J Dent Anesth Pain Med.
2019 Aug;19(4):217-226. 10.17245/jdapm.2019.19.4.217.
Effects site concentrations of propofol using target-controlled infusion in dental treatment under deep sedation among different intellectual disability types
- Affiliations
-
- 1Department of Dental Anesthesiology, Seoul National University, School of Dentistry, Seoul, Korea. stone90@snu.ac.kr
- KMID: 2456013
- DOI: http://doi.org/10.17245/jdapm.2019.19.4.217
Abstract
- BACKGROUND
We aimed to assess the dose needed to achieve the propofol effect-site concentration using target-controlled infusion in intellectually disabled patients and to detail the most effective method for achieving a safe level of consciousness without hemodynamic changes as well as detail any resulting adverse effects.
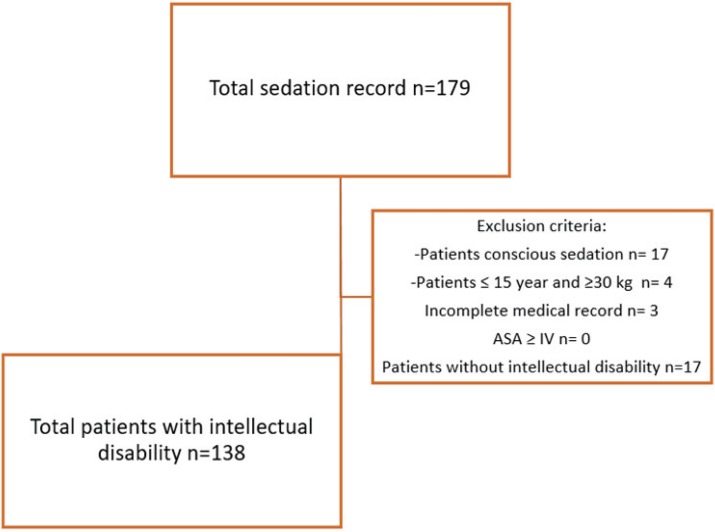
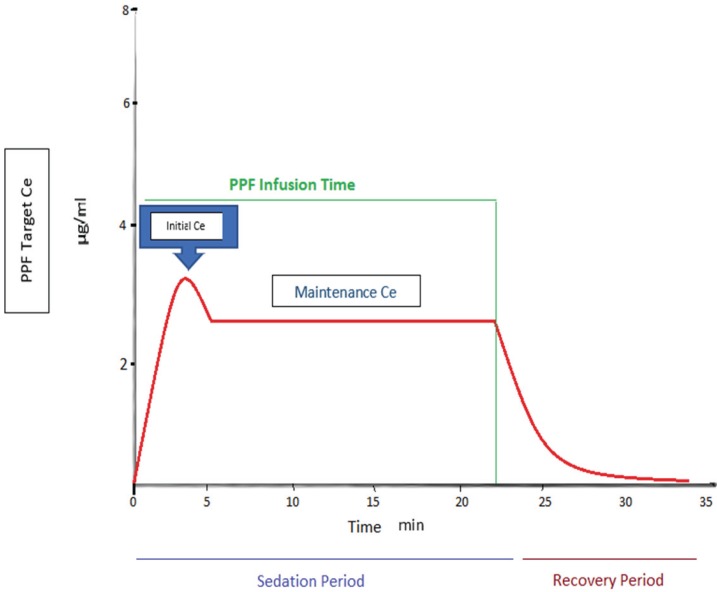
METHODS
We performed a retrospective review of sedation service records of 138 intellectually disabled patients (51, mental retardation; 36, autism; 30, brain lesion, 12 genetic diseases, 9 dementia) aged over 15 years and weighing over 30 kg. These patients had received propofol via target-controlled infusion in the special care dental clinic of Seoul National University Dental Hospital from May 2008 to September 2018 for restorative treatment (112), minor surgery (13), prosthodontics (7), periodontics treatment (5), and implant (1).
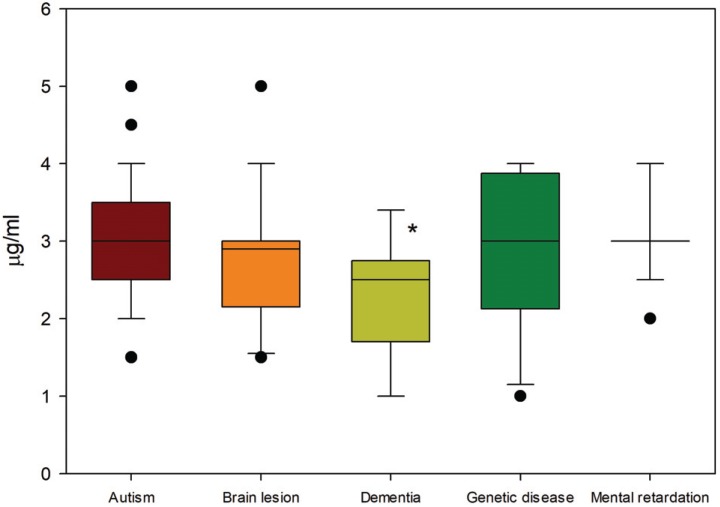
RESULTS
For all groups, the duration of dental treatments was 43 ± 18 minutes, total sedation time was 73 ± 23 minutes, and total BIS values was 57 ± 12. The propofol maintenance dosage values for each group were: mental retardation, 3 ± 0.5 (2-4) µg/ml; autism, 3.1 ± 0.7 (2-5) µg/ml; brain lesion, 2.8 ± 0.7 (1.5-5) µg/ml; genetic disease, 2.9 ± 0.9 (1-4) µg/ml; and dementia 2.3 ± 0.7 (1-3.4) µg/ml.
CONCLUSIONS
The dementia group needed a lower dosage to reach a safe, effective propofol effect-site concentration than the other groups. Since there were no complications, deep sedation is a great alternative to general anesthesia for dental treatment of intellectually disabled patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Altun C, Guven G, Akgun OM, Akkurt MD, Basak F, Akbulut E. Oral health status of disabled individuals attending special schools. Eur J Dent. 2010; 4:361–366. PMID: 20922154.2. Sakaguchi M, Higuchi H, Maeda S, Miyawaki T. Dental sedation for patients with intellectual disability: a prospective study of manual control versus bispectral index-guided target-controlled infusion of propofol. J Clin Anesth. 2011; 23:636–642. PMID: 22137516.
Article3. Caputo AC. Providing deep sedation and general anesthesia for patients with special needs in the dental office-based setting. Spec Care Dentist. 2009; 29:26–30. PMID: 19152565.
Article4. Corcuera-Flores JR, Delgado-Munoz JM, Ruiz-Villandiego JC, Maura-Solivellas I, Machuca-Portillo G. Dental treatment for handicapped patients; sedation vs general anesthesia and update of dental treatment in patients with different diseases. Med Oral Patol Oral Cir Bucal. 2014; 19:e170–e176. PMID: 24121922.
Article5. Chi SI, Kim HJ, Seo KS, Yang M, Chang J. Use of ADMS™ during sedation for dental treatment of an intellectually disabled patient: A case report. J Dent Anesth Pain Med. 2016; 16:217–222. PMID: 28884157.
Article6. Asahi Y, Kubota K, Omichi S. Dose requirements for propofol anaesthesia for dental treatment for autistic patients compared with intellectually impaired patients. Anaesth Intensive Care. 2009; 37:70–73. PMID: 19157349.
Article7. Chidambaran V, Costandi A, D'Mello A. Propofol: A review of its role in pediatric anesthesia and sedation. CNS Drugs. 2015; 29:543–563. PMID: 26290263.
Article8. Lee BS, Shin TJ, Kim HJ, Choi YJ, Lee SE, Chang J, et al. Effect site concentrations of propofol for dental treatment under deep sedation in intellectually disabled patients. J Korean Dent Soc Anesthesiol. 2014; 14:167–172.
Article9. Wang YC, Lin IH, Huang CH, Fan SZ. Dental anesthesia for patients with special needs. Acta Anaesthesiol Taiwan. 2012; 50:122–125. PMID: 23026171.
Article10. Shin B, Yoo S, Kim J, Kim S, Kim J. A survey of dental treatment under general anesthesia in a korean university hospital pediatric dental clinic. J Dent Anesth Pain Med. 2016; 16:203–208. PMID: 28884154.
Article11. Messieha Z. Risks of general anesthesia for the special needs dental patient. Spec Care Dentist. 2009; 29:21–25. PMID: 19152564.
Article12. Morimoto Y, Hayashi M, Yokoe C, Kinugawa T, Iida T, Boku A, et al. Intravenous sedation for dental treatment in patients with intellectual disability-efficacy of nasal airway, pharyngeal suction tube and oxygen tube placement. Biomed Res (Aligarh). 2017; 28:4931–4936.13. Yoshikawa F, Tamaki Y, Okumura H, Miwa Z, Ishikawa M, Shimoyama K, et al. Risk factors with intravenous sedation for patients with disabilities. Anesth Prog. 2013; 60:153–161. PMID: 24423418.
Article14. Vaessen HH, Schouten AN, van der, Knape JT. The feasibility of office-based propofol sedation for dental care in patients with intellectual disability by sedation practitioners. Spec Care Dentist. 2017; 37:93–98. PMID: 27805733.
Article15. Mu J, Jiang T, Xu XB, Yuen VM, Irwin MG. Comparison of target-controlled infusion and manual infusion for propofol anaesthesia in children. Br J Anaesth. 2018; 120:1049–1055. PMID: 29661382.
Article16. Sheahan CG, Mathews DM. Monitoring and delivery of sedation. Br J Anaesth. 2014; 113:ii37–ii47. PMID: 25498581.
Article17. Saricaoglu F, Celebi N, Celik M, Aypar U. The evaluation of propofol dosage for anesthesia induction in children with cerebral palsy with bispectral index (BIS) monitoring. Paediatr Anaesth. 2005; 15:1048–1052. PMID: 16324022.
Article18. Ouchi K, Sugiyama K. Required propofol dose for anesthesia and time to emerge are affected by the use of antiepileptics: prospective cohort study. BMC Anesthesiol. 2015; 15:34. PMID: 25788855.
Article19. So E, Kim HJ, Karm MH, Seo KS, Chang J, Lee JH. A retrospective analysis of outpatient anesthesia management for dental treatment of patients with severe Alzheimer's disease. J Dent Anesth Pain Med. 2017; 17:271–280. PMID: 29349349.
Article20. Patsalos PN, Fröscher W, Pisani F, van Rijn CM. The importance of drug interactions in epilepsy therapy. Epilepsia. 2002; 43:365–385. PMID: 11952767.
Article21. Johansen JW. Update on bispectral index monitoring. Best Pract Res Clin Anaesthesiol. 2006; 20:81–99. PMID: 16634416.
Article22. Funder KS, Steinmetz J, Rasmussen LS. Anaesthesia for the patient with dementia undergoing outpatient surgery. Curr Opin Anaesthesiol. 2009; 22:712–717. PMID: 19734784.
Article23. Alcorn S, Foo I. Perioperative management of patients with dementia. BJA Educ. 2017; 17:94–98.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect Site Concentrations of Propofol for Dental Treatment under Deep Sedation in Intellectually Disabled Patients
- Use of ADMSâ„¢ during sedation for dental treatment of an intellectually disabled patient: a case report
- Sedation for Implant Surgery using Propofol and Remifentanil in Severe Dental Phobia Patient: A Case Report
- Target Controlled Conscious Sedation with Propofol and Remifentanil for the Extraction of Impacted Wisdom Teeth
- Monitored anesthesia care for great saphenous vein stripping surgery with target controlled infusion of propofol and remifentanil: a prospective study