann Plast Surg. 2004; 52:551–556.
Article7. Persichetti P, Brunetti B, Cagli B, Tenna S. Chest wall reconstruction with the perforator-plus thoracoabdominal flap. Plast Reconstr Surg. 2012; 130:488e–489e.
Article8. Vieira RADC, da Silva KMT, de Oliveira-Junior I, de Lima MA. ITADE flap after mastectomy for locally advanced breast cancer: a good choice for mid-sized defects of the chest wall, based on a systematic review of thoracoabdominal flaps. J Surg Oncol. 2017; 115:949–958.
Article9. Cogliandro A, Cagli B, Filoni A, Cassotta G, Tenna S, Persichetti P. Expander/Implant breast reconstruction after reconstruction using an extended cutaneous thoracoabdominal flap: a case report. J Breast Cancer. 2013; 16:438–441.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Expander/Implant Breast Reconstruction after Reconstruction Using an Extended Cutaneous Thoracoabdominal Flap: A Case Report
- Immediate Breast and Chest Wall Reconstruction for Advanced Breast Cancer
- Chest Wall Reconstruction with Thoracoabdominal Flap for Large Skin Defects after Mastectomy of Advanced Breast Cancer
- External Oblique Myocutaneous Flap for Reconstruction of Large Chest-Wall Defects following Resection of Advanced Breast Cancer
- Using Local Flaps in a Chest Wall Reconstruction after Mastectomy for Locally Advanced Breast Cancer