J Gastric Cancer.
2019 Sep;19(3):355-364. 10.5230/jgc.2019.19.e30.
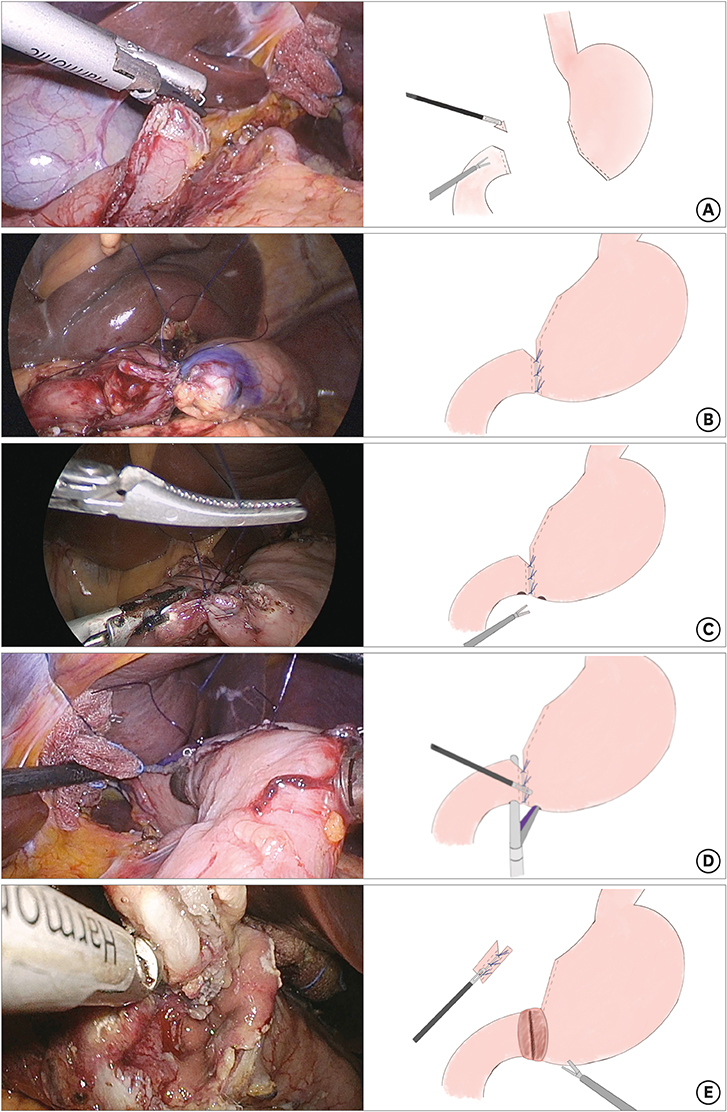
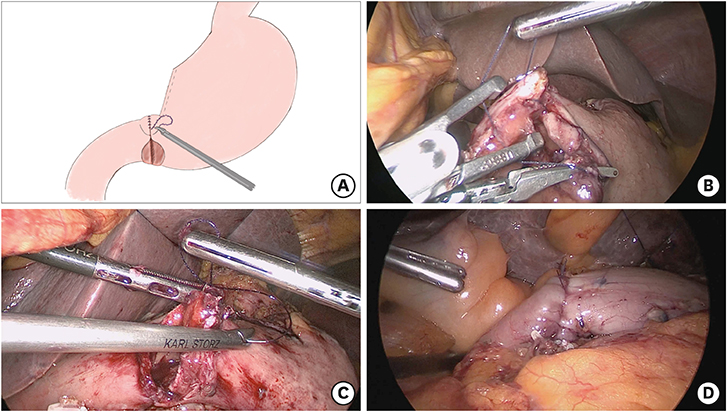
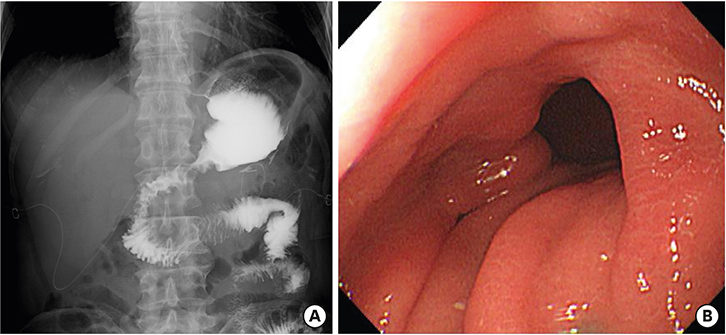
Modified Book Binding Technique (MBBT) for Intracorporeal Gastroduodenostomy in Totally Laparoscopic Distal Gastrectomy: Initial Experience
- Affiliations
-
- 1Department of Surgery, Ulsan University Hospital, Ulsan, Korea. parkdongjin7907@gmail.com
- 2Department of Surgery, University of Ulsan College of Medicine, Ulsan, Korea.
- KMID: 2458834
- DOI: http://doi.org/10.5230/jgc.2019.19.e30
Abstract
- Totally laparoscopic distal gastrectomy (TLDG) frequently involves the use of delta shaped gastroduodenostomy (DSG) for intracorporeal anastomosis. However, DSG has some drawbacks, and the book binding technique (BBT) was developed as a new technique to overcome these drawbacks. Subsequently, this technique was further improved with the development of modified book binding technique (MBBT). This study evaluated the safety and feasibility of MBBT in patients undergoing TLDG. Thirty-three patients who underwent TLDG with MBBT were retrospectively evaluated. The mean operation time was 277.6±37.1 minutes, including 51.9±15.7 minutes for reconstruction. Two patients had anastomosis-related complications, one patient with stricture after leakage and 1 patient with stenosis. The former patient was treated with endoscopic balloon dilatation, and the latter was managed conservatively; neither required re-operation. MBBT is a safe and feasible technique, with acceptable surgical outcomes. It may be a good alternative option for the treatment of intracorporeal anastomosis in patients undergoing TLDG.
Keyword
MeSH Terms
Figure
Reference
-
1. Kanaya S, Gomi T, Momoi H, Tamaki N, Isobe H, Katayama T, et al. Delta-shaped anastomosis in totally laparoscopic Billroth I gastrectomy: new technique of intraabdominal gastroduodenostomy. J Am Coll Surg. 2002; 195:284–287.2. Tanimura S, Higashino M, Fukunaga Y, Takemura M, Nishikawa T, Tanaka Y, et al. Intracorporeal Billroth 1 reconstruction by triangulating stapling technique after laparoscopic distal gastrectomy for gastric cancer. Surg Laparosc Endosc Percutan Tech. 2008; 18:54–58.
Article3. Noshiro H, Iwasaki H, Miyasaka Y, Kobayashi K, Masatsugu T, Akashi M, et al. An additional suture secures against pitfalls in delta-shaped gastroduodenostomy after laparoscopic distal gastrectomy. Gastric Cancer. 2011; 14:385–389.
Article4. Ikeda T, Kawano H, Hisamatsu Y, Ando K, Saeki H, Oki E, et al. Progression from laparoscopic-assisted to totally laparoscopic distal gastrectomy: comparison of circular stapler (i-DST) and linear stapler (BBT) for intracorporeal anastomosis. Surg Endosc. 2013; 27:325–332.
Article5. Huang C, Lin M, Chen Q, Lin J, Zheng C, Li P, et al. A modified delta-shaped gastroduodenostomy in totally laparoscopic distal gastrectomy for gastric cancer: a safe and feasible technique. PLoS One. 2014; 9:e102736.
Article6. Jang CE, Lee SI. Modified intracorporeal gastroduodenostomy in totally laparoscopic distal gastrectomy for gastric cancer: early experience. Ann Surg Treat Res. 2015; 89:306–312.
Article7. Byun C, Cui LH, Son SY, Hur H, Cho YK, Han SU. Linear-shaped gastroduodenostomy (LSGD): safe and feasible technique of intracorporeal Billroth I anastomosis. Surg Endosc. 2016; 30:4505–4514.
Article8. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.9. Kubo M, Sasako M, Gotoda T, Ono H, Fujishiro M, Saito D, et al. Endoscopic evaluation of the remnant stomach after gastrectomy: proposal for a new classification. Gastric Cancer. 2002; 5:83–89.
Article10. Cristaudi A, Matthey-Gié ML, Demartines N, Christoforidis D. Prospective assessment of trocar-specific morbidity in laparoscopy. World J Surg. 2014; 38:3089–3096.
Article11. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017; 20:1–19.12. Guideline Committee of the Korean Gastric Cancer Association (KGCA). Development Working Group & Review Panel. Korean practice guideline for gastric cancer 2018: an evidence-based, multi-disciplinary approach. J Gastric Cancer. 2019; 19:1–48.13. Yoshida M, Koga S, Ishimaru K, Yamamoto Y, Matsuno Y, Akita S, et al. Laparoscopy-assisted distal gastrectomy is feasible also for elderly patients aged 80 years and over: effectiveness and long-term prognosis. Surg Endosc. 2017; 31:4431–4437.
Article14. Song HM, Lee SL, Hur H, Cho YK, Han SU. Linear-shaped gastroduodenostomy in totally laparoscopic distal gastrectomy. J Gastric Cancer. 2010; 10:69–74.
Article15. Kim JJ, Song KY, Chin HM, Kim W, Jeon HM, Park CH, et al. Totally laparoscopic gastrectomy with various types of intracorporeal anastomosis using laparoscopic linear staplers: preliminary experience. Surg Endosc. 2008; 22:436–442.
Article16. Oki E, Tsuda Y, Saeki H, Ando K, Imamura Y, Nakashima Y, et al. Book-binding technique for Billroth I anastomosis during totally laparoscopic distal gastrectomy. J Am Coll Surg. 2014; 219:e69–e73.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intracorporeal Anastomosis in Laparoscopic Gastric Cancer Surgery
- Modified intracorporeal gastroduodenostomy in totally laparoscopic distal gastrectomy for gastric cancer: early experience
- The Early Experience with a Totally Laparoscopic Distal Gastrectomy
- Linear-Shaped Gastroduodenostomy in Totally Laparoscopic Distal Gastrectomy
- Intracorporeal Anastomosis Using Linear Stapler in Laparoscopic Distal Gastrectomy: Comparison between Gastroduodenostomy and Gastrojejunostomy