Acute Crit Care.
2019 Aug;34(3):192-201. 10.4266/acc.2018.00374.
The quality of dying and death for patients in intensive care units: a single center pilot study
- Affiliations
-
- 1Department of Burn and Critical Care, Bestian Hospital, Osong, Korea.
- 2Department of Internal Medicine, Daejeon Veterans Hospital, Daejeon, Korea.
- 3Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Chungnam National University Hospital, Daejeon, Korea. jymoon@cnuh.co.kr
- 4Hospital Ethics Committee, Chungnam National University Hospital, Daejeon, Korea.
- 5Department of Internal Medicine, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- KMID: 2457677
- DOI: http://doi.org/10.4266/acc.2018.00374
Abstract
- BACKGROUND
To identify the necessary care for dying patients in intensive care units (ICUs), we designed a retrospective study to evaluate the quality of dying and death (QODD) experienced by the surrogates of patients with medical illness who died in the ICU of a tertiary referral hospital.
METHODS
To achieve our objective, the authors compared the QODD scores as appraised by the relatives of patients who died of cancer under hospice care with those who died in the ICU. For this study, a Korean version of the QODD questionnaire was developed, and individual interviews were also conducted.
RESULTS
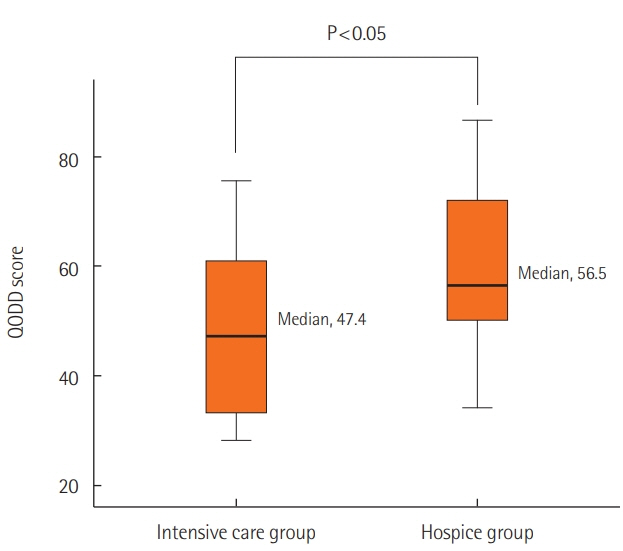
Sixteen people from the intensive care group and 23 people from the hospice care group participated in the survey and completed the questionnaire. The family members of patients who died in the ICU declined participation at a high rate (50%), with the primary reason being to avoid bringing back painful memories (14 people, 87.5%). The relatives of the intensive care group obtained an average total score on the 17-item QODD questionnaire, which was significantly lower than that of the relatives of the hospice group (48.7±15.5 vs. 60.3±14.8, P=0.03).
CONCLUSIONS
This work implies that there are unmet needs for the care of dying patients and for the QODD in tertiary hospital ICUs. This result suggests that shared decision making for advance care planning should be encouraged and that education on caring for dying patients should be provided to healthcare professionals to improve the QODD in Korean ICUs.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Recent Trends in the Withdrawal of Life-Sustaining Treatment in Patients with Acute Cerebrovascular Disease : 2017–2021
Seung Hwan Kim, Ji Hwan Jang, Young Zoon Kim, Kyu Hong Kim, Taek Min Nam
J Korean Neurosurg Soc. 2024;67(1):73-83. doi: 10.3340/jkns.2023.0074.
Reference
-
1. Statistics Korea. Report of 2017 birth and death rate. Daejeon: Statistics Korea;2018.2. Truog RD, Campbell ML, Curtis JR, Haas CE, Luce JM, Rubenfeld GD, et al. Recommendations for end-of-life care in the intensive care unit: a consensus statement by the American College [corrected] of Critical Care Medicine. Crit Care Med. 2008; 36:953–63.3. Patrick DL, Engelberg RA, Curtis JR. Evaluating the quality of dying and death. J Pain Symptom Manage. 2001; 22:717–26.
Article4. Curtis JR, Patrick DL, Engelberg RA, Norris K, Asp C, Byock I. A measure of the quality of dying and death; initial validation using after-death interviews with family members. J Pain Symptom Manage. 2002; 24:17–31.5. Heckel M, Bussmann S, Stiel S, Weber M, Ostgathe C. Validation of the German Version of the Quality of Dying and Death Questionnaire for Informal Caregivers (QODD-D-Ang). J Pain Symptom Manage. 2015; 50:402–13.
Article6. Pérez-Cruz PE, Padilla Pérez O, Bonati P, Thomsen Parisi O, Tupper Satt L, Gonzalez Otaiza M, et al. Validation of the Spanish version of the Quality of Dying and Death Questionnaire (QODD-ESP) in a home-based cancer palliative care program and development of the QODD-ESP-12. J Pain Symptom Manage. 2017; 53:1042–9.
Article7. Cho JY, Lee J, Lee SM, Park JH, Kim J, Kim Y, et al. Transcultural adaptation and validation of quality of dying and death questionnaire in medical intensive care units in South Korea. Acute Crit Care. 2018; 33:95–101.
Article8. Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013; 41:263–306.
Article9. National Cancer Center. Cancer pain management guideline. Goyang: National Cancer Center;2015.10. Downey L, Curtis JR, Lafferty WE, Herting JR, Engelberg RA. The Quality of Dying and Death Questionnaire (QODD): empirical domains and theoretical perspectives. J Pain Symptom Manage. 2010; 39:9–22.
Article11. Mularski RA. Defining and measuring quality palliative and end-of-life care in the intensive care unit. Crit Care Med. 2006; 34(11 Suppl):S309–16.
Article12. Center to Advance Palliative Care. About palliative care. New York: Center to Advance Palliative Care;2018.13. Blumenthal D. Part 1: quality of care: what is it? N Engl J Med. 1996; 335:891–4.14. Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, Grambow S, Parker J, et al. Preparing for the end of life: preferences of patients, families, physicians, and other care providers. J Pain Symptom Manage. 2001; 22:727–37.15. Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000; 284:2476–82.
Article16. Singer PA, Martin DK, Kelner M. Quality end-of-life care: patients’ perspectives. JAMA. 1999; 281:163–8.17. Lynn J, Teno JM, Phillips RS, Wu AW, Desbiens N, Harrold J, et al. Perceptions by family members of the dying experience of older and seriously ill patients; SUPPORT investigators. Study to understand prognoses and preferences for outcomes and risks of treatments. Ann Intern Med. 1997; 126:97–106.18. Clarke EB, Curtis JR, Luce JM, Levy M, Danis M, Nelson J, et al. Quality indicators for end-of-life care in the intensive care unit. Crit Care Med. 2003; 31:2255–62.
Article19. American Academy of Hospice and Palliative Medicine; Center to Advance Palliative Care; Hospice and Palliative Nurses Association; Last Acts Partnership; National Hospice and Palliative Care Organization. National Consensus Project for Quality Palliative Care: Clinical Practice Guidelines for quality palliative care, executive summary. J Palliat Med. 2004; 7:611–27.20. Gerritsen RT, Koopmans M, Hofhuis JG, Curtis JR, Jensen HI, Zijlstra JG, et al. Comparing quality of dying and death perceived by family members and nurses for patients dying in US and Dutch ICUs. Chest. 2017; 151:298–307.
Article21. Levy CR, Ely EW, Payne K, Engelberg RA, Patrick DL, Curtis JR. Quality of dying and death in two medical ICUs: perceptions of family and clinicians. Chest. 2005; 127:1775–83.22. Teno JM, Clarridge BR, Casey V, Welch LC, Wetle T, Shield R, et al. Family perspectives on end-of-life care at the last place of care. JAMA. 2004; 291:88–93.
Article23. Kinoshita H, Maeda I, Morita T, Miyashita M, Yamagishi A, Shirahige Y, et al. Place of death and the differences in patient quality of death and dying and caregiver burden. J Clin Oncol. 2015; 33:357–63.
Article24. Phua J, Joynt GM, Nishimura M, Deng Y, Myatra SN, Chan YH, et al. Withholding and withdrawal of life-sustaining treatments in intensive care units in Asia. JAMA Intern Med. 2015; 175:363–71.
Article25. Park SY, Phua J, Nishimura M, Deng Y, Kang Y, Tada K, et al. End-of-life care in ICUs in East Asia: a comparison among China, Korea, and Japan. Crit Care Med. 2018; 46:1114–24.26. Lanken PN, Terry PB, Delisser HM, Fahy BF, Hansen-Flaschen J, Heffner JE, et al. An official American Thoracic Society clinical policy statement: palliative care for patients with respiratory diseases and critical illnesses. Am J Respir Crit Care Med. 2008; 177:912–27.
Article27. Sprung CL, Truog RD, Curtis JR, Joynt GM, Baras M, Michalsen A, et al. Seeking worldwide professional consensus on the principles of end-of-life care for the critically ill: the consensus for Worldwide End-of-Life Practice for Patients in Intensive Care Units (WELPICUS) study. Am J Respir Crit Care Med. 2014; 190:855–66.
Article28. Gerritsen RT, Hofhuis JG, Koopmans M, van der Woude M, Bormans L, Hovingh A, et al. Perception by family members and ICU staff of the quality of dying and death in the ICU: a prospective multicenter study in The Netherlands. Chest. 2013; 143:357–63.29. Piers RD, Azoulay E, Ricou B, Dekeyser Ganz F, Decruyenaere J, Max A, et al. Perceptions of appropriateness of care among European and Israeli intensive care unit nurses and physicians. JAMA. 2011; 306:2694–703.
Article30. Cook D, Rocker G. Dying with dignity in the intensive care unit. N Engl J Med. 2014; 370:2506–14.
Article31. Kon AA, Davidson JE, Morrison W, Danis M, White DB; American College of Critical Care Medicine, et al. Shared decision making in ICUs: an American College of Critical Care Medicine and American Thoracic Society Policy statement. Crit Care Med. 2016; 44:188–201.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Experiences of Critical Care Nurses Caring for Dying Patients
- Influence of Death Perception, Attitude Toward Terminal Care, Mental Health on the Terminal Care Stress of Intensive Care Unit Nurses
- Rehabilitation in Intensive Care Unit
- A Study of Intensive Care Unit Nurses' Understanding of the Meaning of Death, Death Anxiety, Death Concern and Respect for Life
- The Effects of Counseling about Death and Dying on Perceptions, Preparedness, and Anxiety Regarding Death among Family Caregivers Caring for Hospice Patients: A Pilot Study