Intest Res.
2019 Jul;17(3):357-364. 10.5217/ir.2018.00107.
Risk of surgery in patients with stricturing type of Crohn's disease at the initial diagnosis: a single center experience
- Affiliations
-
- 1Department of Medicine and Clinical Science, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan. ymaehata@intmed2.med.kyushu-u.ac.jp
- 2Maehata Clinic, Kagoshima, Japan.
- 3Department of Surgery and Oncology, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan.
- 4Department of Endoscopic Diagnostics and Therapeutics, Saga University Hospital, Saga, Japan.
- KMID: 2454744
- DOI: http://doi.org/10.5217/ir.2018.00107
Abstract
- BACKGROUND/AIMS
It remains uncertain which patients with stricturing-type Crohn's disease (CD) require early small bowel surgery after the initial diagnosis. We aimed to clarify clinical characteristics associated with the intervention in such condition of CD.
METHODS
We retrospectively evaluated the clinical course of 53 patients with CD and small bowel strictures who were initially treated with medications after the initial diagnosis. We investigated possible associations between small bowel surgery and the following: clinical factors and radiologic findings at initial diagnosis and the types of medications administered during follow-up.
RESULTS
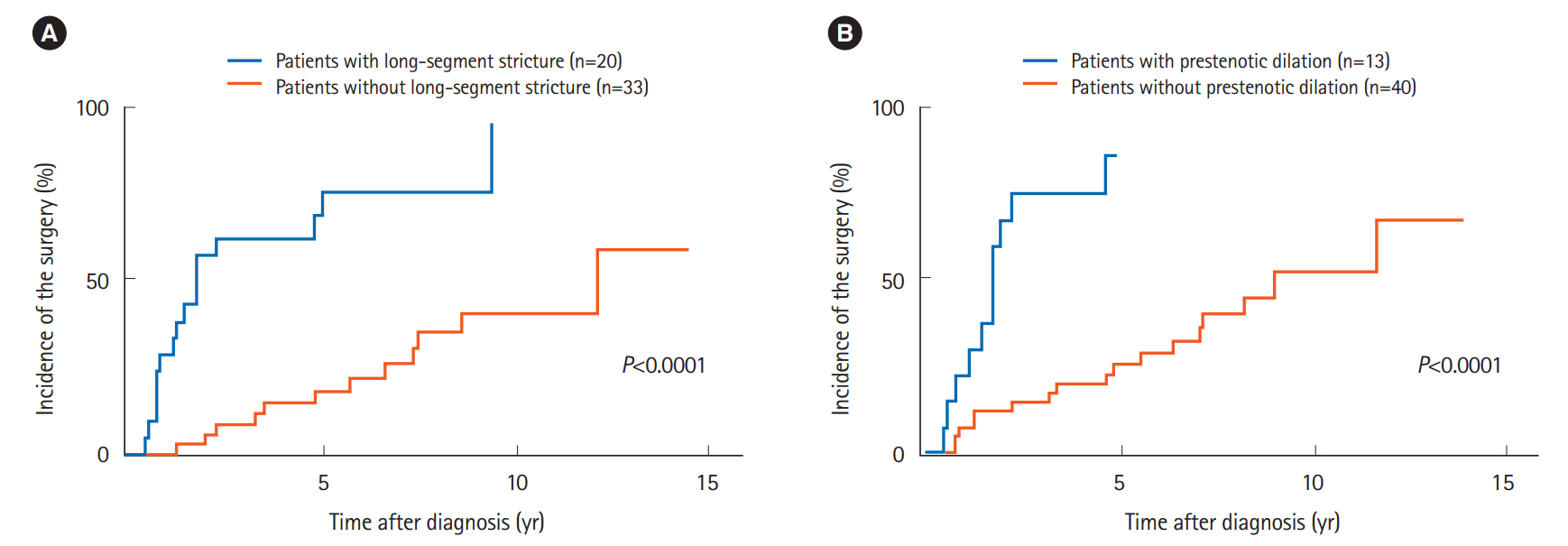
Twenty-eight patients (53%) required small bowel resection during a median follow-up period of 5.0 years (range, 0.5-14.3 years). The cumulative incidence rates of small bowel surgery at 2, 5, and 10 years were 26.4%, 41.0%, and 63.2%, respectively. Univariate analysis indicated that obstructive symptoms (P=0.036), long-segment stricture (P<0.0001), and prestenotic dilation (P<0.0001) on radiography were associated with small bowel surgery, and immunomodulatory (P=0.037) and biological therapy (P=0.008) were significant factors during follow-up. Multivariate analysis revealed that long-segment stricture (hazard ratio [HR], 4.25; 95% confidence interval [CI], 1.78-10.53; P=0.001) and prestenotic dilation (HR, 3.41; 95% CI, 1.24-9.62; P=0.018) on radiography showed a positive correlation with small bowel surgery, and biological therapy (HR, 0.40; 95% CI, 0.15-0.99; P=0.048) showed a negative correlation.
CONCLUSIONS
CD patients with long-segment stricture and prestenotic dilation on radiography seem to be at a higher risk of needing small bowel surgery. For such patients, early surgical intervention might be appropriate, even at initial diagnosis.
MeSH Terms
Figure
Reference
-
1. Baumgart DC, Sandborn WJ. Crohn’s disease. Lancet. 2012; 380:1590–1605.
Article2. Louis E, Collard A, Oger AF, Degroote E, Aboul Nasr El Yafi FA, Belaiche J. Behaviour of Crohn’s disease according to the Vienna classification: changing pattern over the course of the disease. Gut. 2001; 49:777–782.
Article3. Cleynen I, González JR, Figueroa C, et al. Genetic factors conferring an increased susceptibility to develop Crohn’s disease also influence disease phenotype: results from the IBDchip European Project. Gut. 2013; 62:1556–1565.
Article4. Yano Y, Matsui T, Hirai F, et al. Cancer risk in Japanese Crohn’s disease patients: investigation of the standardized incidence ratio. J Gastroenterol Hepatol. 2013; 28:1300–1305.
Article5. Cosnes J. Crohn’s disease phenotype, prognosis, and long-term complications: what to expect? Acta Gastroenterol Belg. 2008; 71:303–307.6. Aloi M, Viola F, D’Arcangelo G, et al. Disease course and efficacy of medical therapy in stricturing paediatric Crohn’s disease. Dig Liver Dis. 2013; 45:464–468.
Article7. Hanauer SB, Feagan BG, Lichtenstein GR, et al. Maintenance infliximab for Crohn’s disease: the ACCENT I randomised trial. Lancet. 2002; 359:1541–1549.
Article8. Hanauer SB, Sandborn WJ, Rutgeerts P, et al. Human anti-tumor necrosis factor monoclonal antibody (adalimumab) in Crohn’s disease: the CLASSIC-I trial. Gastroenterology. 2006; 130:323–333.
Article9. Matsumoto T, Iida M, Motoya S, et al. Therapeutic efficacy of infliximab on patients with short duration of Crohn’s disease: a Japanese multicenter survey. Dis Colon Rectum. 2008; 51:916–923.
Article10. Colombel JF, Sandborn WJ, Reinisch W, et al. Infliximab, azathioprine, or combination therapy for Crohn’s disease. N Engl J Med. 2010; 362:1383–1395.
Article11. Regueiro M, Kip KE, Baidoo L, Swoger JM, Schraut W. Postoperative therapy with infliximab prevents long-term Crohn’s disease recurrence. Clin Gastroenterol Hepatol. 2014; 12:1494–1502.
Article12. De Cruz P, Kamm MA, Hamilton AL, et al. Crohn’s disease management after intestinal resection: a randomised trial. Lancet. 2015; 385:1406–1417.
Article13. Regueiro M, Feagan BG, Zou B, et al. Infliximab reduces endoscopic, but not clinical, recurrence of Crohn’s disease after ileocolonic resection. Gastroenterology. 2016; 150:1568–1578.14. Samimi R, Flasar MH, Kavic S, Tracy K, Cross RK. Outcome of medical treatment of stricturing and penetrating Crohn’s disease: a retrospective study. Inflamm Bowel Dis. 2010; 16:1187–1194.
Article15. Yao T, Matsui T, Hiwatashi N. Crohn’s disease in Japan: diagnostic criteria and epidemiology. Dis Colon Rectum. 2000; 43(10 Suppl):S85–S93.16. Best WR, Becktel JM, Singleton JW, Kern F Jr. Development of a Crohn’s disease activity index. National Cooperative Crohn’s Disease Study. Gastroenterology. 1976; 70:439–444.17. Matsumoto T, Esaki M, Kurahara K, et al. Double-contrast barium enteroclysis as a patency tool for nonsteroidal anti-inflammatory drug-induced enteropathy. Dig Dis Sci. 2011; 56:3247–3253.
Article18. Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006; 55:749–753.
Article19. Rieder F, Zimmermann EM, Remzi FH, Sandborn WJ. Crohn’s disease complicated by strictures: a systematic review. Gut. 2013; 62:1072–1084.
Article20. Hirai F, Beppu T, Sou S, Seki T, Yao K, Matsui T. Endoscopic balloon dilatation using double-balloon endoscopy is a useful and safe treatment for small intestinal strictures in Crohn’s disease. Dig Endosc. 2010; 22:200–204.
Article21. Lakatos PL, Golovics PA, David G, et al. Has there been a change in the natural history of Crohn’s disease? Surgical rates and medical management in a population-based inception cohort from Western Hungary between 1977-2009. Am J Gastroenterol. 2012; 107:579–588.
Article22. Fu YT, Hong T, Round A, Bressler B. Impact of medical therapy on patients with Crohn’s disease requiring surgical resection. World J Gastroenterol. 2014; 20:11808–11814.
Article23. Chhaya V, Pollok RC, Cecil E, et al. Impact of early thiopurines on surgery in 2770 children and young people diagnosed with inflammatory bowel disease: a national population-based study. Aliment Pharmacol Ther. 2015; 42:990–999.
Article24. Cosnes J, Bourrier A, Laharie D, et al. Early administration of azathioprine vs conventional management of Crohn’s disease: a randomized controlled trial. Gastroenterology. 2013; 145:758–765.
Article25. Chatu S, Subramanian V, Saxena S, Pollok RC. The role of thiopurines in reducing the need for surgical resection in Crohn’s disease: a systematic review and meta-analysis. Am J Gastroenterol. 2014; 109:23–34.
Article26. Feagan BG, Panaccione R, Sandborn WJ, et al. Effects of adalimumab therapy on incidence of hospitalization and surgery in Crohn’s disease: results from the CHARM study. Gastroenterology. 2008; 135:1493–1499.
Article27. Schnitzler F, Fidder H, Ferrante M, et al. Long-term outcome of treatment with infliximab in 614 patients with Crohn’s disease: results from a single-centre cohort. Gut. 2009; 58:492–500.
Article28. Rungoe C, Langholz E, Andersson M, et al. Changes in medical treatment and surgery rates in inflammatory bowel disease: a nationwide cohort study 1979-2011. Gut. 2014; 63:1607–1616.
Article29. Lichtenstein GR, Olson A, Travers S, et al. Factors associated with the development of intestinal strictures or obstructions in patients with Crohn’s disease. Am J Gastroenterol. 2006; 101:1030–1038.
Article30. Pelletier AL, Kalisazan B, Wienckiewicz J, Bouarioua N, Soulé JC. Infliximab treatment for symptomatic Crohn’s disease strictures. Aliment Pharmacol Ther. 2009; 29:279–285.
Article31. Condino G, Calabrese E, Zorzi F, et al. Anti-TNF-alpha treatments and obstructive symptoms in Crohn’s disease: a prospective study. Dig Liver Dis. 2013; 45:258–262.
Article32. Gomollón F, Dignass A, Annese V, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016. Part 1: diagnosis and medical management. J Crohns Colitis. 2017; 11:3–25.
Article33. Matsuoka K, Kobayashi T, Ueno F, et al. Evidence-based clinical practice guidelines for inflammatory bowel disease. J Gastroenterol. 2018; 53:305–353.
Article34. Otterson MF, Lundeen SJ, Spinelli KS, et al. Radiographic underestimation of small bowel stricturing Crohn’s disease: a comparison with surgical findings. Surgery. 2004; 136:854–860.
Article35. Angriman I, Scarpa M, Ruffolo C, et al. Double contrast small-bowel radiography in the preoperative assessment of Crohn’s disease: is it still useful? Surg Today. 2008; 38:700–704.
Article36. Greenup AJ, Bressler B, Rosenfeld G. Medical imaging in small bowel Crohn’s disease-computer tomography enterography, magnetic resonance enterography, and ultrasound: “Which one is the best for what?”. Inflamm Bowel Dis. 2016; 22:1246–1261.
Article37. Takenaka K, Ohtsuka K, Kitazume Y, et al. Comparison of magnetic resonance and balloon enteroscopic examination of the small intestine in patients with Crohn’s disease. Gastroenterology. 2014; 147:334–342.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rates of Early Surgery and Associated Risk Factors in Crohn's Disease
- Postoperative Complications and Recurrence in Patients with Crohn's Disease
- Risk Factors for Repeat Abdominal Surgery in Korean Patients with Crohn's Disease: A Multi-Center Study of a Korean Inflammatory Bowel Disease Study Group
- Crohn's Disease with Intraabdominal Abscess as the Initial Diagnosis
- Efficacy of Thiopurines in Biologic-Naive Japanese Patients With Crohn's Disease: A Single-Center Experience