Korean J Gastroenterol.
2019 Sep;74(3):175-182. 10.4166/kjg.2019.74.3.175.
Pancreatitis, Panniculitis, and Polyarthritis Syndrome Simulating Cellulitis and Gouty Arthritis
- Affiliations
-
- 1Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Korea. onesbi@gmail.com
- 2Department of Anatomic Pathology, Kangwon National University School of Medicine, Chuncheon, Korea.
- KMID: 2458699
- DOI: http://doi.org/10.4166/kjg.2019.74.3.175
Abstract
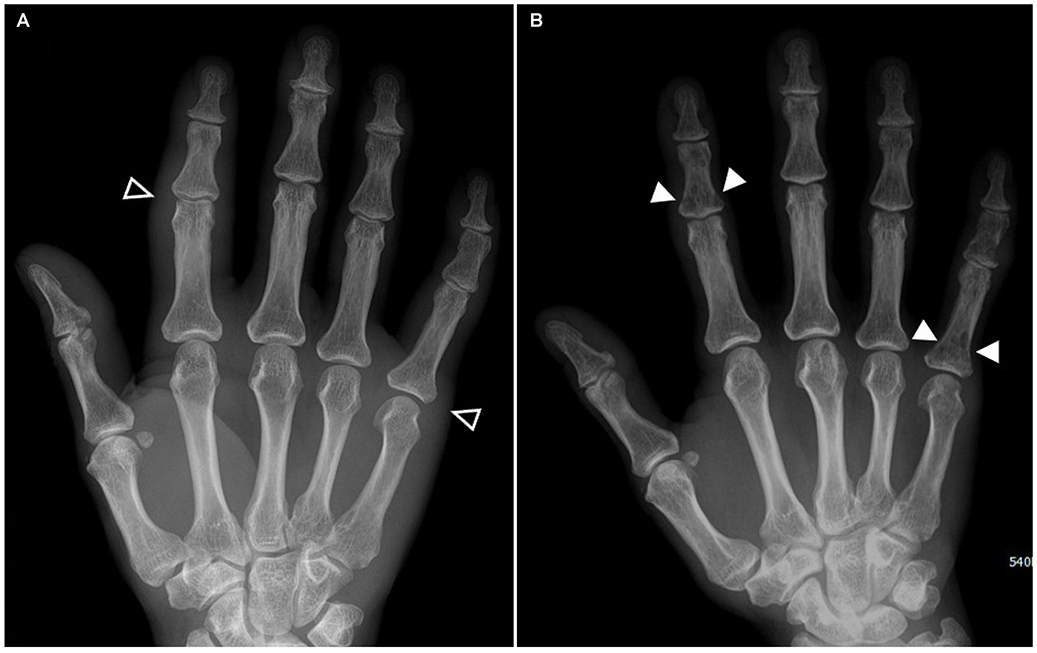
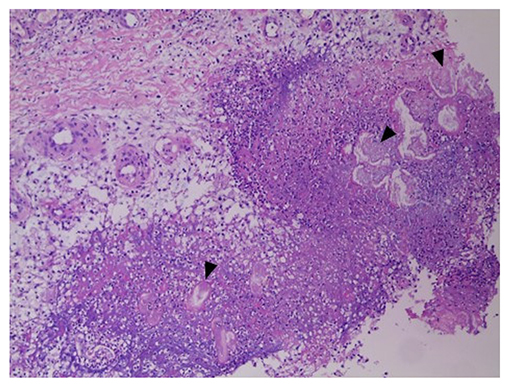
- Pancreatitis, panniculitis, and polyarthritis (PPP) syndrome is a rare but critical disease with a high mortality rate. The diagnostic dilemma of PPP syndrome is the fact that symptoms occur unexpectedly. A 48-year-old man presented with fever and painful swelling of the left foot that was initially mistaken for cellulitis and gouty arthritis. The diagnosis of PPP syndrome was made based on the abdominal CT findings and elevated pancreatic enzyme levels, lobular panniculitis with ghost cells on a skin biopsy, and polyarthritis on a bone scan. The pancreatitis and panniculitis disappeared spontaneously over time, but the polyarthritis followed its own course despite the use of anti-inflammatory agents. In addition to this case, 30 cases of PPP syndrome in the English literature were reviewed. Most of the patients had initial symptoms other than abdominal pain, leading to misdiagnosis. About one-third of them were finally diagnosed with a pancreatic tumor, of which pancreatic acinar cell carcinoma was the most dominant. They showed a mortality rate of 32.3%, associated mainly with the pancreatic malignancy. Therefore, PPP syndrome should be considered when cutaneous or osteoarticular manifestations occur in patients with pancreatitis. Active investigation and continued observations are needed for patients suspected of PPP syndrome.
Keyword
MeSH Terms
Figure
Reference
-
1. Chiari H. Über die sogenannte fettnekrose. Prager Med Wochenschr. 1883; 8:284–286.2. Requena L, Sánchez Yus E. Panniculitis. Part II. Mostly lobular panniculitis. J Am Acad Dermatol. 2001; 45:325–364.
Article3. Narváez J, Bianchi MM, Santo P, et al. Pancreatitis, panniculitis, and polyarthritis. Semin Arthritis Rheum. 2010; 39:417–423.
Article4. Agarwal S, Sasi A, Ray A, Jadon RS, Vikram N. Pancreatitis panniculitis polyarthritis syndrome with multiple bone infarcts. QJM. 2019; 112:43–44.
Article5. Chattopadhyay A, Mittal S, Sharma A, Jain S. Pancreatitis, panniculitis, and polyarthritis. J Clin Rheumatol. 2018; 09. 27. [Epub ahead of print].
Article6. Fordham T, Sims HM, Farrant T. Unusual presentation of pancreatitis with extrapancreatic manifestations. BMJ Case Rep. 2018; 2018:bcr-2018-226440.
Article7. Sondhi AR, Wamsteker EJ, Piper MS. “Doc, I can't walk”-a classic presentation of a rare disease. Gastroenterology. 2018; 155:1703–1705.
Article8. Fernández-Sartorio C, Combalia A, Ferrando J, et al. Pancreatic panniculitis: a case series from a tertiary university hospital in Spain. Australas J Dermatol. 2018; 59:e269–e272.
Article9. Graham PM, Altman DA, Gildenberg SR. Panniculitis, pancreatitis, and polyarthritis: a rare clinical syndrome. Cutis. 2018; 101:E34–E37.10. Zundler S, Strobel D, Manger B, Neurath MF, Wildner D. Pancreatic panniculitis and polyarthritis. Curr Rheumatol Rep. 2017; 19:62.
Article11. Dong E, Attam R, Wu BU. Board review vignette: PPP syndrome: pancreatitis, panniculitis, polyarthritis. Am J Gastroenterol. 2017; 112:1215–1216.
Article12. Rao P, Coffman N, Ferreira JP. A diagnostic dilemma in a patient with polyarthritis. Am J Med. 2017; 130:e497–e498.
Article13. Dieker W, Derer J, Henzler T, et al. Pancreatitis, panniculitis and polyarthritis (PPP-) syndrome caused by post-pancreatitis pseudocyst with mesenteric fistula. Diagnosis and successful surgical treatment. Case report and review of literature. Int J Surg Case Rep. 2017; 31:170–175.
Article14. Kang DJ, Lee SJ, Choo HJ, Her M, Yoon HK. Pancreatitis, panniculitis, and polyarthritis (PPP) syndrome: MRI features of intraosseous fat necrosis involving the feet and knees. Skeletal Radiol. 2017; 46:279–285.
Article15. Ferri V, Ielpo B, Duran H, et al. Pancreatic disease, panniculitis, polyarthrtitis syndrome successfully treated with total pancreatectomy: case report and literature review. Int J Surg Case Rep. 2016; 28:223–226.
Article16. Loverdos I, Swan MC, Shekherdimian S, et al. A case of pancreatitis, panniculitis and polyarthritis syndrome: elucidating the pathophysiologic mechanisms of a rare condition. J Pediatr Surg Case Rep. 2015; 3:223–226.
Article17. Langenhan R, Reimers N, Probst A. Osteomyelitis: a rare complication of pancreatitis and PPP-syndrome. Joint Bone Spine. 2016; 83:221–224.
Article18. Naeyaert C, de Clerck F, De Wilde V. Pancreatic panniculitis as a paraneoplastic phenomenon of a pancreatic acinar cell carcinoma. Acta Clin Belg. 2016; 71:448–450.
Article19. Callata-Carhuapoma HR, Pato Cour E, Garcia-Paredes B, et al. Pancreatic acinar cell carcinoma with bilateral ovarian metastases, panniculitis and polyarthritis treated with FOLFIRINOX chemotherapy regimen. A case report and review of the literature. Pancreatology. 2015; 15:440–444.
Article20. Arbeláez-Cortés A, Vanegas-García AL, Restrepo-Escobar M, Correa-Londoño LA, González-Naranjo LA. Polyarthritis and pancreatic panniculitis associated with pancreatic carcinoma: review of the literature. J Clin Rheumatol. 2014; 20:433–436.21. Laureano A, Mestre T, Ricardo L, Rodrigues AM, Cardoso J. Pancreatic panniculitis - a cutaneous manifestation of acute pancreatitis. J Dermatol Case Rep. 2014; 8:35–37.
Article22. Azar L, Chatterjee S, Schils J. Pancreatitis, polyarthritis and panniculitis syndrome. Joint Bone Spine. 2014; 81:184.
Article23. Kashyap S, Shanker V, Kumari S, Rana L. Panniculitis-polyarthritis-pancreatitis syndrome. Indian J Dermatol Venereol Leprol. 2014; 80:352–354.
Article24. Fraisse T, Boutet O, Tron AM, Prieur E. Pancreatitis, panniculitis, polyarthritis syndrome: an unusual cause of destructive polyarthritis. Joint Bone Spine. 2010; 77:617–618.
Article25. Vasdev V, Bhakuni D, Narayanan K, Jain R. Intramedullary fat necrosis, polyarthritis and panniculitis with pancreatic tumor: a case report. Int J Rheum Dis. 2010; 13:e74–e78.
Article26. Porcu A, Tilocca PL, Pilo L, Ruiu F, Dettori G. Pancreatic pseudocyst-inferior vena cava fistula causing caval stenosis, left renal vein thrombosis, subcutaneous fat necrosis, arthritis and dysfibrinogenemia. Ann Ital Chir. 2010; 81:215–220.27. Borowicz J, Morrison M, Hogan D, Miller R. Subcutaneous fat necrosis/ panniculitis and polyarthritis associated with acinar cell carcinoma of the pancreas: a rare presentation of pancreatitis, panniculitis and polyarthritis syndrome. J Drugs Dermatol. 2010; 9:1145–1150.28. Harris MD, Bucobo JC, Buscaglia JM. Pancreatitis, panniculitis, polyarthritis syndrome successfully treated with EUS-guided cyst-gastrostomy. Gastrointest Endosc. 2010; 72:456–458.
Article29. Mustafa KN, Hadidy A, Shoumaf M, Razzuki SA. Polyarthritis with chondronecrosis associated with osteonecrosis, panniculitis and pancreatitis. Rheumatol Int. 2010; 30:1239–1242.
Article30. Jose T, Biju IK, Kumar A, et al. 'Pancreatitis, polyarthritis, panniculitis syndrome' (PPP syndrome) plus prolonged pyrexia--a rare presentation of chronic pancreatitis. Indian J Gastroenterol. 2009; 28:186–188.
Article31. Chee C. Panniculitis in a patient presenting with a pancreatic tumour and polyarthritis: a case report. J Med Case Rep. 2009; 3:7331.
Article32. Kuwatani M, Kawakami H, Yamada Y. Osteonecrosis and panniculitis as life-threatening signs. Clin Gastroenterol Hepatol. 2010; 8:e52–e53.
Article33. Park SM. Recent advances in management of chronic pancreatitis. Korean J Gastroenterol. 2015; 66:144–149.
Article34. Park SM, Lee HS, Kim SY, et al. Clinical characteristics of chronic pancreatitis according to the history of pancreatitis. Korean J Gastroenterol. 2009; 53:239–245.35. Dahl PR, Su WP, Cullimore KC, Dicken CH. Pancreatic panniculitis. J Am Acad Dermatol. 1995; 33:413–417.
Article36. Burns WA, Matthews MJ, Hamosh M, Weide GV, Blum R, Johnson FB. Lipase-secreting acinar cell carcinoma of the pancreas with polyarthropathy. A light and electron microscopic, histochemical, and biochemical study. Cancer. 1974; 33:1002–1009.37. Klimstra DS, Heffess CS, Oertel JE, Rosai J. Acinar cell carcinoma of the pancreas. A clinicopathologic study of 28 cases. Am J Surg Pathol. 1992; 16:815–837.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Gouty Arthritis Involving the Hip Joint Diagnosed Using Ultrasonography
- Polyarthritis and Pancreatic Panniculitis in a Patient with Pancreatic Acinar Cell Carcinoma
- A Case of Sclerosing Panniculitis treated with Stanozolol
- Pancreatitis, Panniculitis, and Polyarthritis Syndrome with a Fatal Course
- Chronic Multiple Gouty Arthritis Diagnosed during Anti-Tuberculosis Treatment of Recurrent Tuberculous Arthritis: A Case Report