Neurointervention.
2019 Sep;14(2):137-141. 10.5469/neuroint.2019.00143.
Endovascular Thrombectomy for Distal Occlusion Using a Semi-Deployed Stentriever: Report of 2 Cases and Technical Note
- Affiliations
-
- 1Department of Neurology, The Third People’s Hospital of Hubei, Wuhan, China.
- 2Department of Medical Imaging, Kaohsiung Medical University Hospital, Kaohsiung, Taiwan.
- 3Division of Neuroradiology, Joint Department of Medical Imaging, Toronto Western Hospital, Toronto, Canada. acotsang@hku.hk
- 4Division of Neurosurgery, Department of Surgery, The University of Hong Kong, Hong Kong.
- KMID: 2458494
- DOI: http://doi.org/10.5469/neuroint.2019.00143
Abstract
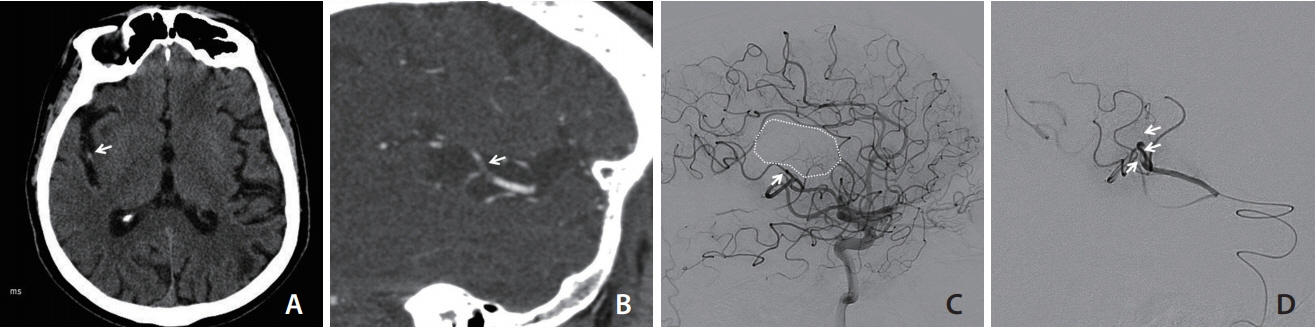
- Distal intracranial occlusions can sometimes cause significant neurological deficits. Endovascular thrombectomy in these vessels may improve outcome but carry a higher risk of haemorrhagic complications due to the small calibre and tortuosity of the target vessel. We report two cases of isolated M2/3 artery occlusion causing dense hemiplegia that was successfully treated with stent retrieval thrombectomy. A "semi-deployment technique" of a 3 mm stentriever was employed at the M2/3 bifurcation of the middle cerebral artery. Partial stent unsheathing allowed adequate clot engagement while avoiding excessive tension by the stent metal struts along the tortuous course of a distal vessel. Complete revascularization was achieved after first-pass of the stent retriever without complication, resulting in good clinical outcome in both cases. The described semi-deployment technique reduces the radial and tractional force exerted by the stentreiver on small branches, and may reduce the risk of vessel laceration or dissection in distal vessel thrombectomy.
Keyword
MeSH Terms
Figure
Reference
-
1. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018; 49:e46. –e110.
Article2. Saber H, Narayanan S, Palla M, Saver JL, Nogueira RG, Yoo AJ, et al. Mechanical thrombectomy for acute ischemic stroke with occlusion of the M2 segment of the middle cerebral artery: a meta-analysis. J Neurointerv Surg. 2018; 10:620–624.
Article3. Tan IY, Demchuk AM, Hopyan J, Zhang L, Gladstone D, Wong K, et al. CT angiography clot burden score and collateral score: correlation with clinical and radiologic outcomes in acute middle cerebral artery infarct. AJNR Am J Neuroradiol. 2009; 30:525–531.
Article4. Fanous AA, Siddiqui AH. Mechanical thrombectomy: stent retrievers vs. aspiration catheters. Cor et Vasa. 2016; 58:e193. –e203.
Article5. Haussen DC, Lima A, Nogueira RG. The Trevo XP 3x20 mm retriever (‘Baby Trevo’) for the treatment of distal intracranial occlusions. J Neurointerv Surg. 2016; 8:295–299.6. Machi P, Jourdan F, Ambard D, Reynaud C, Lobotesis K, Sanchez M, et al. Experimental evaluation of stent retrievers’ mechanical properties and effectiveness. J Neurointerv Surg. 2017; 9:257–263.
Article7. Imahori T, Tanaka K, Koyama J, Arai A, Shiomi R, Iwahashi H, et al. Mechanical thrombectomy using the Trevo ProVue in 50 consecutive patients with anterior circulation stroke: a single-center experience after approval of the stent retriever in Japan. Neurol Med Chir (Tokyo). 2017; 57:128–135.
Article8. Premat K, Bartolini B, Baronnet-Chauvet F, Shotar E, Degos V, Muresan P, et al. Single-center experience using the 3MAX reperfusion catheter for the treatment of acute ischemic stroke with distal arterial occlusions. Clin Neuroradiol. 2018; 28:553–562.
Article9. Kim YW, Son S, Kang DH, Hwang YH, Kim YS. Endovascular thrombectomy for M2 occlusions: comparison between forced arterial suction thrombectomy and stent retriever thrombectomy. J Neurointerv Surg. 2017; 9:626–630.
Article10. Tsang COA, Cheung IHW, Lau KK, Brinjikji W, Kallmes DF, Krings T. Outcomes of stent retriever versus aspiration-first thrombectomy in ischemic stroke: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2018; 39:2070–2076.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- How to Escape Stentriever Wedging in an Open-cell Carotid Stent during Mechanical Thrombectomy for Tandem Cervical Internal Carotid Artery and Middle Cerebral Artery Occlusion
- Suction thrombectomy of distal medium vessel occlusion using microcatheter during mechanical thrombectomy for acute ischemic stroke: A case series
- Pull-Through Buddy Wire Technique for Endovascular Thrombectomy in Patients with Acute Ischemic Stroke: Technical Note
- Novel use of a stent retriever as a distal filler protection device for prevention of secondary embolization
- Direct Brachial Approach for Acute Basilar Artery Occlusion: Technical Note and Preliminary Clinical Experience