J Korean Orthop Assoc.
2019 Aug;54(4):366-371. 10.4055/jkoa.2019.54.4.366.
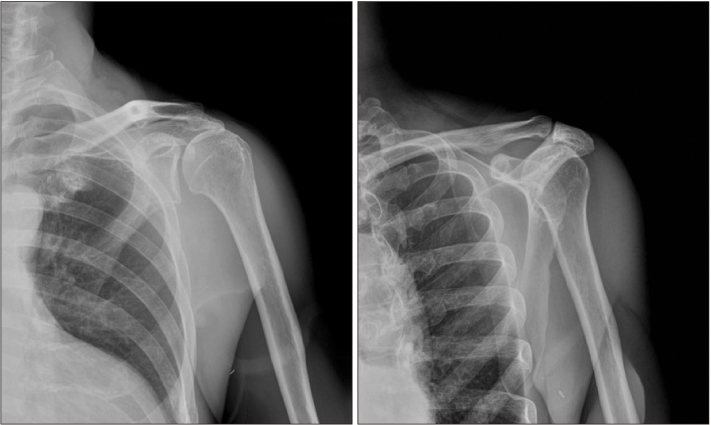
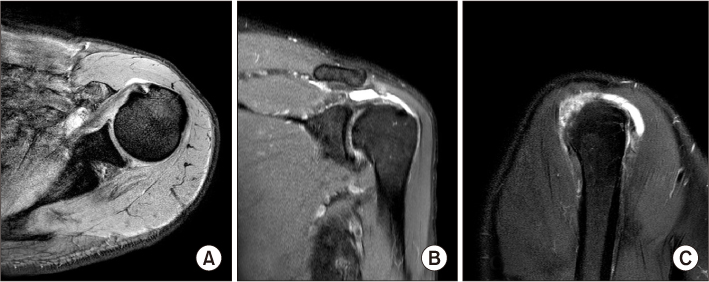
Hemarthrosis Occurred after Arthroscopic Rotator Cuff Repair in a Chronic Renal Failure Patient with a Stenosis in an Ipsilateral Arteriovenous Fistula
- Affiliations
-
- 1Department of Orthopaedic Surgery, St. Carollo Hospital, Suncheon, Korea. abeli@naver.com
- KMID: 2455506
- DOI: http://doi.org/10.4055/jkoa.2019.54.4.366
Abstract
- Hemarthrosis occurring after arthroscopic surgery for lesions of the shoulder joint is a very rare complication that can develop due to an injury to the blood vessels when an anterior portal is formed. This is a complication that rarely develops in patients who are taking antithrombotic drugs or who do not have associated diseases, such as thrombocytopenia. We report a case of hemarthrosis that occurred after performing arthroscopic surgery to repair a rotator cuff tear in a patient with a stenosis in an arteriovenous fistula for hemodialysis in the ipsilateral upper arm.
Keyword
MeSH Terms
Figure
Reference
-
1. Lo IK, Lind CC, Burkhart SS. Glenohumeral arthroscopy portals established using an outside-in technique: neurovascular anatomy at risk. Arthroscopy. 2004; 20:596–602.
Article2. Curtis AS, Snyder SJ, Del Pizzo W, Friedman MJ, Ferkel RD, Karzel RP. Complications of shoulder arthroscopy. Arthroscopy. 1992; 8:395.3. Cameron SE. Venous pseudoaneurysm as a complication of shoulder arthroscopy. J Shoulder Elbow Surg. 1996; 5:404–406.
Article4. Godin JA, Mayer SW, Garrigues GE, Mather RC 3rd. Pseudoaneurysm after shoulder arthroscopy. J Shoulder Elbow Surg. 2013; 22:e12–e17.
Article5. Hall HC, Moudgill N, Kahn M, et al. An unusual cause of venous hypertension after dialysis access creation. Ann Vasc Surg. 2011; 25:983.e1–983.e4.
Article6. Neville RF, Abularrage CJ, White PW, Sidawy AN. Venous hypertension associated with arteriovenous hemodialysis access. Semin Vasc Surg. 2004; 17:50–56.
Article7. Small NC. Complications in arthroscopic surgery performed by experienced arthroscopists. Arthroscopy. 1988; 4:215–221.
Article8. Tsujii A, Tanaka Y, Yonetani Y, Shiozaki Y, Tomiyama Y, Horibe S. Knee hemarthrosis after arthroscopic surgery in an athlete with low factor XIII activity. Sports Med Arthrosc Rehabil Ther Technol. 2012; 4:35.
Article9. Im JH, Huh SW, Park MK, Lee JY. Volar loking plate fixation for distal radius fractures in hemodialysis patients. J Korean Soc Surg Hand. 2015; 20:96–103.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Revisional Rotator Cuff Repair
- New Retear Pattern after Rotator Cuff Repair at Previous Intact Portion of Rotator Cuff
- Surgical Options for Failed Rotator Cuff Repair, except Arthroplasty: Review of Current Methods
- Various Regimens for the Functional Recovery after Arthroscopic Shoulder Surgery
- Arthroscopic Bony Procedure During of Rotator Cuff Repair: Acromioplasty, Distal Clavicle Resection, Footprint Preparation and Coracoplasty