J Gastric Cancer.
2010 Jun;10(2):69-74.
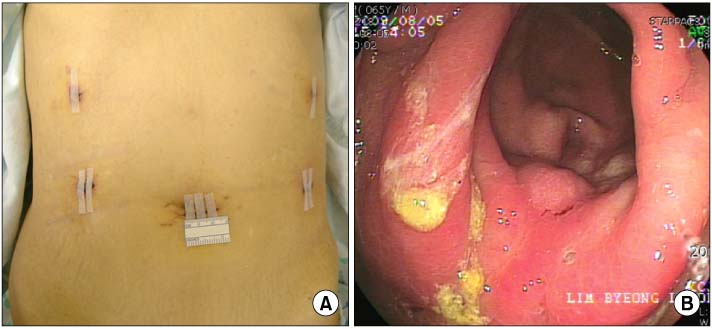
Linear-Shaped Gastroduodenostomy in Totally Laparoscopic Distal Gastrectomy
- Affiliations
-
- 1Department of Surgery, Ajou University Hospital, Suwon, Korea. hansu@ajou.ac.kr
Abstract
- PURPOSE
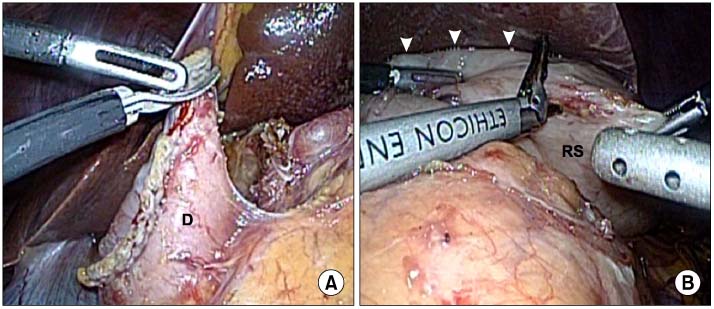
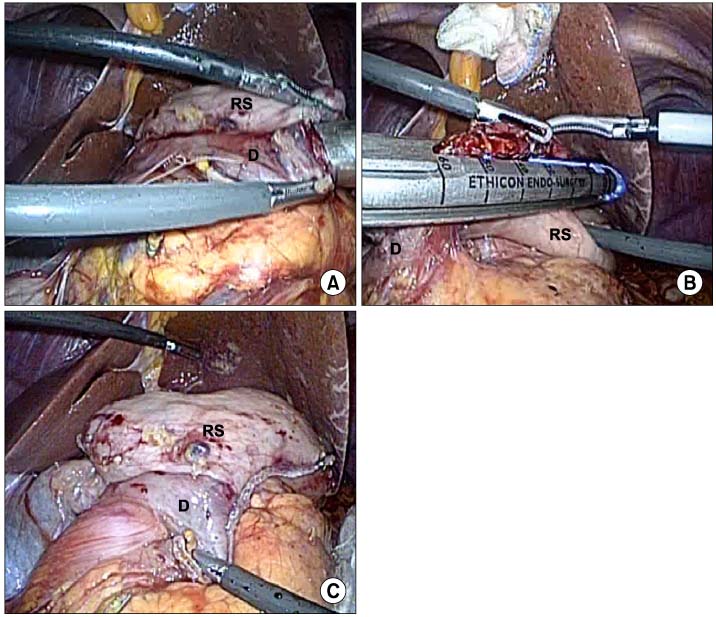
Laparoscopic gastrectomy has been common treatment modality for gastric cancer. But, most surgeons tend to perform laparoscopy-assisted distal gastrectomy using epigastric incision. Delta-shaped anastomosis is known as intracorporeal gastroduodenostomy, but it is technically difficult and needed many staplers. So we tried to find simple and economical method, here we report on the results of liner-shaped gastroduodenostomy in totally laparoscopic distal gastrectomy.
MATERIALS AND METHODS
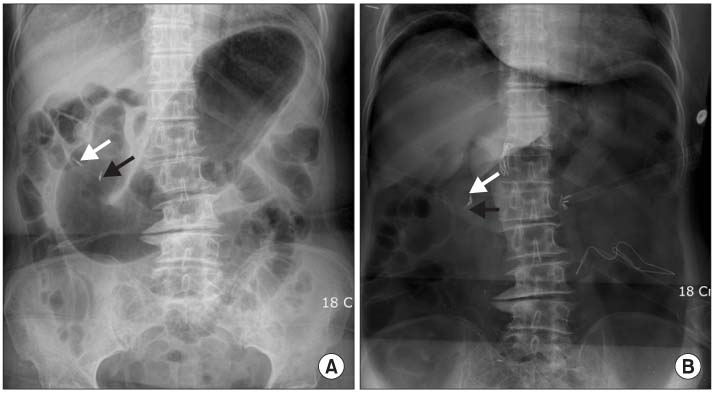
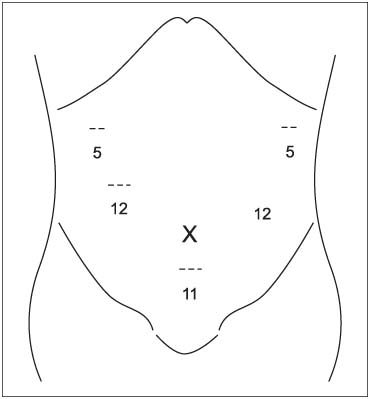
We retrospectively reviewed the medical records of 25 patients who underwent totally laparoscopic distal gastrectomy using liner-shaped anastomosis at School of Medicine, Ajou University between January to October 2009. The indication was early gastric cancer as diagnosed by preoperative workup, the anastomoses were performed by using laparoscopic linear stapler.
RESULTS
There were 12 female and 13 male patients with a mean age of 55.6+/-11.2. The following procedures were performed 14 laparoscopic gastrectomies, 11 robotic gastrectomies. The mean operation time was 179.5+/-27.4 minutes, the mean anastomotic time was 17.5+/-3.4 minutes. The mean number of stapler cartridges was 5.6+/-0.8. Postoperative complication occurred in one patient, anastomotic stenosis, and the patient required reoperation to gastrojejunostomy. The mean length of postoperative hospital stay was 6.7+/-1.0 days except the complication case, and there was no case of conversion to open procedure and postoperative mortality.
CONCLUSIONS
Linear-shaped gastroduodenostomy in totally laparoscopic distal gastrectomy is technically simple and feasible method.
MeSH Terms
Figure
Reference
-
1. Kitano S, Iso Y, Moriyama M, Sugimachi K. Laparoscopy-assisted billroth i gastrectomy. Surg Laparosc Endosc. 1994. 4:146–148.2. Kitano S, Shiraishi N, Fujii K, Yasuda K, Inomata M, Adachi Y. A randomized controlled trial comparing open vs laparoscopy-assisted distal gastrectomy for the treatment of early gastric cancer: an interim report. Surgery. 2002. 131:1 Suppl. S306–S311.
Article3. Kim MC, Kim KH, Kim HH, Jung GJ. Comparison of laparoscopy-assisted by conventional open distal gastrectomy and extraperigastric lymph node dissection in early gastric cancer. J Surg Oncol. 2005. 91:90–94.
Article4. Hosono S, Arimoto Y, Ohtani H, Kanamiya Y. Meta-analysis of short-term outcomes after laparoscopy-assisted distal gastrectomy. World J Gastroenterol. 2006. 12:7676–7683.
Article5. Kitano S, Shiraish N, Uyama I, Sugihara K, Tanigawa N. Japanese Laparoscopic Surgery Study Group. A multicenter study on oncologic outcome of laparoscopic gastrectomy for early cancer in Japan. Ann Surg. 2007. 245:68–72.
Article6. Kanaya S, Gomi T, Momoi H, Tamaki N, Isobe H, Katayama T, et al. Delta-shaped anastomosis in totally laparoscopic billroth i gastrectomy: new technique of intraabdominal gastroduodenostomy. J Am Coll Surg. 2002. 195:284–287.
Article7. Kim JJ, Kim SK, Jun KH, Kang HC, Song KY, Chin HM, et al. Clinical usefulness of a totally laparoscopic gastrectomy. J Korean Gastric Cancer Assoc. 2007. 7:132–138.
Article8. Kim HH. Laparoscopic Billroth II gastrectomy for benign gastric disease. J Korean Soc Endosc Laparosc Surg. 1999. 2:11–18.9. Kim HH, Kim KH, Kim DH, Kim C, Kim BS, Kim YW, et al. Korean Laparoscopic Gastrointestinal Surgery Study Group. Nationwide survey of laparoscopic gastric surgery in Korea, 2004. J Korean Gastric Cancer Assoc. 2005. 5:295–303.
Article10. Le Blanc-Louvry I, Ducrotte P, Peillon C, Michel P, Chiron A, Denis P. Roux-en-Y limb motility after total or distal gastrectomy in symptomatic and asymptomatic patients. J Am Coll Surg. 2000. 190:408–417.
Article11. Le Blanc-Louvry I, Ducrotte P, Chayvialle JA, Coquerel A, Michot F, Ténière P. Distal gastrectomy and Roux-Y limb in the rat: plasma motilin, pancreatic polypeptide concentrations, and duodenojejunal motility. Dig Dis Sci. 2000. 45:1525–1530.12. Meyer BM, Werth BA, Beglinger C, Hildebrand P, Jansen JB, Zach D, et al. Role of cholecystokinin in regulation of gastrointestinal motor functions. Lancet. 1989. 2:12–15.
Article13. van der Mijle HC, Beekhuis H, Bleichrodt RP, Kleibeuker JH. Transit disorders of the gastric remnant and Roux limb after Rouxen-Y gastrojejunostomy: relation to symptomatology and vagotomy. Br J Surg. 1993. 80:60–64.
Article14. Csendes A, Burgos AM, Smok G, Burdiles P, Braghetto I, Diaz JC. Latest result (12~21 years) of a prospective randomized study comparing billroth II and Roux-en-Y anastomosis after a partial gastrectomy plus vagotomy in patients with duodenal ulcers. Ann Surg. 2009. 249:189–194.
Article15. Chan DC, Fan YM, Lin CK, Chen CJ, Chen CY, Chao YC. Roux-en-Y reconstruction after distal gastrectomy to reduce enterogastric reflux and helicobacter pylori infection. J Gastrointest Surg. 2007. 11:1732–1740.
Article16. Fukuhara K, Osugi H, Takada N, Takemura M, Higashino M, Kinoshita H. Reconstructive procedure after distal gastrectomy for gastric cancer that best prevents duodenogastroesophageal reflux. World J Surg. 2002. 26:1452–1457.
Article17. Sah BK, Zhu ZG, Chen MM, Yan M, Yin HR, Zhen LY. Gastric cancer surgery and its hazards: post operative infection is the most important complication. Hepatogastroenterology. 2008. 55:2259–2263.18. Sah BK, Zhu ZG, Chen MM, Xiang M, Chen J, Yan M, et al. Effect of surgical work volume on postoperative complication: superiority of specialized center in gastric cancer treatment. Langenbecks Arch Surg. 2009. 394:41–47.
Article19. Hyung WJ, Lim JS, Cheong JH, Kim J, Choi SH, Song SY, et al. Intraoperative tumor localization using laparoscopic ultrasonography in laparoscopic-assisted gastrectomy. Surg Endosc. 2005. 19:1353–1357.
Article20. Tanimura S, Higashino M, Fukunaga Y, Osugi H. Laparoscopic distal gastrectomy with regional lymph node dissection for gastric cancer. Surg Endosc. 2003. 17:758–762.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Delta-Shaped Gastroduodenostomy after Totally Laparoscopic Distal Gastrectomy: A Comparison Analysis between Early and Late Experience
- The Early Experience with a Totally Laparoscopic Distal Gastrectomy
- Intracorporeal Anastomosis in Laparoscopic Gastric Cancer Surgery
- Comparison of Laparoscopy-Assisted and Totally Laparoscopic Distal Gastrectomy: The Short-Term Outcome at a Low Volume Center
- Feasibility of Linear-Shaped Gastroduodenostomy during the Performance of Totally Robotic Distal Gastrectomy