Neurointervention.
2021 Mar;16(1):64-69. 10.5469/neuroint.2020.00409.
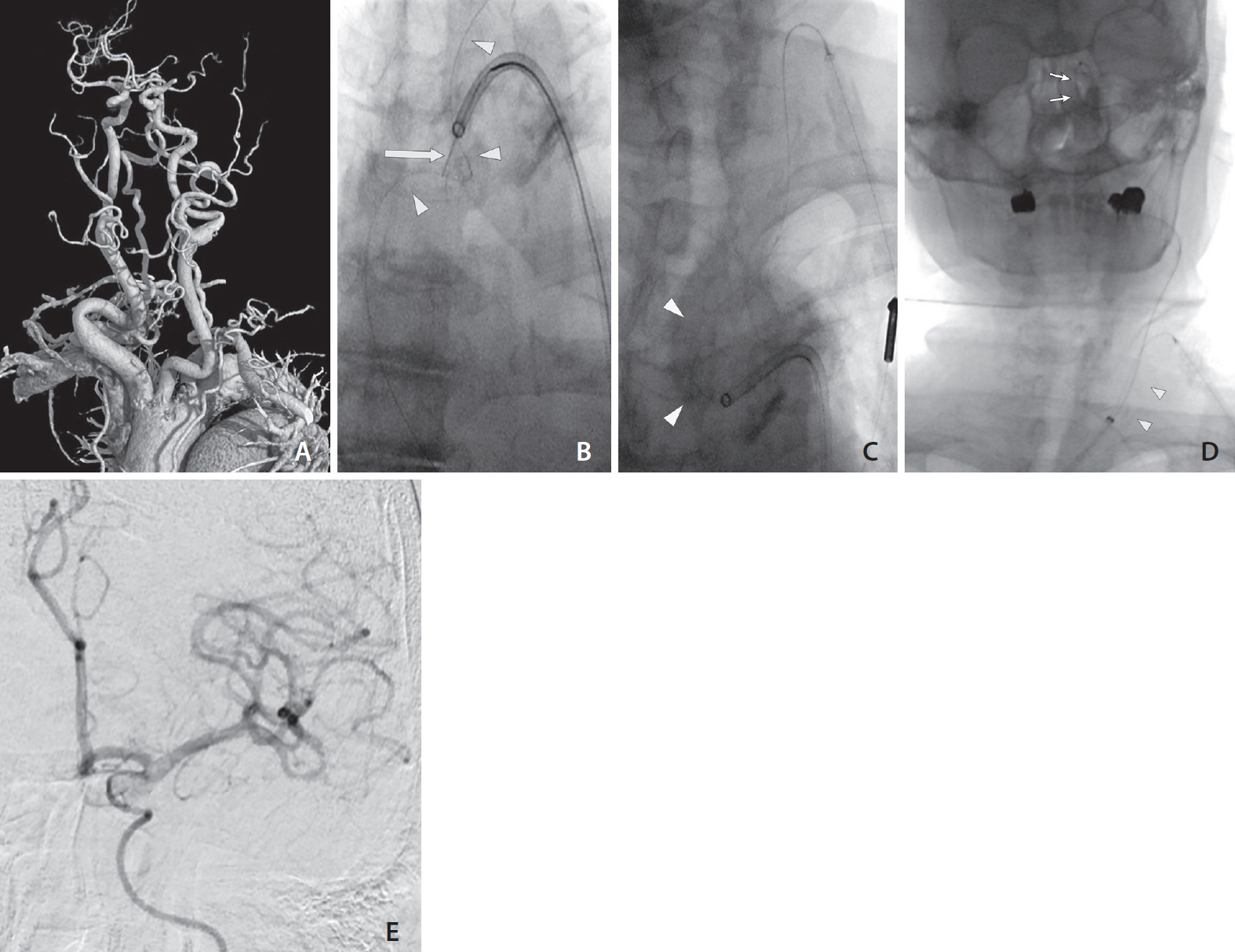
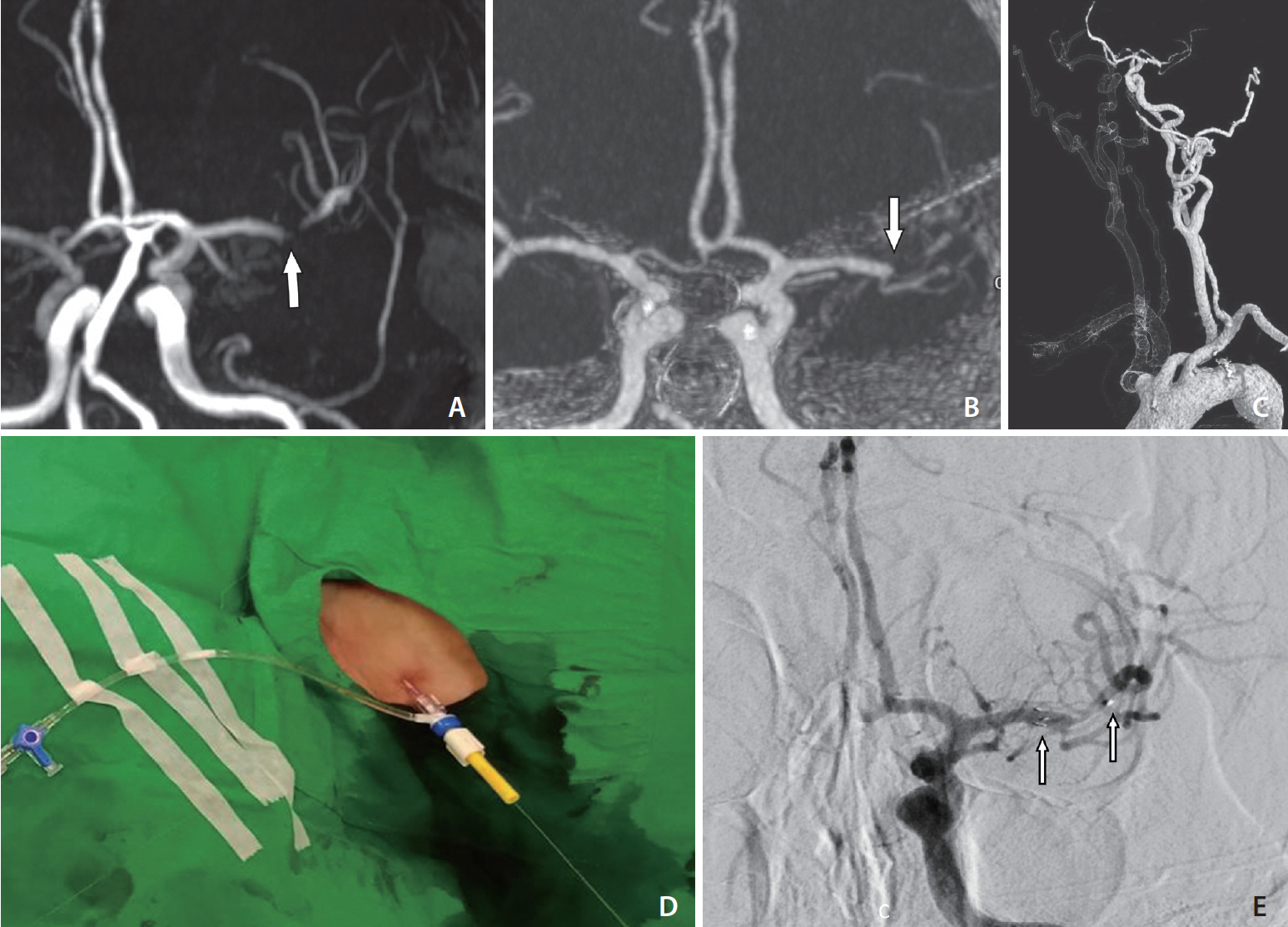
Pull-Through Buddy Wire Technique for Endovascular Thrombectomy in Patients with Acute Ischemic Stroke: Technical Note
- Affiliations
-
- 1Department of Medical Imaging, National Taiwan University Hospital, Taipei, Taiwan
- KMID: 2513346
- DOI: http://doi.org/10.5469/neuroint.2020.00409
Abstract
- Excessive tortuosity is a notable cause of failed endovascular thrombectomy for acute large-vessel occlusion stroke. Transcervical access (TCA) is a commonly proposed solution for overcoming this difficulty. However, the large-bore catheter usually used in TCA increases the risk of serious local complications. This paper presents a modified technique for TCA that uses a pull-through buddy wire (PTBW) to track a large-bore femoral guiding sheath (GS) into the carotid artery via a small carotid puncture site. The carotid puncture site can be easily managed through gentle manual compression. Two illustrative cases using this technique to deal with a large aortic arch and tortuous left common carotid artery are reported. In both cases, recanalization was achieved after successful GS placement. Using a PTBW is feasible in TCA.
Figure
Reference
-
1. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50:e344–e418.
Article2. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, HERMES collaborators, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387:1723–1731.
Article3. Leischner H, Flottmann F, Hanning U, Broocks G, Faizy TD, Deb-Chatterji M, et al. Reasons for failed endovascular recanalization attempts in stroke patients. J Neurointerv Surg. 2019; 11:439–442.
Article4. Ribo M, Flores A, Rubiera M, Pagola J, Mendonca N, Rodriguez-Luna D, et al. Difficult catheter access to the occluded vessel during endovascular treatment of acute ischemic stroke is associated with worse clinical outcome. J Neurointerv Surg. 2013; 5 Suppl 1:i70–i73.
Article5. Styczen H, Behme D, Hesse AC, Psychogios MN. Alternative transcarotid approach for endovascular treatment of acute ischemic stroke patients: a case series. Neurointervention. 2019; 14:131–136.
Article6. Jadhav AP, Ribo M, Grandhi R, Linares G, Aghaebrahim A, Jovin TG, et al. Transcervical access in acute ischemic stroke. J Neurointerv Surg. 2014; 6:652–657.
Article7. Colombo E, Rinaldo L, Lanzino G. Direct carotid puncture in acute ischaemic stroke intervention. Stroke Vasc Neurol. 2020; 5:71–79.
Article8. Wiesmann M, Kalder J, Reich A, Brockmann MA, Othman A, Greiner A, et al. Feasibility of combined surgical and endovascular carotid access for interventional treatment of ischemic stroke. J Neurointerv Surg. 2016; 8:571–575.
Article9. Blanc R, Piotin M, Mounayer C, Spelle L, Moret J. Direct cervical arterial access for intracranial endovascular treatment. Neuroradiology. 2006; 48:925–929.
Article10. Mokin M, Snyder KV, Levy EI, Hopkins LN, Siddiqui AH. Direct carotid artery puncture access for endovascular treatment of acute ischemic stroke: technical aspects, advantages, and limitations. J Neurointerv Surg. 2015; 7:108–113.
Article11. Matsumoto H, Fujita K, Miki J, Tsuji N, Terada T, Itakura T. [Direct carotid approach for carotid angioplasty and stenting with a small incision: a technical case report]. No Shinkei Geka. 2004; 32:735–740. Japanese.12. Nii K, Kazekawa K, Onizuka M, Aikawa H, Tsutsumi M, Tomokiyo M, et al. Direct carotid puncture for the endovascular treatment of anterior circulation aneurysms. AJNR Am J Neuroradiol. 2006; 27:1502–1504.13. Vidale S, Longoni M, Valvassori L, Agostoni E. Mechanical thrombectomy in strokes with large-vessel occlusion beyond 6 hours: a pooled analysis of randomized trials. J Clin Neurol. 2018; 14:407–412.
Article14. Sfyroeras GS, Moulakakis KG, Markatis F, Antonopoulos CN, Antoniou GA, Kakisis JD, et al. Results of carotid artery stenting with transcervical access. J Vasc Surg. 2013; 58:1402–1407.
Article15. Gandhi CD, Al Mufti F, Singh IP, Abruzzo CD, Albani B, Ansari SA, Standards and Guidelines committee of the Society of NeuroInterventional Surgery (SNIS), et al. Neuroendovascular management of emergent large vessel occlusion: update on the technical aspects and standards of practice by the Standards and Guidelines Committee of the Society of NeuroInterventional Surgery. J Neurointerv Surg. 2018; 10:315–320.
Article16. Fjetland L, Roy S. Transcarotid endovascular thrombectomy for acute ischemic stroke. J Vasc Interv Radiol. 2018; 29:1006–1010.
Article17. Dorfer C, Standhardt H, Gruber A, Ferraz-Leite H, Knosp E, Bavinzski G. Direct percutaneous puncture approach versus surgical cutdown technique for intracranial neuroendovascular procedures: technical aspects. World Neurosurg. 2012; 77:192–200.
Article18. Loose HW, Ryall CJ. Common iliac artery occlusion: treatment with pull-through angioplasty. Radiology. 1988; 168:273–274.
Article19. Mitsuhashi Y, Nishio A, Kawakami T, Shibamoto K, Yamagata T, Ichinose T, et al. New pull-through technique using the superficial temporal artery for transbrachial carotid artery stenting. Neurol Med Chir (Tokyo). 2009; 49:320–324.20. He Q, Yu B, Shi W, Tan J, Zhu L, Liang K. Pull-through technique combined with percutaneous angioplasty for treating high-grade arteriovenous fistula stenosis. J Vasc Access. 2020; 21:223–229.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ethic Statement Correction: Pull-Through Buddy Wire Technique for Endovascular Thrombectomy in Patients with Acute Ischemic Stroke: Technical Note
- Endovascular Treatment of Acute Ischemic Stroke
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom
- Refinement of a Thrombectomy Technique to Treat Acute Ischemic Stroke: Technical Note on Microcatheter Advance during Retrieving Self-Expandable Stent
- Differences in Effectiveness among Devices for Endovascular Thrombectomy in Patients with Acute Ischemic Stroke