The Korean Organ Transplant Registry (KOTRY): Second Official Adult Heart Transplant Report
- Affiliations
-
- 1Division of Cardiology, Department of Medicine, Heart Vascular Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. choijean5@gmail.com
- 2Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 4Department of Thoracic Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 5Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2456867
- DOI: http://doi.org/10.4070/kcj.2018.0392
Abstract
- BACKGROUND AND OBJECTIVES
This second adult heart transplantation (HTx) report is based on Korean Organ Transplant Registry data submitted on 400 HTxs in recipients of all ages.
METHODS
From March 2014 to December 2017, a total of 400 HTxs were performed at 4 major centers in Korea. We analyzed demographics and characteristics according to transplant years. Patterns of immunosuppression, allograft rejection, and survival after HTx were analyzed. Donor and recipient age were highlighted.
RESULTS
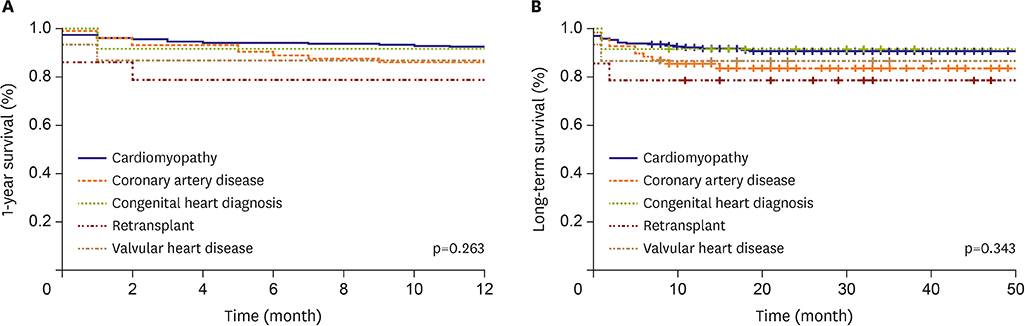
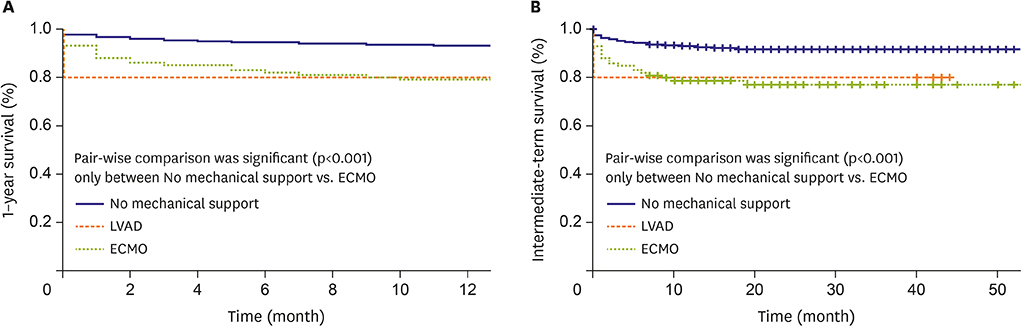
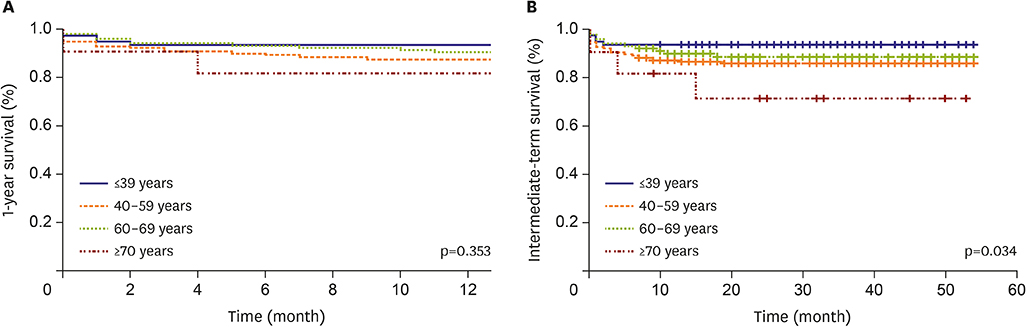
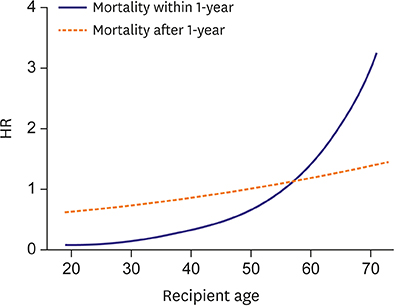
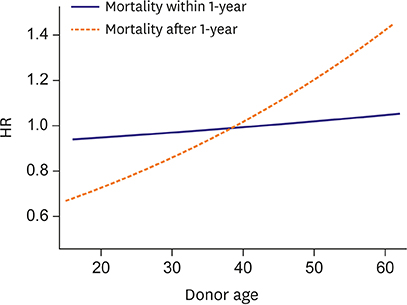
Some distinct differences in HTx statistics were noted. Mean donor age increased significantly in the most recent years compared to 2014-2015, while mean recipient age did not change. The proportion of patients on pre-transplant extracorporeal membrane oxygenation (ECMO) increased over time. One-year and intermediate-term survival was significantly worse in patients on pre-transplant ECMO compared to those without mechanical support. Over the years, tacrolimus has increased to become the most frequently used calcineurin inhibitor over cyclosporine, while the number of patients using steroids both at discharge and 1-year follow-up has declined. Age did not affect 1-year survival, but significantly affected intermediate-term survival.
CONCLUSIONS
From 2014 to 2017, centers were willing to accept older donors to address increasing organ shortages and more patients received transplant under ECMO care. Increasing age was a strong independent factor for intermediate-term survival, however, post-transplant comorbidities did not differ among age groups. Further studies with longer follow-up duration are needed to better understand age-related post-transplant prognosis.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
Increased Risk with Older Donor Age and More Frequent Pre-transplant ECMO: the Second Official KOTRY Report
Jong-Chan Youn, In-Cheol Kim, Nam-Hee Park, Hyungseop Kim
Korean Circ J. 2019;49(8):738-741. doi: 10.4070/kcj.2019.0117.To Take or Not to Take: The Dilemma With Marginal Donor Heart?
Jin Joo Park
Korean Circ J. 2023;53(4):268-270. doi: 10.4070/kcj.2023.0045.Comparison of Veno-arterial Extracorporeal Membrane Oxygenation Configurations for Patients Listed for Heart Transplantation
Jung Ae Hong, Ah-Ram Kim, Min-Ju Kim, Dayoung Pack, Junho Hyun, Sang Eun Lee, Jae-Joong Kim, Pil Je Kang, Sung-Ho Jung, Min-Seok Kim
Korean Circ J. 2023;53(8):535-547. doi: 10.4070/kcj.2022.0348.Korean Society of Heart Failure Guidelines for the Management of Heart Failure: Advanced and Acute Heart Failure
Junho Hyun, Jae Yeong Cho, Jong-Chan Youn, Darae Kim, Dong-Hyuk Cho, Sang Min Park, Mi-Hyang Jung, Hyun-Jai Cho, Seong-Mi Park, Jin-Oh Choi, Wook-Jin Chung, Byung-Su Yoo, Seok-Min Kang,
Korean Circ J. 2023;53(7):452-471. doi: 10.4070/kcj.2023.0115.
Reference
-
1. Kim IC, Youn JC. Understanding the current status of Korean heart transplantation based on initial KOTRY report. Korean Circ J. 2017; 47:858–860.
Article2. Kim IC, Youn JC, Kobashigawa JA. The past, present and future of heart transplantation. Korean Circ J. 2018; 48:565–590.
Article3. Khush KK, Cherikh WS, Chambers DC, et al. The international thoracic organ transplant registry of the International Society for Heart and Lung Transplantation: thirty-fifth adult heart transplantation report-2018; focus theme: multiorgan transplantation. J Heart Lung Transplant. 2018; 37:1155–1168.
Article4. Lee HY, Jeon ES, Kang SM, Kim JJ. Initial report of the Korean Organ Transplant Registry (KOTRY): heart transplantation. Korean Circ J. 2017; 47:868–876.
Article5. Viana LA, Cristelli MP, Santos DW, et al. Influence of epidemiology, immunosuppressive regimens, clinical presentation, and treatment on kidney transplant outcomes of patients diagnosed with tuberculosis: a retrospective cohort analysis. Am J Transplant. 2018.
Article6. Fukuhara S, Takeda K, Kurlansky PA, Naka Y, Takayama H. Extracorporeal membrane oxygenation as a direct bridge to heart transplantation in adults. J Thorac Cardiovasc Surg. 2018; 155:1607–1618.e6.
Article7. Chambers DC, Yusen RD, Cherikh WS, et al. The registry of the International Society for Heart and Lung Transplantation: thirty-fourth adult lung and heart-lung transplantation report-2017; focus theme: allograft ischemic time. J Heart Lung Transplant. 2017; 36:1047–1059.
Article8. Mehra MR, Canter CE, Hannan MM, et al. The 2016 International Society for Heart Lung Transplantation listing criteria for heart transplantation: a 10-year update. J Heart Lung Transplant. 2016; 35:1–23.
Article9. Laks H, Marelli D, Fonarow GC, et al. Use of two recipient lists for adults requiring heart transplantation. J Thorac Cardiovasc Surg. 2003; 125:49–59.
Article10. Blanche C, Blanche DA, Kearney B, et al. Heart transplantation in patients seventy years of age and older: a comparative analysis of outcome. J Thorac Cardiovasc Surg. 2001; 121:532–541.
Article11. Demers P, Moffatt S, Oyer PE, Hunt SA, Reitz BA, Robbins RC. Long-term results of heart transplantation in patients older than 60 years. J Thorac Cardiovasc Surg. 2003; 126:224–231.
Article12. Lund LH, Edwards LB, Kucheryavaya AY, et al. The registry of the International Society for Heart and Lung Transplantation: thirtieth official adult heart transplant report--2013; focus theme: age. J Heart Lung Transplant. 2013; 32:951–964.
Article13. Daneshvar D, Czer LS, Phan A, et al. Heart transplantation in patients aged 70 years and older: a two-decade experience. Transplant Proc. 2011; 43:3851–3856.
Article14. Fulop T, Kotb R, Fortin CF, Pawelec G, de Angelis F, Larbi A. Potential role of immunosenescence in cancer development. Ann N Y Acad Sci. 2010; 1197:158–165.
Article15. Prieto D, Correia P, Batista M, Antunes Mde J. Heart transplantation in patients older than 65 years: worthwhile or wastage of organs? Thorac Cardiovasc Surg. 2015; 63:684–691.
Article16. Prieto D, Correia P, Baptista M, Antunes MJ. Outcome after heart transplantation from older donor age: expanding the donor pool. Eur J Cardiothorac Surg. 2015; 47:672–678.
Article17. Gao HZ, Hunt SA, Alderman EL, Liang D, Yeung AC, Schroeder JS. Relation of donor age and preexisting coronary artery disease on angiography and intracoronary ultrasound to later development of accelerated allograft coronary artery disease. J Am Coll Cardiol. 1997; 29:623–629.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Initial Report of the Korean Organ Transplant Registry (KOTRY): Heart Transplantation
- The Korean Organ Transplantation Registry (KOTRY): an overview and summary of the kidney-transplant cohort
- Pre- and post-transplant risk factors for renal dysfunction in the patients with preserved renal function at 1 month after liver transplantation: a national cohort study using Korean Organ Transplantation Registry (KOTRY)
- ABO blood type does not affect recurrence of hepatocellular carcinoma after liver transplantation: analysis of the Korean Organ Transplantation Registry database
- The first hair transplant assessment scale: parameters for good hair transplantation