Ann Dermatol.
2018 Aug;30(4):427-431. 10.5021/ad.2018.30.4.427.
Low But Continuous Occurrence of Microsporum gypseum Infection in the Study on 198 Cases in South Korea from 1979 to 2016
- Affiliations
-
- 1Department of Dermatology, School of Medicine, Kyungpook National University, Kyungpook National University Hospital, Daegu, Korea. weonju@knu.ac.kr
- 2Institue of Medical Mycology, Catholic Skin Clinic, Daegu, Korea.
- KMID: 2457519
- DOI: http://doi.org/10.5021/ad.2018.30.4.427
Abstract
- BACKGROUND
Microsporum gypseum has been isolated from South Korea since 1966. However, the incidence of M. gypseum infection is very low.
OBJECTIVE
The aim of this study is to add massive data on M. gypseum to the literature and to provide useful information on clinical and mycological characteristics of M. gypseum.
METHODS
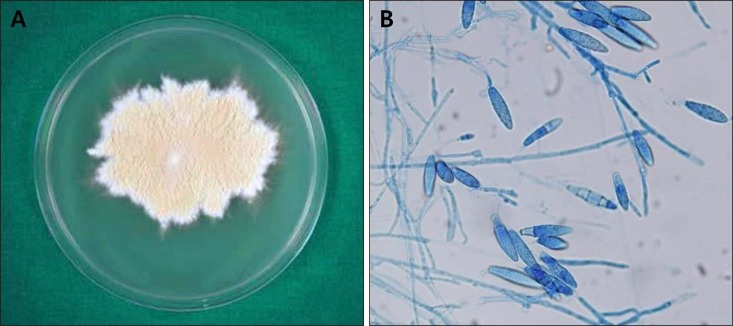
We retrospectively analyzed data of 198 cases infected with M. gypseum from 1979 to 2016. The identification of M. gypseum was done with mycological examination using 15% KOH preparation and potato corn meal tween 80 agar culture media.
RESULTS
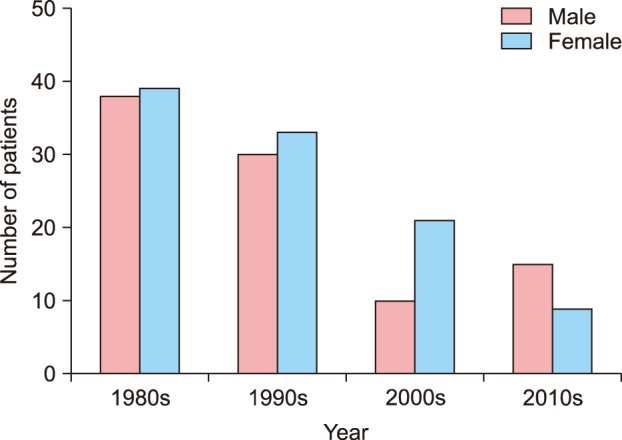
The incidence of M. gypseum infection was very low in South Korea, showing a tendency to decrease. Out of 198 cases, men were 94 cases (47.5%) and women were 104 cases (52.5%). Mean age of all patients was 29.83 years old: 24.97 years old in men and 34.22 years old in women. M. gypseum infection occurred most frequently in September (16.7%) and August (16.2%). The most common clinical type of M. gypseum infection was tinea corporis (38.4%).
CONCLUSION
M. gypseum infection shows very low incidence but still remains around us until recent years. We should keep in mind the characteristics of M. gypseum.
Keyword
MeSH Terms
Figure
Reference
-
1. Lee WJ, Sim HB, Jang YH, Lee SJ, Kim DW, Jun JB, et al. Skin infection due to trichophyton tonsurans still occurs in people in Korea but not as outbreaks. J Korean Med Sci. 2016; 31:296–300. PMID: 26839486.
Article2. Sei Y. [2011 epidemiological survey of dermatomycoses in Japan]. Med Mycol J. 2015; 56:129–135. Japanese.
Article3. Romano C, Massai L, Gallo A, Fimiani M. Microsporum gypseum infection in the Siena area in 2005-2006. Mycoses. 2009; 52:67–71. PMID: 18498297.4. Kim SL, Lee KC, Jang YH, Lee SJ, Kim DW, Lee WJ, et al. The epidemiology of dermatophyte infection in Southeastern Korea (1979~2013). Ann Dermatol. 2016; 28:524–527. PMID: 27489448.
Article5. Zhan P, Liu W. The changing face of dermatophytic infections worldwide. Mycopathologia. 2017; 182:77–86. PMID: 27783316.
Article6. Lee WJ, Kim SL, Jang YH, Lee SJ, Kim DW, Bang YJ, et al. Increasing prevalence of trichophyton rubrum identified through an analysis of 115,846 cases over the last 37 years. J Korean Med Sci. 2015; 30:639–643. PMID: 25931797.
Article7. Seebacher C, Bouchara JP, Mignon B. Updates on the epidemiology of dermatophyte infections. Mycopathologia. 2008; 166:335–352. PMID: 18478365.
Article8. Kim BS, Suh SB. Mycological and clinical observation on dermatophytosis. Korean J Dermatol. 1976; 14:325–334.9. Jun JB, Suh SB. Clinical and mycological studies on microsporum gypseum infection. Korean J Dermatol. 1980; 18:369–381.10. Lee WJ, Park KH, Kim MS, Lee SJ, Kim DW, Bang YJ, et al. Decreasing incidence of trichophyton mentagrophytes in Korea: analysis of 6,250 cases during the last 21-year-period (1992-2012). J Korean Med Sci. 2014; 29:272–276. PMID: 24550657.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical and Mycological Studies on microsporum Gypseum Infection
- A Case of Kerion Celsi Caused by Microsporum gypseum
- A Case of Tinea Corporis Caused by Microsporum gypseum after Scratch Injury by a Dog
- Absence of Reported cases of Microsporum ferrugineum, Trichophyton violaceum, and Trichophyton schoenleinii in South Korea
- A Case of Tinea Capitis Due to Microsporum gypseum