Healthc Inform Res.
2019 Jul;25(3):212-220. 10.4258/hir.2019.25.3.212.
Bayesian Approach to Predicting Acute Appendicitis Using Ultrasonographic and Clinical Variables in Children
- Affiliations
-
- 1Medical Imaging and Nuclear Medicine, Queensland Children's Hospital, South Brisbane, Australia. Tristan.Reddan@health.qld.gov.au
- 2Faculty of Science and Engineering, Queensland University of Technology, Brisbane, Australia.
- 3Hunter Industrial Medicine, Maitland, Australia.
- 4Faculty of Health, Queensland University of Technology, Brisbane, Australia.
- KMID: 2457473
- DOI: http://doi.org/10.4258/hir.2019.25.3.212
Abstract
OBJECTIVES
Ultrasound has an established role in the diagnostic pathway for children with suspected appendicitis. Relevant clinical information can influence the diagnostic probability and reporting of ultrasound findings. A Bayesian network (BN) is a directed acyclic graph (DAG) representing variables as nodes connected by directional arrows permitting visualisation of their relationships. This research developed a BN model with ultrasonographic and clinical variables to predict acute appendicitis in children.
METHODS
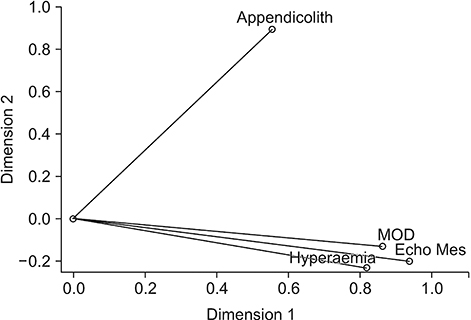
A DAG was designed through a hybrid method based on expert opinion and a review of literature to define the model structure; and the discretisation and weighting of identified variables were calculated using principal components analysis, which also informed the conditional probability table of nodes.
RESULTS
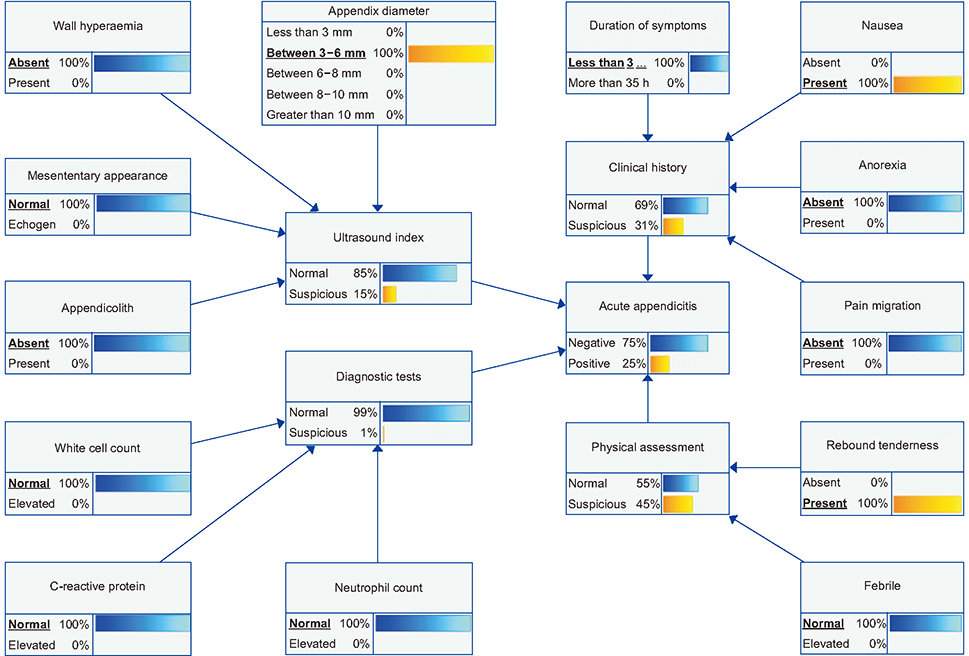
The acute appendicitis target node was designated as an outcome of interest influenced by four sub-models, including Ultrasound Index, Clinical History, Physical Assessment, and Diagnostic Tests. These sub-models included four sonographic, three blood-test, and six clinical variables. The BN was scenario tested and evaluated for face, predictive, and content validity. A lack of similar networks complicated concurrent and convergent validity evaluation.
CONCLUSIONS
To our knowledge, this is the first BN model developed for the identification of acute appendicitis incorporating imaging variables. It has particular benefit for cases in which variables are missing because prior probabilities are built into corresponding nodes. It will be of use to clinicians involved in ultrasound examination of children with suspected appendicitis, as well as their treating clinicians. Prospective evaluation and development of an online tool will permit validation and refinement of the BN.
MeSH Terms
Figure
Reference
-
1. Vom J, Williams I. Justification of radiographic examinations: what are the key issues? J Med Radiat Sci. 2017; 64(3):212–219.
Article2. Mendelson RM, Montgomery BD. Towards appropriate imaging: tips for practice. Aust Fam Physician. 2016; 45(6):391–395.3. Fatahi N, Krupic F, Hellstrom M. Quality of radiologists' communication with other clinicians: as experienced by radiologists. Patient Educ Couns. 2015; 98(6):722–727.
Article4. Pitman AG. Quality of referral: what information should be included in a request for diagnostic imaging when a patient is referred to a clinical radiologist? J Med Imaging Radiat Oncol. 2017; 61(3):299–303.
Article5. Kamel PI, Nagy PG. Patient-centered radiology with FHIR: an introduction to the use of FHIR to offer radiology a clinically integrated platform. J Digit Imaging. 2018; 31(3):327–333.
Article6. Kyburg HE. Reviewed work: Probabilistic Reasoning in Intelligent Systems: Networks of Plausible Inference by Judea Pearl. J Philos. 1991; 88(8):434–447.
Article7. Korb KB, Nicholson AE. Bayesian artificial intelligence. 2nd ed. Boca Raton (FL): CRC Press;2011.8. Bayes T. An essay towards solving a problem in the doctrine of chances. 1763. MD Comput. 1991; 8(3):157–171.9. Benndorf M, Kotter E, Langer M, Herda C, Wu Y, Burnside ES. Development of an online, publicly accessible naive Bayesian decision support tool for mammographic mass lesions based on the American College of Radiology (ACR) BI-RADS lexicon. Eur Radiol. 2015; 25(6):1768–1775.
Article10. Liu YI, Kamaya A, Desser TS, Rubin DL. A Bayesian network for differentiating benign from malignant thyroid nodules using sonographic and demographic features. AJR Am J Roentgenol. 2011; 196(5):W598–W605.
Article11. Thomsen LP, Weinreich UM, Karbing DS, Helbo Jensen VG, Vuust M, Frokjaer JB, et al. Can computed tomography classifications of chronic obstructive pulmonary disease be identified using Bayesian networks and clinical data? Comput Methods Programs Biomed. 2013; 110(3):361–368.
Article12. Sakai S, Kobayashi K, Nakamura J, Toyabe S, Akazawa K. Accuracy in the diagnostic prediction of acute appendicitis based on the Bayesian network model. Methods Inf Med. 2007; 46(6):723–726.
Article13. Reddan T, Corness J, Harden F, Mengersen K. Improving the value of ultrasound in children with suspected appendicitis: a prospective study integrating secondary sonographic signs. Ultrasonography. 2019; 38(1):67–75.
Article14. Pourret O, Naim P, Marcot B. Bayesian networks: a practical guide to applications. Chichester, UK: John Wiley & Sons Ltd.;2008.15. Constantinou AC, Fenton N, Neil M. Integrating expert knowledge with data in Bayesian networks: preserving data-driven expectations when the expert variables remain unobserved. Expert Syst Appl. 2016; 56:197–208.
Article16. Reddan T, Corness J, Mengersen K, Harden F. Sonographic diagnosis of acute appendicitis in children: a 3-year retrospective. Sonography. 2016; 3(3):87–94.
Article17. Reddan T, Corness J, Harden F, Mengersen K. Analysis of the predictive value of clinical and sonographic variables in children with suspected acute appendicitis using decision tree algorithms. Sonography. 2018; 5(4):157–163.
Article18. Salo M, Friman G, Stenstrom P, Ohlsson B, Arnbjornsson E. Appendicitis in children: evaluation of the pediatric appendicitis score in younger and older children. Surg Res Pract. 2014; 2014:438076.19. Samuel M. Pediatric appendicitis score. J Pediatr Surg. 2002; 37(6):877–881.
Article20. Kwan KY, Nager AL. Diagnosing pediatric appendicitis: usefulness of laboratory markers. Am J Emerg Med. 2010; 28(9):1009–1015.
Article21. Salari AA, Binesh F. Diagnostic value of anorexia in acute appendicitis. Pak J Med Sci. 2007; 23(1):68–70.22. Bhatt M, Joseph L, Ducharme FM, Dougherty G, McGillivray D. Prospective validation of the pediatric appendicitis score in a Canadian pediatric emergency department. Acad Emerg Med. 2009; 16(7):591–596.
Article23. Linting M, Meulman JJ, Groenen PJ, van der Koojj AJ. Nonlinear principal components analysis: introduction and application. Psychol Methods. 2007; 12(3):336–358.
Article24. Linting M, van der Kooij A. Nonlinear principal components analysis with CATPCA: a tutorial. J Pers Assess. 2012; 94(1):12–25.
Article25. Mostbeck G, Adam EJ, Nielsen MB, Claudon M, Clevert D, Nicolau C, et al. How to diagnose acute appendicitis: ultrasound first. Insights Imaging. 2016; 7(2):255–263.
Article26. Pitchforth J, Mengersen K. A proposed validation framework for expert elicited Bayesian networks. Expert Syst Appl. 2013; 40(1):162–167.
Article27. Rothrock SG, Pagane J. Acute appendicitis in children: emergency department diagnosis and management. Ann Emerg Med. 2000; 36(1):39–51.
Article28. Reddan T, Corness J, Mengersen K, Harden F. Ultrasound of paediatric appendicitis and its secondary sonographic signs: providing a more meaningful finding. J Med Radiat Sci. 2016; 63(1):59–66.
Article29. Bickell NA, Aufses AH Jr, Rojas M, Bodian C. How time affects the risk of rupture in appendicitis. J Am Coll Surg. 2006; 202(3):401–406.
Article30. Howell EC, Dubina ED, Lee SL. Perforation risk in pediatric appendicitis: assessment and management. Pediatric Health Med Ther. 2018; 9:135–145.
Article31. Reddan T, Corness J, Harden F, Mengersen K. Paediatric appendiceal ultrasound: a survey of Australasian sonographers' opinions on examination performance and sonographic criteria. J Med Radiat Sci. 2018; 65(4):267–274.
Article32. Cundy TP, Gent R, Frauenfelder C, Lukic L, Linke RJ, Goh DW. Benchmarking the value of ultrasound for acute appendicitis in children. J Pediatr Surg. 2016; 51(12):1939–1943.
Article33. Held JM, McEvoy CS, Auten JD, Foster SL, Ricca RL. The non-visualized appendix and secondary signs on ultrasound for pediatric appendicitis in the community hospital setting. Pediatr Surg Int. 2018; 34(12):1287–1292.
Article34. Alter SM, Walsh B, Lenehan PJ, Shih RD. Ultrasound for diagnosis of appendicitis in a community hospital emergency department has a high rate of nondiagnostic studies. J Emerg Med. 2017; 52(6):833–838.
Article