Neurointervention.
2020 Mar;15(1):31-36. 10.5469/neuroint.2019.00290.
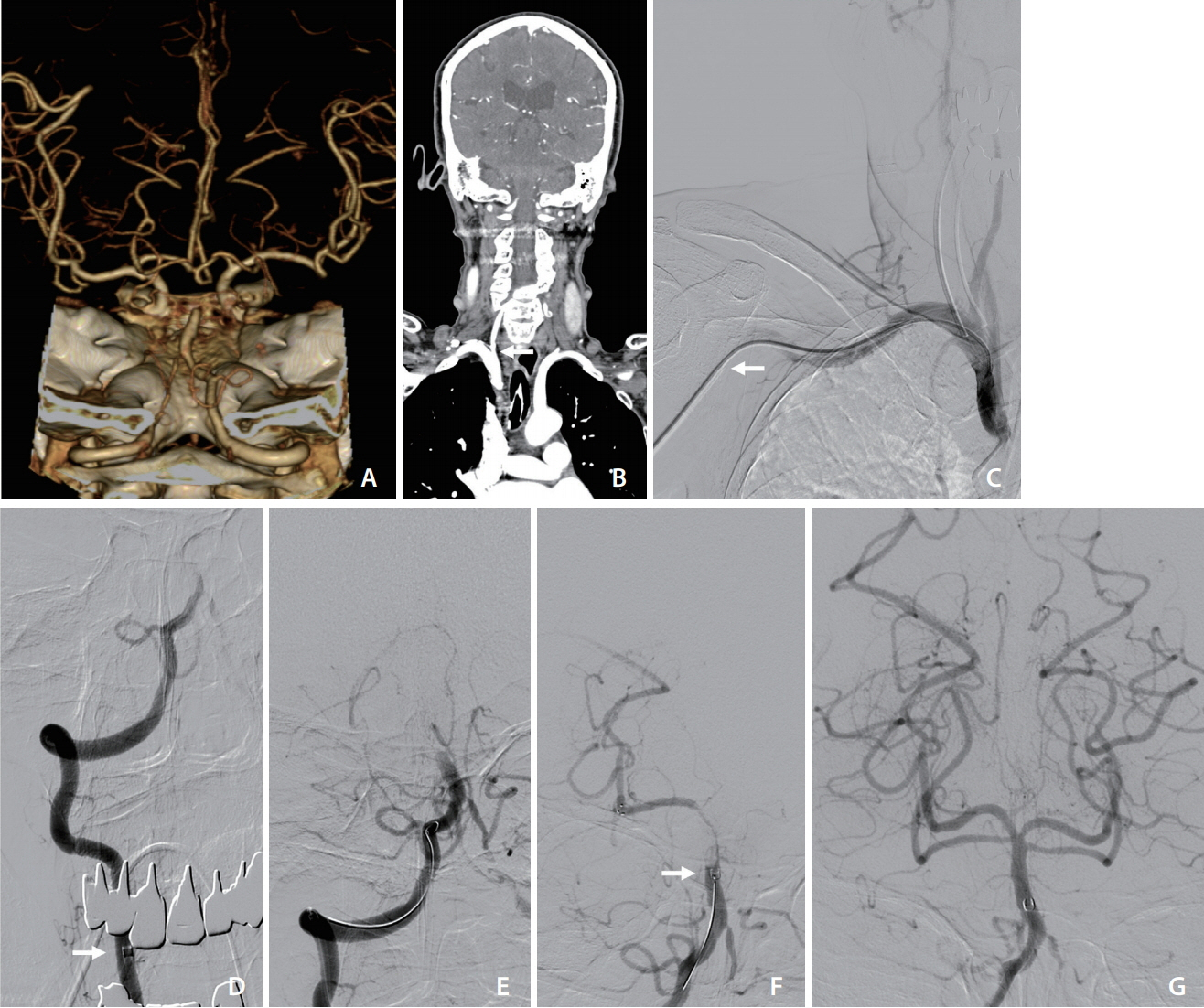
Direct Brachial Approach for Acute Basilar Artery Occlusion: Technical Note and Preliminary Clinical Experience
- Affiliations
-
- 1Department of Neurosurgery, Nagoya City University Graduate School of Medical Sciences, Nagoya, Japan
- 2Department of Neurology, Nagoya City University Graduate School of Medical Sciences, Nagoya, Japan
- KMID: 2502080
- DOI: http://doi.org/10.5469/neuroint.2019.00290
Abstract
- In mechanical endovascular thrombectomy (MET) for acute basilar artery occlusion (ABAO) in the elderly, navigating a guide catheter via the femoral artery may be difficult due to the approach route’s significant tortuosity. To resolve this problem, we have been performing a technique that uses a direct brachial approach (DiBA) with a large-bore aspiration catheter. We reported our preliminary clinical experience with this technique. MET for ABAO using the DiBA technique was performed on 4 consecutive patients between August 2017 and December 2018. In all patients, thrombolysis in cerebral infarction 2B or 3 recanalization was achieved, but the modified Rankin Scale at 90 days was ≥4. There were no technical difficulties or complications with this technique. The DiBA technique is an effective and feasible approach in MET for ABAO. Although excellent clinical outcomes could not be achieved, the angiographic outcomes were excellent with no technical complications. This approach can be an alternative to the femoral artery approach, particularly for tortuous arteries in the elderly.
Figure
Cited by 1 articles
-
Mechanical Thrombectomy for Large Vessel Occlusion via the Transbrachial Approach: Case Series
Yuichiro Tsuji, Takanori Miki, Hiroto Kakita, Kimitoshi Sato, Takashi Yoshida, Fuminori Shimizu
Neurointervention. 2020;15(2):89-95. doi: 10.5469/neuroint.2020.00136.
Reference
-
1. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372:11–20.2. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372:1019–1030.3. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015; 372:1009–1018.
Article4. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015; 372:2285–2295.
Article5. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 372:2296–2306.
Article6. Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA. 2016; 316:1279–1288.
Article7. Giorgianni A, Biraschi F, Piano M, Mardighian D, Gasparotti R, Frigerio M, et al. Endovascular treatment of acute basilar artery occlusion: Registro Endovascolare Lombardo Occlusione basilar artery (RELOBA) study group experience. J Stroke Cerebrovasc Dis. 2018; 27:2367–2374.
Article8. Ribo M, Flores A, Rubiera M, Pagola J, Mendonca N, Rodriguez-Luna D, et al. Difficult catheter access to the occluded vessel during endovascular treatment of acute ischemic stroke is associated with worse clinical outcome. J NeuroInterv Surg. 2013; 5 Supple 1:i70–i73.
Article9. Iwata T, Mori T, Miyazaki Y, Tanno Y, Kasakura S, Aoyagi Y. Anatomical features of the vertebral artery for transbrachial direct cannulation of a guiding catheter to perform coil embolization of cerebral aneurysms in the posterior cerebral circulation. Interv Neuroradiol. 2015; 21:381–386.
Article10. Humphries W, Hoit D, Doss VT, Elijovich L, Frei D, Loy D, et al. Distal aspiration with retrievable stent assisted thrombectomy for the treatment of acute ischemic stroke. J Neurointerv Surg. 2015; 7:90–94.
Article11. McTaggart RA, Ansari SA, Goyal M, Abruzzo TA, Albani B, Arthur AJ, et al. Initial hospital management of patients with emergent large vessel occlusion (ELVO): report of the standards and guidelines committee of the Society of NeuroInterventional Surgery. J Neurointerv Surg. 2017; 9:316–323.
Article12. Kaneko J, Ota T, Tagami T, Unemoto K, Shigeta K, Amano T, et al. Endovascular treatment of acute basilar artery occlusion: Tama-REgistry of Acute Thrombectomy (TREAT) study. J Neurol Sci. 2019; 401:29–33.
Article13. Lee DG, Lee DH, Shim JH, Suh DC. Feasibility of the transradial or the transbrachial approach in various neurointerventional procedures. Neurointervention. 2015; 10:74–81.
Article14. Ishikawa O, Tsutsumi K, Yoshikawa G, Saito A, Tsunoda S, Kondo E, et al. Thrombectomy using a method to directly insert an aspiration catheter into a 6-Fr sheath-introducer placed into the brachial artery. JNET. 2018; 12:456–462.
Article15. Turk AS, Frei D, Fiorella D, Mocco J, Baxter B, Siddiqui A, et al. ADAPT FAST study: a direct aspiration first pass technique for acute stroke thrombectomy. J Neurointerv Surg. 2014; 6:260–264.
Article16. Nguyen TN, Malisch T, Castonguay AC, Gupta R, Sun CH, Martin CO, et al. Balloon guide catheter improves revascularization and clinical outcomes with the Solitaire device: analysis of the North American Solitaire Acute Stroke Registry. Stroke. 2014; 45:141–145.
Article17. Matsubara N, Miyachi S, Okamaoto T, Izumi T, Asai T, Yamanouchi T, et al. Spinal cord infarction is an unusual complication of intracranial neuroendovascular intervention. Interv Neuroradiol. 2013; 19:500–505.
Article18. Agrawal A, Ziccardi MR, Witzke C, Palacios I, Rangaswami J. Cholesterol embolization syndrome: an under-recognized entity in cardiovascular interventions. J Interv Cardiol. 2018; 31:407–415.
Article19. Oomura M, Yamada K, Anan C, Yamada G Hashimoto N, Kamimoto K. Transbrachial carotid artery stenting can prevent renal cholesterol embolism. Intern Med. 2014; 53:1017–1021.
Article20. McTaggart RA, Tung EL, Yaghi S, Cutting SM, Hemendinger M, Gale HI, et al. Continuous aspiration prior to intracranial vascular embolectomy (CAPTIVE): a technique which improves outcomes. J Neurointerv Surg. 2017; 9:1154–1159.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Subtemporal Approach for Basilar Bifurcation and Basilar-Superior Cerebellar Artery Aneurysms
- Upper Basilar Artery Aneurysm Surgery via Transclinoidal Approach
- Subtemporal Transpetrosal Approach for Aneurysms of the Low-Lying Basilar Bifurcation
- Fusiform “True” Posterior Communicating Artery Aneurysm with Basilar Artery Occlusion: A Case Report
- The Use of Protection Device in Landmark-wire Technique of Symptomatic Subclavian Artery Occlusion with Combined Approach via Trans-femoral vs. Trans-brachial Arteries: Technical note