Korean J Gastroenterol.
2019 Aug;74(2):110-114. 10.4166/kjg.2019.74.2.110.
Early Phase of Achalasia Manifested as an Esophageal Subepithelial Tumor
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Presbyterian Medical Center, Jeonju, Korea. rocephine@naver.com
- 2Department of General Surgery, Presbyterian Medical Center, Jeonju, Korea.
- 3Department of Pathology, Presbyterian Medical Center, Jeonju, Korea.
- KMID: 2455774
- DOI: http://doi.org/10.4166/kjg.2019.74.2.110
Abstract
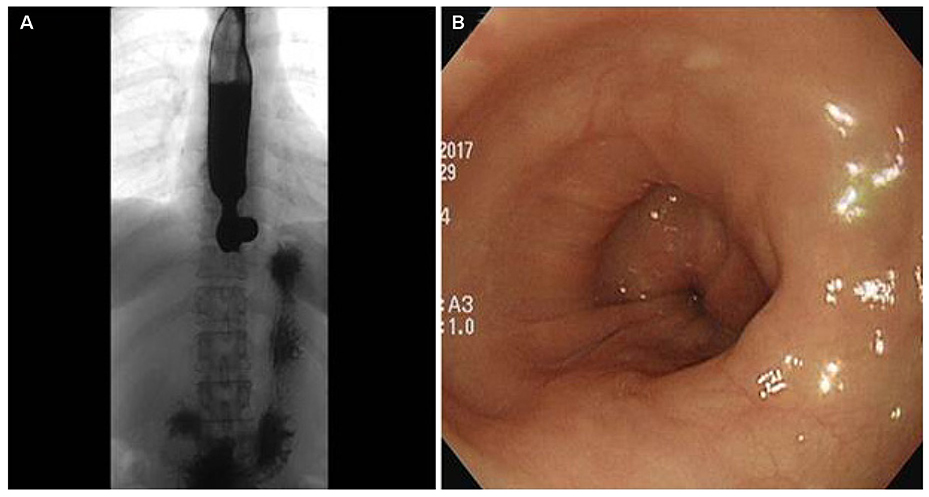
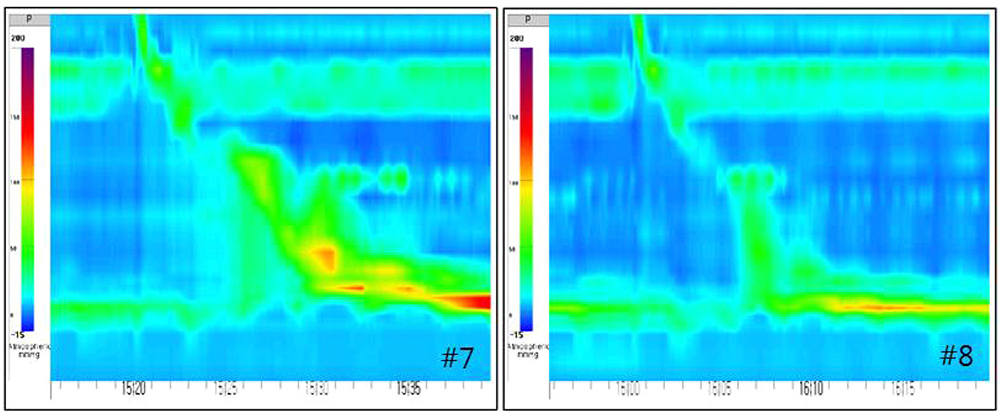
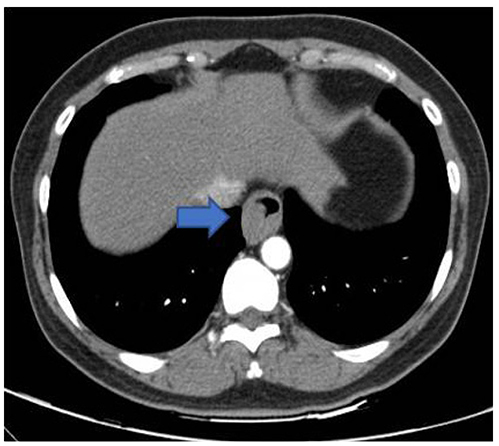
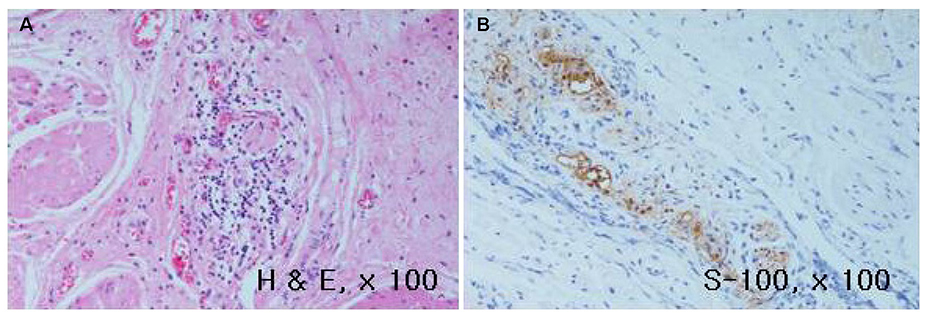
- The Chicago classification (CC) defines an esophagogastric junction outflow obstruction (EGJOO) as the presence of several instances of intact or weak peristalsis, elevated median integrated relaxation pressure above 15 mmHg, and a discrepancy from the criteria of achalasia. The revised CC addresses the potential etiology of EGJOO, including the early forms of achalasia, mechanical obstruction, esophageal wall stiffness, or manifestation of hiatal hernia. A 58-year-old woman visited the Presbyterian Medical Center with swallowing difficulty. The patient underwent a high resolution manometry (HRM) examination and was diagnosed with EGJOO. Chest CT was performed to exclude a mechanical obstruction as a cause, and CT revealed a subepithelial tumor (SET) at the upper part of the esophagogastric junction. Therefore, laparoscopic surgery was performed and eccentric muscular hypertrophy of the distal esophagus was observed. Longitudinal myotomy and Dor fundoplication were also performed. The histology findings of the surgical specimens were consistent with achalasia. This paper reports a case of early achalasia that was finally diagnosed by the histology findings, but was initially diagnosed as EGJOO using HRM and misdiagnosed as SET in the image study.
MeSH Terms
Figure
Reference
-
1. Ortiz V, García-Campos M, Sáez-González E, delPozo P, Garrigues V. A concise review of opioid-induced esophageal dysfunction: is this a new clinical entity? Dis Esophagus. 2018; 31:1–6.
Article2. Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015; 27:160–174.
Article3. Scherer JR, Kwiatek MA, Soper NJ, Pandolfino JE, Kahrilas PJ. Functional esophagogastric junction obstruction with intact peristalsis: a heterogeneous syndrome sometimes akin to achalasia. J Gastrointest Surg. 2009; 13:2219–2225.
Article4. Shin IS, Min YW, Rhee PL. Esophagogastric junction outflow obstruction transformed to type II achalasia. J Neurogastroenterol Motil. 2016; 22:344–345.
Article5. Pandolfino JE, Gawron AJ. Achalasia: a systematic review. JAMA. 2015; 313:1841–1852.6. DeLay K, Austin GL, Menard-Katcher P. Anatomic abnormalities are common potential explanations of manometric esophagogastric junction outflow obstruction. Neurogastroenterol Motil. 2016; 28:1166–1171.
Article7. Hirano I, Tatum RP, Shi G, Sang Q, Joehl RJ, Kahrilas PJ. Manometric heterogeneity in patients with idiopathic achalasia. Gastroenterology. 2001; 120:789–798.
Article8. Sodikoff JB, Lo AA, Shetuni BB, Kahrilas PJ, Yang GY, Pandolfino JE. Histopathologic patterns among achalasia subtypes. Neurogastroenterol Motil. 2016; 28:139–145.
Article9. Goldblum JR, Whyte RI, Orringer MB, Appelman HD. Achalasia. A morphologic study of 42 resected specimens. Am J Surg Pathol. 1994; 18:327–337.10. Mittal RK, Kassab G, Puckett JL, Liu J. Hypertrophy of the muscularis propria of the lower esophageal sphincter and the body of the esophagus in patients with primary motility disorders of the esophagus. Am J Gastroenterol. 2003; 98:1705–1712.
Article11. Pérez-Fernández MT, Santander C, Marinero A, Burgos-Santamaría D, Chavarría-Herbozo C. Characterization and follow-up of esophagogastric junction outflow obstruction detected by high resolution manometry. Neurogastroenterol Motil. 2016; 28:116–126.
Article