Ann Dermatol.
2019 Oct;31(5):559-562. 10.5021/ad.2019.31.5.559.
Syringocystadenocarcinoma Papilliferum: A Case Report and Review of the Literature
- Affiliations
-
- 1Department of Dermatology, College of Medicine, Konyang University, Daejeon, Korea. mabie@hanmail.net
- KMID: 2456234
- DOI: http://doi.org/10.5021/ad.2019.31.5.559
Abstract
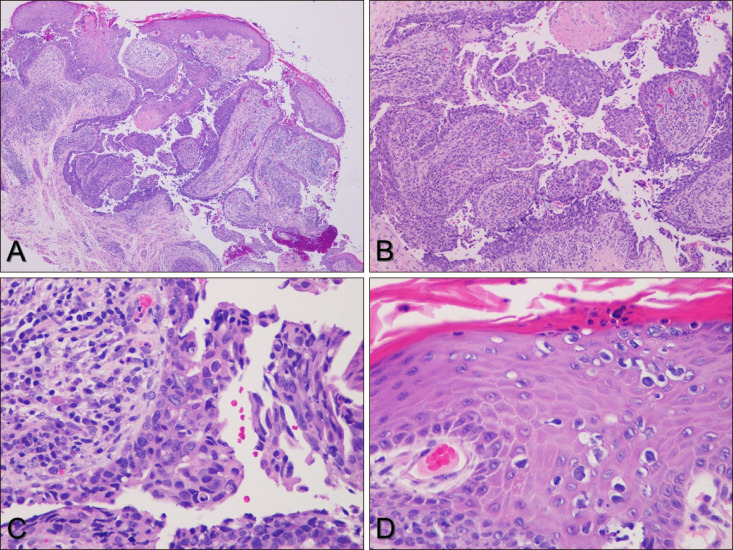
- Syringocystadenocarcinoma papilliferum (SCACP) is a rare malignant adnexal neoplasm, which is considered as a malignant counterpart of syringocystadenoma papilliferum (SCAP). Clinically, SCACP appears as a nodule, inflammatory plaque, or tumor. The lesion is usually covered with crusts, which are formed by secretion of the apocrine epithelial cells. Histologically, SCACP resembles SCAP, with cystic papillomatous invaginations connected to the skin surface by funnel-shaped structures lined by infundibular epithelium. The stroma of the tumor consists of a dense inflammatory infiltrate of plasma cells and lymphocytes. SCACP differs from SCAP in terms of the architectural and cytological features of the tumor cells, and is characterized by higher nuclear cytoplasmic ratio, nuclear irregularity, coarse chromatin, and increased mitotic activity. However, the immunohistochemical findings of SCACP vary. Since only 49 cases of SCACP have been reported in the English literature, the clinical and histologic characteristics of SCACP have not been fully established. Further studies on the diagnostic criteria for SCACP are warranted. Here, we report a rare case of SCACP and present a review of other relevant literature.
Keyword
MeSH Terms
Figure
Reference
-
1. Park SH, Shin YM, Shin DH, Choi JS, Kim KH. Syringocystadenocarcinoma papilliferum: a case report. J Korean Med Sci. 2007; 22:762–765. PMID: 17728526.
Article2. Numata M, Hosoe S, Itoh N, Munakata Y, Hayashi S, Maruyama Y. Syringadenocarcinoma papilliferum. J Cutan Pathol. 1985; 12:3–7. PMID: 2982933.
Article3. Chen J, Beg M, Chen S. Syringocystadenocarcinoma papilliferum in situ, a variant of cutaneous adenocarcinoma in situ: a case report with literature review. Am J Dermatopathol. 2016; 38:762–765. PMID: 27533073.
Article4. Parekh V, Guerrero CE, Knapp CF, Elmets CA, McKay KM. A histological snapshot of hypothetical multistep progression from nevus sebaceus to invasive syringocystadenocarcinoma papilliferum. Am J Dermatopathol. 2016; 38:56–62. PMID: 26317389.
Article5. Leeborg N, Thompson M, Rossmiller S, Gross N, White C, Gatter K. Diagnostic pitfalls in syringocystadenocarcinoma papilliferum: case report and review of the literature. Arch Pathol Lab Med. 2010; 134:1205–1209. PMID: 20670144.
Article6. Ishida-Yamamoto A, Sato K, Wada T, Takahashi H, Iizuka H. Syringocystadenocarcinoma papilliferum: case report and immunohistochemical comparison with its benign counterpart. J Am Acad Dermatol. 2001; 45:755–759. PMID: 11606929.
Article7. Langner C, Ott A. Syringocystadenocarcinoma papilliferum in situ originating from the perianal skin. APMIS. 2009; 117:148–150. PMID: 19239438.
Article8. Iga N, Fujii H, Miyake T, Ehara M, Kore-Eda S. Syringocystadenocarcinoma papilliferum in the perianal area. Case Rep Dermatol. 2015; 7:84–89. PMID: 26078737.
Article9. Hügel H, Requena L. Ductal carcinoma arising from a syringocystadenoma papilliferum in a nevus sebaceus of Jadassohn. Am J Dermatopathol. 2003; 25:490–493. PMID: 14631190.
Article10. Zhang YH, Wang WL, Rapini RP, Torres-Cabala C, Prieto VG, Curry JL. Syringocystadenocarcinoma papilliferum with transition to areas of squamous differentiation: a case report and review of the literature. Am J Dermatopathol. 2012; 34:428–433. PMID: 22343110.11. Mohanty SK, Pradhan D, Diwaker P, Gami A, Hanna IT, Freedman AM, et al. Long-standing exophytic mass in the right infratemporal region. Syringocystadenocarcinoma papilliferum. Int J Dermatol. 2014; 53:539–542. PMID: 24602090.12. Zhang Y, Kong YY, Cai X, Shen XX, Kong JC. Syringocystadenocarcinoma papilliferum: clinicopathologic analysis of 10 cases. J Cutan Pathol. 2017; 44:538–543. PMID: 28337777.
Article13. Rao PB, Ghosh S, Mohapatra M, Philip NP, Kumar PR, Manam S, et al. Chemoradiotherapy in a case of malignant syringocystadenocarcinoma papilliferum of vulva with locoregional failure. Case Rep Oncol Med. 2015; 2015:638294. PMID: 26697249.
Article14. Peterson J, Tefft K, Blackmon J, Rajpara A, Fraga G. Syringocystadenocarcinoma papilliferum: a rare tumor with a favorable prognosis. Dermatol Online J. 2013; 19:19620. PMID: 24050294.
Article15. Bakhshi GD, Wankhede KR, Tayade MB, Shenoy SS, Gore ST, Valand AG. Carcino-sarcoma in a case of syringocystadenoma papilliferum: a rare entity. Clin Pract. 2012; 2:e71. PMID: 24765470.
Article16. Choccalingam C, Samuel PT, Subramaniam D, Hammed F, Purushothaman V, Joshi RS. Syringocystadenocarcinoma papilliferum: a case report of a rare skin adnexal tumor. Our Dermatol Online. 2013; 4:221–223.17. Paradiso B, Bianchini E, Cifelli P, Cavazzini L, Lanza G. A new case of syringocystadenocarcinoma papilliferum: a rare pathology for a wide-ranging comprehension. Case Rep Med. 2014; 2014:453874. PMID: 24959179.
Article18. Satter E, Grady D, Schlocker CT. Syringocystadenocarcinoma papilliferum with locoregional metastases. Dermatol Online J. 2014; 20:22335. PMID: 24746298.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Syringocystadenocarcinoma Papilliferum in Situ Secondary to Scalp Nevus Sebaceus
- Syringocystadenocarcinoma Papilliferum: A Case Report
- A Case of Hidradenoma Papilliferum of the Nipple
- Hidradenoma Papilliferum of the Anus: A Report of 2 Cases and Review of the Literature
- A Case of Ectopic Hidradenoma Papilliferum