Korean Circ J.
2019 Oct;49(10):883-907. 10.4070/kcj.2019.0234.
Reducing Stroke Risk in Atrial Fibrillation: Adherence to Guidelines Has Improved, but Patient Persistence with Anticoagulant Therapy Remains Suboptimal
- Affiliations
-
- 1Heart Research Institute, Charles Perkins Centre, Camperdown, Australia. nicole.lowres@sydney.edu.au
- 2Faculty of Medicine and Health, The University of Sydney, Sydney, Australia.
- 3School of Medicine, The University of Notre Dame, Sydney, Australia.
- 4Department of Cardiology, Concord Hospital, The University of Sydney Concord Clinical School, Concord, Australia.
- KMID: 2457998
- DOI: http://doi.org/10.4070/kcj.2019.0234
Abstract
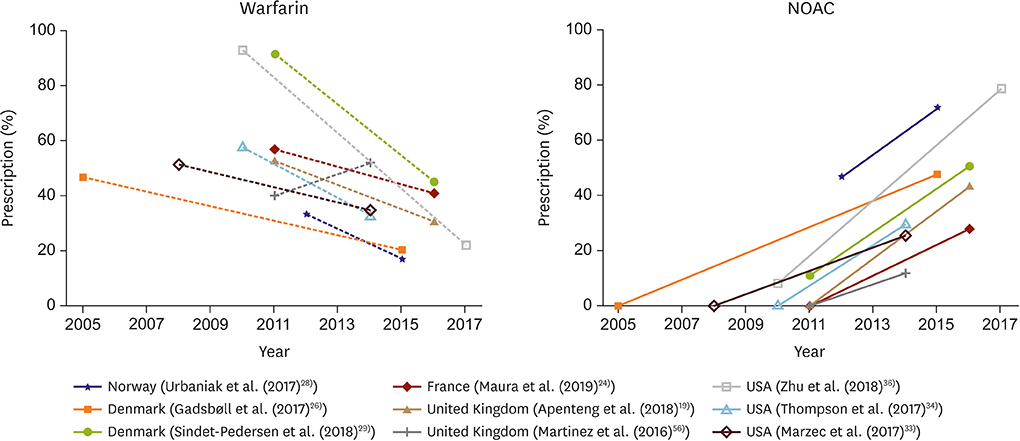
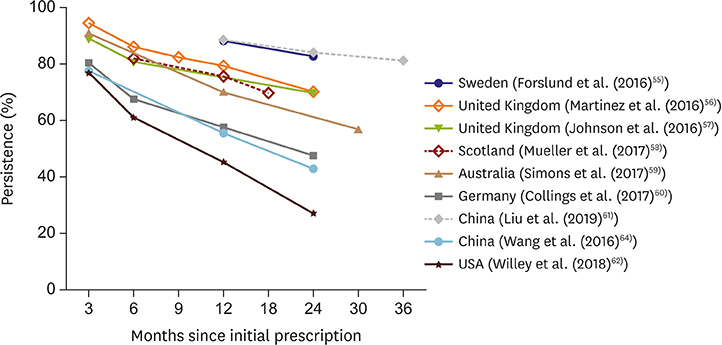
- Atrial fibrillation (AF) is a significant risk factor for avoidable stroke. Among high-risk patients with AF, stroke risk can be mitigated using oral anticoagulants (OACs), however reduction is largely contingent on physician prescription and patient persistence with OAC therapy. Over the past decade significant advances have occurred, with revisions to clinical practice guidelines relating to management of stroke risk in AF in several countries, and the introduction of non-vitamin K antagonist OACs (NOACs). This paper summarises the evolving body of research examining guideline-based clinician prescription over the past decade, and patient-level factors associated with OAC persistence. The review shows clinicians' management over the past decade has increasingly reflected guideline recommendations, with an increasing proportion of high-risk patients receiving OACs, driven by an upswing in NOACs. However, a treatment gap remains, as 25-35% of high-risk patients still do not receive OAC treatment, with great variation between countries. Reduction in stroke risk directly relates to level of OAC prescription and therapy persistence. Persistence and adherence to OAC thromboprophylaxis remains an ongoing issue, with 2-year persistence as low as 50%, again with wide variation between countries and practice settings. Multiple patient-level factors contribute to poor persistence, in addition to concerns about bleeding. Considered review of individual patient's factors and circumstances will assist clinicians to implement appropriate strategies to address poor persistence. This review highlights the interplay of both clinician's awareness of guideline recommendations and understanding of individual patient-level factors which impact adherence and persistence, which are required to reduce the incidence of preventable stroke attributable to AF.
Keyword
MeSH Terms
Figure
Reference
-
1. Miyasaka Y, Barnes ME, Gersh BJ, et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006; 114:119–125.
Article2. Schnabel RB, Yin X, Gona P, et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: a cohort study. Lancet. 2015; 386:154–162.
Article3. Andersson T, Magnuson A, Bryngelsson IL, et al. All-cause mortality in 272,186 patients hospitalized with incident atrial fibrillation 1995–2008: a Swedish nationwide long-term case-control study. Eur Heart J. 2013; 34:1061–1067.4. Healey JS, Oldgren J, Ezekowitz M, et al. Occurrence of death and stroke in patients in 47 countries 1 year after presenting with atrial fibrillation: a cohort study. Lancet. 2016; 388:1161–1169.
Article5. Madhavan M, Hu TY, Gersh BJ, et al. Efficacy of warfarin anticoagulation and incident dementia in a community-based cohort of atrial fibrillation. Mayo Clin Proc. 2018; 93:145–154.
Article6. Healey JS, Connolly SJ, Gold MR, et al. Subclinical atrial fibrillation and the risk of stroke. N Engl J Med. 2012; 366:120–129.
Article7. Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007; 146:857–867.
Article8. Leung LY, McAllister M, Selim M, Fisher M. Factors influencing oral anticoagulant prescribing practices for atrial fibrillation. J Stroke. 2017; 19:232–235.
Article9. NHFA CSANZ Atrial Fibrillation Guideline Working Group. Brieger D, Amerena J, et al. National heart foundation of Australia and the cardiac society of Australia and New Zealand: Australian clinical guidelines for the diagnosis and management of atrial fibrillation 2018. Heart Lung Circ. 2018; 27:1209–1266.
Article10. Kjerpeseth LJ, Ellekjær H, Selmer R, Ariansen I, Furu K, Skovlund E. Risk factors for stroke and choice of oral anticoagulant in atrial fibrillation. Eur J Clin Pharmacol. 2018; 74:1653–1662.
Article11. Gieling EM, van den Ham HA, van Onzenoort H, et al. Risk of major bleeding and stroke associated with the use of vitamin K antagonists, nonvitamin K antagonist oral anticoagulants and aspirin in patients with atrial fibrillation: a cohort study. Br J Clin Pharmacol. 2017; 83:1844–1859.
Article12. Ben Freedman S, Gersh BJ, Lip GY. Misperceptions of aspirin efficacy and safety may perpetuate anticoagulant underutilization in atrial fibrillation. Eur Heart J. 2015; 36:653–656.
Article13. Joung B, Lee JM, Lee KH, et al. 2018 Korean guideline of atrial fibrillation management. Korean Circ J. 2018; 48:1033–1080.
Article14. Manav S. Contemporary management of stroke prevention in atrial fibrillation following the European Society of Cardiology guidelines. Eur Cardiol. 2017; 12:38–39.15. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association task force on practice guidelines and the heart rhythm society. J Am Coll Cardiol. 2014; 64:e1–76.16. Lip GY, Banerjee A, Boriani G, et al. Antithrombotic therapy for atrial fibrillation: CHEST guideline and expert panel report. Chest. 2018; 154:1121–1201.17. Steinberg BA, Shrader P, Thomas L, et al. Factors associated with non-vitamin K antagonist oral anticoagulants for stroke prevention in patients with new-onset atrial fibrillation: results from the outcomes registry for better informed treatment of atrial fibrillation II (ORBIT-AF II). Am Heart J. 2017; 189:40–47.
Article18. von Schéele B, Fernandez M, Hogue SL, Kwong WJ. Review of economics and cost-effectiveness analyses of anticoagulant therapy for stroke prevention in atrial fibrillation in the US. Ann Pharmacother. 2013; 47:671–685.
Article19. Apenteng PN, Gao H, Hobbs FR, Fitzmaurice DA. UK GARFIELD-AF Investigators and GARFIELD-AF Steering Committee. Temporal trends in antithrombotic treatment of real-world UK patients with newly diagnosed atrial fibrillation: findings from the GARFIELD-AF registry. BMJ Open. 2018; 8:e018905.
Article20. Camm AJ, Pinto FJ, Hankey GJ, Andreotti F, Hobbs FD. Writing Committee of the Action for Stroke Prevention alliance. Non-vitamin K antagonist oral anticoagulants and atrial fibrillation guidelines in practice: barriers to and strategies for optimal implementation. Europace. 2015; 17:1007–1017.
Article21. Cowan JC, Wu J, Hall M, Orlowski A, West RM, Gale CP. A 10 year study of hospitalized atrial fibrillation-related stroke in England and its association with uptake of oral anticoagulation. Eur Heart J. 2018; 39:2975–2983.
Article22. Protty MB, Hayes J. Dawn of the direct-acting oral anticoagulants: trends in oral anticoagulant prescribing in Wales 2009–2015. J Clin Pharm Ther. 2017; 42:132–134.
Article23. Robson J, Dostal I, Mathur R, et al. Improving anticoagulation in atrial fibrillation: observational study in three primary care trusts. Br J Gen Pract. 2014; 64:e275–81.
Article24. Maura G, Billionnet C, Drouin J, Weill A, Neumann A, Pariente A. Oral anticoagulation therapy use in patients with atrial fibrillation after the introduction of non-vitamin K antagonist oral anticoagulants: findings from the French healthcare databases, 2011–2016. BMJ Open. 2019; 9:e026645.
Article25. Dalgaard F, Ruwald MH, Lindhardt TB, Gislason GH, Torp-Pedersen C, Pallisgaard JL. Patients with atrial fibrillation and permanent pacemaker: temporal changes in patient characteristics and pharmacotherapy. PloS one. 2018; 13:e0195175.
Article26. Gadsbøll K, Staerk L, Fosbøl EL, et al. Increased use of oral anticoagulants in patients with atrial fibrillation: temporal trends from 2005 to 2015 in Denmark. Eur Heart J. 2017; 38:899–906.
Article27. Gülker JE, Kröger K, Kowall B, Dingelstadt M, Stang A. Increasing use of anticoagulants in Germany and its impact on hospitalization for intracranial bleeding. Circ Cardiovasc Qual Outcomes. 2018; 11:e004470.
Article28. Urbaniak AM, Strøm BO, Krontveit R, Svanqvist KH. Prescription patterns of non-vitamin K oral anticoagulants across indications and factors associated with their increased prescribing in atrial fibrillation between 2012–2015: a study from the Norwegian prescription database. Drugs Aging. 2017; 34:635–645.
Article29. Sindet-Pedersen C, Staerk L, Lamberts M, et al. Use of oral anticoagulants in combination with antiplatelet(s) in atrial fibrillation. Heart. 2018; 104:912–920.
Article30. Haastrup SB, Hellfritzsch M, Rasmussen L, Pottegård A, Grove EL. Use of non-vitamin K antagonist oral anticoagulants 2008–2016: a Danish nationwide cohort study. Basic Clin Pharmacol Toxicol. 2018; 123:452–463.
Article31. Pilote L, Eisenberg MJ, Essebag V, et al. Temporal trends in medication use and outcomes in atrial fibrillation. Can J Cardiol. 2013; 29:1241–1248.
Article32. Weitz JI, Semchuk W, Turpie AG, et al. Trends in prescribing oral anticoagulants in Canada, 2008–2014. Clin Ther. 2015; 37:2506–2514.e4.
Article33. Marzec LN, Wang J, Shah ND, et al. Influence of direct oral anticoagulants on rates of oral anticoagulation for atrial fibrillation. J Am Coll Cardiol. 2017; 69:2475–2484.34. Thompson LE, Maddox TM, Lei L, et al. Sex differences in the use of oral anticoagulants for atrial fibrillation: a report from the national cardiovascular data registry (NCDR®) PINNACLE registry. J Am Heart Assoc. 2017; 6:e005801.
Article35. Lubitz SA, Khurshid S, Weng LC, et al. Predictors of oral anticoagulant non-prescription in patients with atrial fibrillation and elevated stroke risk. Am Heart J. 2018; 200:24–31.
Article36. Zhu J, Alexander GC, Nazarian S, Segal JB, Wu AW. Trends and variation in oral anticoagulant choice in patients with atrial fibrillation, 2010–2017. Pharmacotherapy. 2018; 38:907–920.
Article37. Chao TF, Chiang CE, Lin YJ, et al. Evolving changes of the use of oral anticoagulants and outcomes in patients with newly diagnosed atrial fibrillation in Taiwan. Circulation. 2018; 138:1485–1487.
Article38. Lee SR, Choi EK, Han KD, Cha MJ, Oh S, Lip GY. Temporal trends of antithrombotic therapy for stroke prevention in Korean patients with non-valvular atrial fibrillation in the era of non-vitamin K antagonist oral anticoagulants: a nationwide population-based study. PLoS One. 2017; 12:e0189495.
Article39. Guo Y, Wang H, Tian Y, Wang Y, Lip GY. Time trends of aspirin and warfarin use on stroke and bleeding events in Chinese patients with new-onset atrial fibrillation. Chest. 2015; 148:62–72.
Article40. Verheugt FW, Gao H, Al Mahmeed W, et al. Characteristics of patients with atrial fibrillation prescribed antiplatelet monotherapy compared with those on anticoagulants: insights from the GARFIELD-AF registry. Eur Heart J. 2018; 39:464–473.
Article41. Haas S, Camm AJ, Bassand JP, et al. Predictors of NOAC versus VKA use for stroke prevention in patients with newly diagnosed atrial fibrillation: results from GARFIELD-AF. Am Heart J. 2019; 213:35–46.
Article42. Bastida C, Corominas N, Sotoca JM, Rovira M. Anticoagulation in atrial fibrillation: NOAC prescribing in primary health care. Int J Clin Pharm. 2017; 39:478–482.
Article43. Ha JT, Neuen BL, Cheng LP, et al. Benefits and harms of oral anticoagulant therapy in chronic kidney disease: a systematic review and meta-analysis. Ann Intern Med. 2019.44. Freedman B. Major progress in anticoagulant uptake for atrial fibrillation at last: does it translate into stroke prevention? Eur Heart J. 2018; 39:2984–2986.
Article45. Pollack CV Jr, Reilly PA, van Ryn J, et al. Idarucizumab for dabigatran reversal - full cohort analysis. N Engl J Med. 2017; 377:431–441.
Article46. Connolly SJ, Crowther M, Eikelboom JW, et al. Full study report of andexanet alfa for bleeding associated with factor Xa inhibitors. N Engl J Med. 2019; 380:1326–1335.47. Soo Y, Chan N, Leung KT, et al. Age-specific trends of atrial fibrillation-related ischaemic stroke and transient ischaemic attack, anticoagulant use and risk factor profile in Chinese population: a 15-year study. J Neurol Neurosurg Psychiatry. 2017; 88:744–748.
Article48. Cramer JA, Roy A, Burrell A, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008; 11:44–47.
Article49. Freedman SB, Martinez C, Wallenhorst C, Katholing A. High burden of potentially avoidable stroke from discontinuation of warfarin therapy in non-valvular atrial fibrillation. Eur Heart J. 2015; 36:862.50. Hurtado-Navarro I, García-Sempere A, Rodríguez-Bernal C, Santa-Ana-Tellez Y, Peiró S, Sanfélix-Gimeno G. Estimating adherence based on prescription or dispensation information: impact on thresholds and outcomes. a real-world study with atrial fibrillation patients treated with oral anticoagulants in Spain. Front Pharmacol. 2018; 9:1353.
Article51. Deshpande CG, Kogut S, Laforge R, Willey C. Impact of medication adherence on risk of ischemic stroke, major bleeding and deep vein thrombosis in atrial fibrillation patients using novel oral anticoagulants. Curr Med Res Opin. 2018; 34:1285–1292.
Article52. Borne RT, O'Donnell C, Turakhia MP, et al. Adherence and outcomes to direct oral anticoagulants among patients with atrial fibrillation: findings from the veterans health administration. BMC Cardiovasc Disord. 2017; 17:236.
Article53. Shore S, Carey EP, Turakhia MP, et al. Adherence to dabigatran therapy and longitudinal patient outcomes: insights from the veterans health administration. Am Heart J. 2014; 167:810–817.
Article54. Alberts MJ, Peacock WF, Fields LE, et al. Association between once- and twice-daily direct oral anticoagulant adherence in nonvalvular atrial fibrillation patients and rates of ischemic stroke. Int J Cardiol. 2016; 215:11–13.
Article55. Forslund T, Wettermark B, Hjemdahl P. Comparison of treatment persistence with different oral anticoagulants in patients with atrial fibrillation. Eur J Clin Pharmacol. 2016; 72:329–338.
Article56. Martinez C, Katholing A, Wallenhorst C, Freedman SB. Therapy persistence in newly diagnosed non-valvular atrial fibrillation treated with warfarin or NOAC. A cohort study. Thromb Haemost. 2016; 115:31–39.57. Johnson ME, Lefèvre C, Collings SL, et al. Early real-world evidence of persistence on oral anticoagulants for stroke prevention in non-valvular atrial fibrillation: a cohort study in UK primary care. BMJ Open. 2016; 6:e011471.
Article58. Mueller T, Alvarez-Madrazo S, Robertson C, Bennie M. Use of direct oral anticoagulants in patients with atrial fibrillation in Scotland: applying a coherent framework to drug utilisation studies. Pharmacoepidemiol Drug Saf. 2017; 26:1378–1386.
Article59. Simons LA, Ortiz M, Freedman B, Waterhouse BJ, Colquhoun D. Medium- to long-term persistence with non-vitamin-K oral anticoagulants in patients with atrial fibrillation: Australian experience. Curr Med Res Opin. 2017; 33:1337–1341.
Article60. Collings SL, Lefèvre C, Johnson ME, et al. Oral anticoagulant persistence in patients with non-valvular atrial fibrillation: a cohort study using primary care data in Germany. PloS one. 2017; 12:e0185642.
Article61. Liu C, Du X, Jiang C, et al. Long-term persistence with newly-initiated warfarin or non-VKA oral anticoagulant (NOAC) in patients with non-valvular atrial fibrillation: insights from the prospective China-AF registry. Med Sci Monit. 2019; 25:2649–2657.
Article62. Willey V, Franchino-Elder J, Fu AC, et al. Treatment and persistence with oral anticoagulants among newly diagnosed patients with non-valvular atrial fibrillation: a retrospective observational study in a US commercially insured and Medicare advantage population. BMJ Open. 2018; 8:e020676.
Article63. Deitelzweig SB, Buysman E, Pinsky B, et al. Warfarin use and stroke risk among patients with nonvalvular atrial fibrillation in a large managed care population. Clin Ther. 2013; 35:1201–1210.
Article64. Wang ZZ, Du X, Wang W, et al. Long-term persistence of newly initiated warfarin therapy in Chinese patients with nonvalvular atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2016; 9:380–387.
Article65. Han S, Jeong HS, Kim H, Suh HS. The treatment pattern and adherence to direct oral anticoagulants in patients with atrial fibrillation aged over 65. PLoS One. 2019; 14:e0214666.
Article66. Beyer-Westendorf J, Ehlken B, Evers T. Real-world persistence and adherence to oral anticoagulation for stroke risk reduction in patients with atrial fibrillation. Europace. 2016; 18:1150–1157.
Article67. Hohnloser SH, Basic E, Nabauer M. Changes in oral anticoagulation therapy over one year in 51,000 atrial fibrillation patients at risk for stroke: a practice-derived study. Thromb Haemost. 2019; 119:882–893.
Article68. Björck F, Ek A, Johansson L, Själander A. Warfarin persistence among atrial fibrillation patients - why is treatment ended? Cardiovasc Ther. 2016; 34:468–474.
Article69. Simons LA, Ortiz M, Freedman SB, Waterhouse BJ, Colquhoun D, Thomas G. Improved persistence with non-vitamin-K oral anticoagulants compared with warfarin in patients with atrial fibrillation: recent Australian experience. Curr Med Res Opin. 2016; 32:1857–1861.
Article70. Shiga T, Naganuma M, Nagao T, et al. Persistence of non-vitamin K antagonist oral anticoagulant use in Japanese patients with atrial fibrillation: a single-center observational study. J Arrhythm. 2015; 31:339–344.
Article71. Zalesak M, Siu K, Francis K, et al. Higher persistence in newly diagnosed nonvalvular atrial fibrillation patients treated with dabigatran versus warfarin. Circ Cardiovasc Qual Outcomes. 2013; 6:567–574.
Article72. Brown JD, Shewale AR, Talbert JC. Adherence to rivaroxaban, dabigatran, and apixaban for stroke prevention for newly diagnosed and treatment-naive atrial fibrillation patients: an update using 2013–2014 data. J Manag Care Spec Pharm. 2017; 23:958–967.
Article73. Engdahl J, Holmén A, Rosenqvist M, Strömberg U. A prospective 5-year follow-up after population-based systematic screening for atrial fibrillation. Europace. 2018; 20:f306–11.
Article74. Fischer MA, Stedman MR, Lii J, et al. Primary medication non-adherence: analysis of 195,930 electronic prescriptions. J Gen Intern Med. 2010; 25:284–290.
Article75. Stephenson JJ, Shinde MU, Kwong WJ, Fu AC, Tan H, Weintraub WS. Comparison of claims vs patient-reported adherence measures and associated outcomes among patients with nonvalvular atrial fibrillation using oral anticoagulant therapy. Patient Prefer Adherence. 2018; 12:105–117.
Article76. Blaschke TF, Osterberg L, Vrijens B, Urquhart J. Adherence to medications: insights arising from studies on the unreliable link between prescribed and actual drug dosing histories. Annu Rev Pharmacol Toxicol. 2012; 52:275–301.
Article77. Obamiro KO, Chalmers L, Lee K, Bereznicki BJ, Bereznicki LR. Adherence to oral anticoagulants in atrial fibrillation: an Australian survey. J Cardiovasc Pharmacol Ther. 2018; 23:337–343.
Article78. Gallagher AM, Rietbrock S, Plumb J, van Staa TP. Initiation and persistence of warfarin or aspirin in patients with chronic atrial fibrillation in general practice: do the appropriate patients receive stroke prophylaxis? J Thromb Haemost. 2008; 6:1500–1506.
Article79. Fang MC, Go AS, Chang Y, et al. Warfarin discontinuation after starting warfarin for atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2010; 3:624–631.
Article80. Gomes T, Mamdani MM, Holbrook AM, Paterson JM, Juurlink DN. Persistence with therapy among patients treated with warfarin for atrial fibrillation. Arch Intern Med. 2012; 172:1687–1689.
Article81. Chatterjee S, Sardar P, Giri JS, Ghosh J, Mukherjee D. Treatment discontinuations with new oral agents for long-term anticoagulation: insights from a meta-analysis of 18 randomized trials including 101,801 patients. Mayo Clin Proc. 2014; 89:896–907.
Article82. Weeda ER, Coleman CI, McHorney CA, Crivera C, Schein JR, Sobieraj DM. Impact of once- or twice-daily dosing frequency on adherence to chronic cardiovascular disease medications: a meta-regression analysis. Int J Cardiol. 2016; 216:104–109.
Article83. Crowley MJ, Zullig LL, Shah BR, et al. Medication non-adherence after myocardial infarction: an exploration of modifying factors. J Gen Intern Med. 2015; 30:83–90.
Article84. Gerber BS, Cho YI, Arozullah AM, Lee SY. Racial differences in medication adherence: a cross-sectional study of Medicare enrollees. Am J Geriatr Pharmacother. 2010; 8:136–145.
Article85. McKenzie SJ, McLaughlin D, Clark J, Doi SA. The burden of non-adherence to cardiovascular medications among the aging population in Australia: a meta-analysis. Drugs Aging. 2015; 32:217–225.
Article86. Suzuki T, Shiga T, Omori H, Tatsumi F, Nishimura K, Hagiwara N. Self-reported non-adherence to medication in Japanese patients with cardiovascular diseases. Am J Cardiovasc Drugs. 2018; 18:311–316.
Article87. Miyazaki M, Nakashima A, Nakamura Y, et al. Association between medication adherence and illness perceptions in atrial fibrillation patients treated with direct oral anticoagulants: an observational cross-sectional pilot study. PLoS One. 2018; 13:e0204814.
Article88. Smet L, Heggermont WA, Goossens E, et al. Adherence, knowledge, and perception about oral anticoagulants in patients with atrial fibrillation at high risk for thromboembolic events after radiofrequency ablation. J Adv Nurs. 2018; 74:2577–2587.
Article89. Pandya EY, Bajorek B. Factors affecting patients' perception on, and adherence to, anticoagulant therapy: anticipating the role of direct oral anticoagulants. Patient. 2017; 10:163–185.
Article90. Fan JH, Lyons SA, Goodman MS, Blanchard MS, Kaphingst KA. Relationship between health literacy and unintentional and intentional medication nonadherence in medically underserved patients with type 2 diabetes. Diabetes Educ. 2016; 42:199–208.
Article91. Abdou JK, Auyeung V, Patel JP, Arya R. Adherence to long-term anticoagulation treatment, what is known and what the future might hold. Br J Haematol. 2016; 174:30–42.
Article92. Rolls CA, Obamiro KO, Chalmers L, Bereznicki LR. The relationship between knowledge, health literacy, and adherence among patients taking oral anticoagulants for stroke thromboprophylaxis in atrial fibrillation. Cardiovasc Ther. 2017; 35:e12304.
Article93. Zhao S, Zhao H, Wang X, et al. Factors influencing medication knowledge and beliefs on warfarin adherence among patients with atrial fibrillation in China. Patient Prefer Adherence. 2017; 11:213–220.
Article94. Wei Y, Xu J, Wu H, et al. Survey of antithrombotic treatment in rural patients (>60 years) with atrial fibrillation in East China. Sci Rep. 2018; 8:6830.
Article95. Wilke T, Bauer S, Mueller S, Kohlmann T, Bauersachs R. Patient preferences for oral anticoagulation therapy in atrial fibrillation: a systematic literature review. Patient. 2017; 10:17–37.
Article96. Clarkesmith DE, Lip GY, Lane DA. Patients' experiences of atrial fibrillation and non-vitamin K antagonist oral anticoagulants (NOACs), and their educational needs: a qualitative study. Thromb Res. 2017; 153:19–27.
Article97. Jin J, Sklar GE, Min Sen Oh V, Chuen Li S. Factors affecting therapeutic compliance: a review from the patient's perspective. Ther Clin Risk Manag. 2008; 4:269–286.98. Vinereanu D, Lopes RD, Bahit MC, et al. A multifaceted intervention to improve treatment with oral anticoagulants in atrial fibrillation (IMPACT-AF): an international, cluster-randomised trial. Lancet. 2017; 390:1737–1746.99. Montalescot G, Brotons C, Cosyns B, et al. Educational impact on apixaban adherence in atrial fibrillation (the AEGEAN STUDY): a randomized clinical trial. Am J Cardiovasc Drugs. 2019.
Article100. Desteghe L, Vijgen J, Koopman P, et al. Telemonitoring-based feedback improves adherence to non-vitamin K antagonist oral anticoagulants intake in patients with atrial fibrillation. Eur Heart J. 2018; 39:1394–1403.
Article101. Di Minno A, Spadarella G, Tufano A, Prisco D, Di Minno G. Ensuring medication adherence with direct oral anticoagulant drugs: lessons from adherence with vitamin K antagonists (VKAs). Thromb Res. 2014; 133:699–704.102. Dupclay L, Eaddy M, Jackson J, Raju A, Shim A. Real-world impact of reminder packaging on antihypertensive treatment adherence and persistence. Patient Prefer Adherence. 2012; 6:499–507.103. Aggarwal B, Liao M, Mosca L. Medication adherence is associated with having a caregiver among cardiac patients. Ann Behav Med. 2013; 46:237–242.
Article104. Hui DS, Morley JE, Mikolajczak PC, Lee R. Atrial fibrillation: a major risk factor for cognitive decline. Am Heart J. 2015; 169:448–456.
Article105. Stacey D, Légaré F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017; 4:CD001431.
Article106. Thakkar J, Kurup R, Laba TL, et al. Mobile telephone text messaging for medication adherence in chronic disease: a meta-analysis. JAMA Intern Med. 2016; 176:340–349.107. Santo K, Singleton A, Rogers K, et al. Medication reminder applications to improve adherence in coronary heart disease: a randomised clinical trial. Heart. 2018; 105:323–329.
Article108. Ahmed I, Ahmad NS, Ali S, et al. Medication adherence apps: review and content analysis. JMIR mHealth uHealth. 2018; 6:e62.
Article109. Rohan JM, Drotar D, Alderfer M, et al. Electronic monitoring of medication adherence in early maintenance phase treatment for pediatric leukemia and lymphoma: identifying patterns of nonadherence. J Pediatr Psychol. 2015; 40:75–84.
Article110. van Heuckelum M, van den Ende CH, Houterman AE, Heemskerk CP, van Dulmen S, van den Bemt BJ. The effect of electronic monitoring feedback on medication adherence and clinical outcomes: a systematic review. PLoS One. 2017; 12:e0185453.
Article111. Aldeer M, Javanmard M, Martin R. A review of medication adherence monitoring technologies. Appl Syst Innov. 2018; 1:14.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Mechanism of and Preventive Therapy for Stroke in Patients with Atrial Fibrillation
- Antithrombotic Therapy for Patients with Nonvalvular Atrial Fibrillation
- Practical Issues to Prevent Stroke Associated with Non-valvular Atrial Fibrillation
- Stroke Prevention in Atrial Fibrillation: Focus on Asian Patients
- Use of NOAC in Cardioversion