Korean J Ophthalmol.
2019 Aug;33(4):371-378. 10.3341/kjo.2019.0027.
Fluid Dynamics of Small Diameter Tubes Used in Membrane-tube Type Glaucoma Shunt Devices
- Affiliations
-
- 1Department of Ophthalmology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Department of Ophthalmology, Myung-Gok Eye Research Institute, Kim's Eye Hospital, Konyang University College of Medicine, Seoul, Korea. brainh@kimeye.com
- KMID: 2454779
- DOI: http://doi.org/10.3341/kjo.2019.0027
Abstract
- PURPOSE
To investigate the outflow characteristics of silicone tubes with intraluminal stents used in membrane-tube (MT) type glaucoma shunt devices.
METHODS
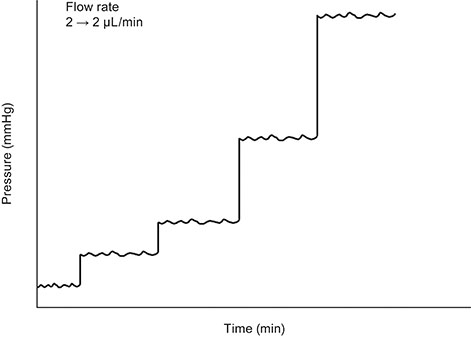
The silicone tubes used in MicroMT (internal diameter of 100 µm with a 7-0 nylon intraluminal stent) and Finetube MT (internal diameter of 200 µm with a 5-0 nylon intraluminal stent) were connected to a syringe-pump that delivered a continuous flow of distilled water at flow rates of 2, 5, 10, and 25 µL/min. The pressures and resistances of tubes were measured at a steady flow rate with full-length, half-length, and absence of intraluminal stents.
RESULTS
The mean outflow resistance of the two types of tubes ranged from 3.0 ± 1.9 to 3.8 ± 1.7 mmHg/µL/min with a full-length intraluminal stent, 1.8 ± 1.1 to 2.2 ± 1.1 mmHg/µL/min with a half-length intraluminal stent, and 0.1 ± 0.0 to 0.2 ± 0.0 mmHg/µL/min without an intraluminal stent. Theoretically, for a physiologic state with a flow rate of 2 µL/min and episcleral venous pressure of 6 mmHg, the mean pressures of tubes were expected to be 13.2 ± 3.0, 10.5 ± 2.4, and 6.4 ± 0.2 mmHg in MicroMT with full-length, half-length, and absence of intraluminal stents, respectively, and 12.5 ± 3.9, 9.6 ± 2.4, and 6.2 ± 0.2 mmHg in Finetube MT with full-length, half-length, and absence of intraluminal stents, respectively. The pressure variance also decreased with intraluminal stent retraction (p < 0.01).
CONCLUSIONS
The small diameter tubes of 100 and 200 µm internal diameters, with 7-0 and 5-0 nylon intraluminal stents, respectively, used in the MT-type glaucoma shunt device showed safe and effective outflow characteristics.
MeSH Terms
Figure
Reference
-
1. Barton K, Feuer WJ, Budenz DL, et al. Three-year treatment outcomes in the Ahmed Baerveldt comparison study. Ophthalmology. 2014; 121:1547–1557.
Article2. Bailey AK, Sarkisian SR Jr. Complications of tube implants and their management. Curr Opin Ophthalmol. 2014; 25:148–153.
Article3. Trible JR, Brown DB. Occlusive ligature and standardized fenestration of a Baerveldt tube with and without antimetabolites for early postoperative intraocular pressure control. Ophthalmology. 1998; 105:2243–2250.4. Sherwood MB, Smith MF. Prevention of early hypotony associated with Molteno implants by a new occluding stent technique. Ophthalmology. 1993; 100:85–90.
Article5. Tong L, Frazao K, LaBree L, Varma R. Intraocular pressure control and complications with two-stage insertion of the Baerveldt implant. Ophthalmology. 2003; 110:353–358.
Article6. Kee C. Prevention of early postoperative hypotony by partial ligation of silicone tube in Ahmed glaucoma valve implantation. J Glaucoma. 2001; 10:466–469.
Article7. Lee JJ, Park KH, Kim DM, Kim TW. Clinical outcomes of Ahmed glaucoma valve implantation using tube ligation and removable external stents. Korean J Ophthalmol. 2009; 23:86–92.
Article8. Ahn BH, Hwang YH, Han JC. Novel membrane-tube type glaucoma shunt device for glaucoma surgery. Clin Exp Ophthalmol. 2016; 44:776–782.
Article9. Han JC, Hwang YH, Ahn BH. Membrane-tube-type glaucoma shunt device for refractory glaucoma surgery. Graefes Arch Clin Exp Ophthalmol. 2017; 255:163–169.
Article10. Kim C, Kim Y, Choi S, et al. Clinical experience of e-PTFE membrane implant surgery for refractory glaucoma. Br J Ophthalmol. 2003; 87:63–70.
Article11. Choi YJ, Kim CS, Ahn BH. A comparison of the clinical effect between e-PTFE membrane-tube implant and Ahmed glaucoma valve implant for the treatment of refractory glaucoma. Korean J Ophthalmol. 2003; 17:106–113.
Article12. Kim MK, Hwang YH, Ahn BH. Implantation of a modified baerveldt glaucoma implant with a smaller tube and intraluminal stent. Korean J Ophthalmol. 2017; 31:90–91.
Article13. Bae HB, Kim CS, Ahn BH. A membranous drainage implant in glaucoma filtering surgery: animal trial. Korean J Ophthalmol. 1988; 2:49–56.
Article14. Kim DW, Hwang YH, Ahn BH, et al. Safety and efficacy of a membrane-tube-type glaucoma shunt device: an animal trial. Curr Eye Res. 2017; 42:890–896.
Article15. Sohn SW, Noh MD, Lee JH, et al. Performance of and pressure elevation formed by small-diameter microtubes used in constant-flow sets. Korean J Ophthalmol. 2016; 30:225–233.
Article16. Francis BA, Cortes A, Chen J, Alvarado JA. Characteristics of glaucoma drainage implants during dynamic and steady-state flow conditions. Ophthalmology. 1998; 105:1708–1714.
Article17. Rietveld E, van der Veen AJ AJ. Postoperative pressure regulation in glaucoma shunt surgery: focal tube constriction is not the answer. J Glaucoma. 2004; 13:216–220.18. Hoare Nairne JE JE, Sherwood D, Jacob JS, Rich WJ. Single stage insertion of the Molteno tube for glaucoma and modifications to reduce postoperative hypotony. Br J Ophthalmol. 1988; 72:846–851.19. Sheybani A, Reitsamer H, Ahmed II. Fluid dynamics of a novel micro-fistula implant for the surgical treatment of glaucoma. Invest Ophthalmol Vis Sci. 2015; 56:4789–4795.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anterior Chamber Tube Shunt to a Surgical Membrane
- Intermediate-term Result of e-PTFE Membrane Implant Surgery for Refractory Glaucomas
- Development of the Unsteady Capillary Tube Viscometer and Viscosity Measurement of Blood Analogue Fluid
- Anterior chamber tube shunt to an encircling band in the treatment of glaucoma
- Anterior Chamber Tube Shunt to an Encircling Band in the Treatment of Glaucoma