Cancer Res Treat.
2019 Jul;51(3):1156-1166. 10.4143/crt.2018.472.
High-Dose Thoracic Re-irradiation of Lung Cancer Using Highly Conformal Radiotherapy Is Effective with Acceptable Toxicity
- Affiliations
-
- 1Department of Radiation Oncology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. yeonkim7@catholic.ac.kr
- 2Division of Medical Oncology, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2454307
- DOI: http://doi.org/10.4143/crt.2018.472
Abstract
- PURPOSE
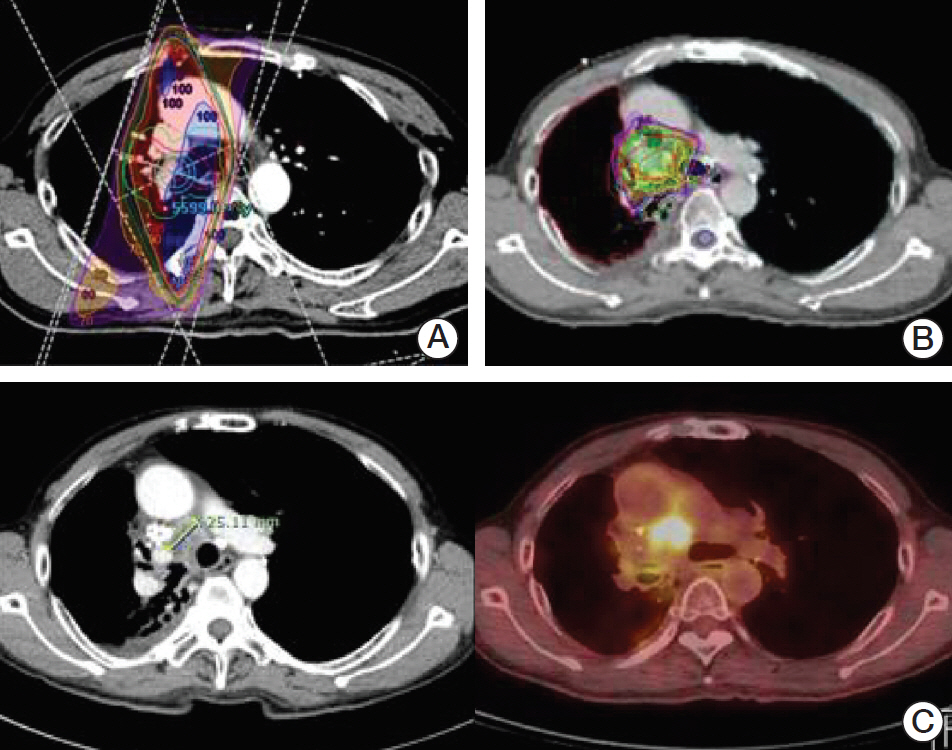
Thoracic re-irradiation (re-RT) of lung cancer has been challenged by the tolerance doses of normal tissues. We retrospectively analyzed local control, overall survival (OS) and toxicity after thoracic re-RT using highly conformal radiotherapy, such as intensity modulated radiotherapy and stereotactic body radiotherapy.
MATERIALS AND METHODS
Thirty-one patients who received high-dose thoracic re-RT were analyzed. Doses were recalculated to determine biologically equivalent doses. The median interval to re-RT was 15.1 months (range, 4.4 to 56.3 months), the median initial dose was 79.2 Gyâ‚â‚€ (range, 51.75 to 150 Gyâ‚â‚€), and the median re-RT dose was 68.8 Gyâ‚â‚€ (range, 43.2 to 132 Gyâ‚â‚€).
RESULTS
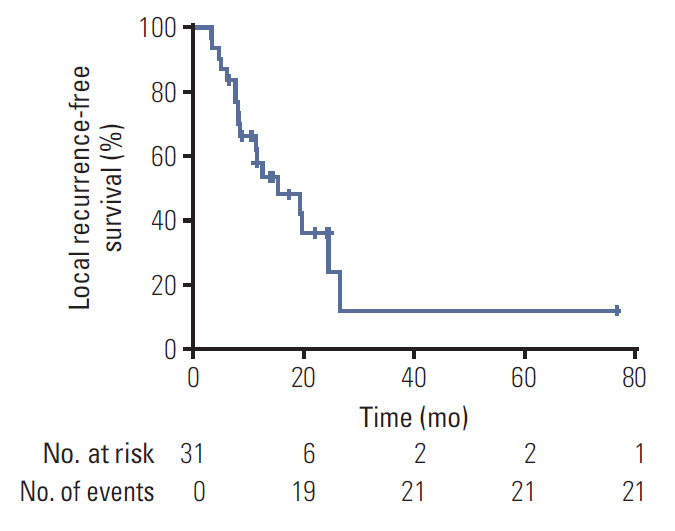
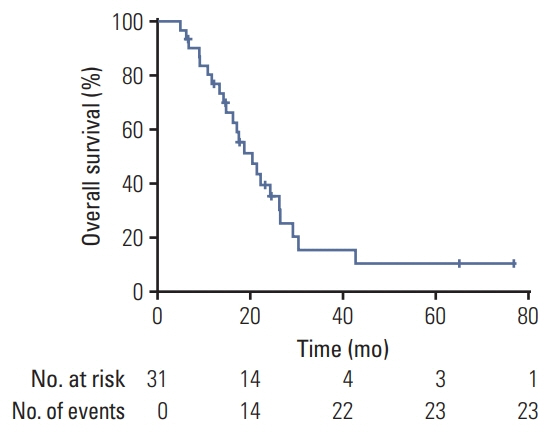
Eighteen (58.1%) and eleven (35.5%) patients showed loco-regional recurrence and distant metastasis, respectively, after 17.4 months of median follow-up. The 1-year and 2-year local control rates were 60.2% and 43.7%, respectively. The median loco-regional recurrence-free-survival (LRFS) was 15.4 months, and the median OS was 20.4 months. The cumulative and re-RT biologically equivalent dose for α/β=10 (BEDâ‚â‚€) doses were the most significant prognostic factors. Cumulative BEDâ‚₀≥145 Gyâ‚â‚€ and re-RT BEDâ‚₀≥68.7 Gyâ‚â‚€ were significantly associated with longer OS (p=0.029 and p=0.012, respectively) and LRFS (p=0.003 and p=0.000, respectively). The most frequent acute toxicity was grade 1-2 pulmonary toxicity (41.9%). No acute grade 3 or higher toxicities occurred.
CONCLUSION
Our results show that high-dose thoracic re-RT of lung cancer can be safely delivered using highly conformal radiotherapy with favorable survival and acceptable toxicity. An optimal strategy to select patients who would benefit from re-RT is crucial in extending the indications and improving the efficacy with a sufficiently high dose.
MeSH Terms
Figure
Reference
-
References
1. National Cancer Information Center. Annual report of cancer statistics in Korea in 2012-2015 [Internet]. Goyang: National Cancer Information Center;2016. [cited 2018 Mar 10]. Available from: http://www.cancer.go.kr/.2. Park JY, Jang SH. Epidemiology of lung cancer in Korea: recent trends. Tuberc Respir Dis. 2016; 79:58–69.
Article3. Warde P, Payne D. Does thoracic irradiation improve survival and local control in limited-stage small-cell carcinoma of the lung? A meta-analysis. J Clin Oncol. 1992; 10:890–5.
Article4. Oh IJ, Ahn SJ. Multidisciplinary team approach for the management of patients with locally advanced non-small cell lung cancer: searching the evidence to guide the decision. Radiat Oncol J. 2017; 35:16–24.
Article5. Auperin A, Le Pechoux C, Rolland E, Curran WJ, Furuse K, Fournel P, et al. Meta-analysis of concomitant versus sequential radiochemotherapy in locally advanced non-small-cell lung cancer. J Clin Oncol. 2010; 28:2181–90.6. Turrisi AT 3rd, Kim K, Blum R, Sause WT, Livingston RB, Komaki R, et al. Twice-daily compared with once-daily thoracic radiotherapy in limited small-cell lung cancer treated concurrently with cisplatin and etoposide. N Engl J Med. 1999; 340:265–71.
Article7. Jeremic B, Videtic GM. Chest reirradiation with external beam radiotherapy for locally recurrent non-small-cell lung cancer: a review. Int J Radiat Oncol Biol Phys. 2011; 80:969–77.8. De Ruysscher D, Faivre-Finn C, Le Pechoux C, Peeters S, Belderbos J. High-dose re-irradiation following radical radiotherapy for non-small-cell lung cancer. Lancet Oncol. 2014; 15:e620–4.
Article9. Vassil AD, Videtic GM, Stephans KL. Re-irradiation in lung cancer. J Radiat Oncol. 2015; 4:129–39.
Article10. Wu KL, Jiang GL, Qian H, Wang LJ, Yang HJ, Fu XL, et al. Three-dimensional conformal radiotherapy for locoregionally recurrent lung carcinoma after external beam irradiation: a prospective phase I-II clinical trial. Int J Radiat Oncol Biol Phys. 2003; 57:1345–50.
Article11. Ohguri T, Imada H, Yahara K, Moon SD, Yamaguchi S, Yatera K, et al. Re-irradiation plus regional hyperthermia for recurrent non-small cell lung cancer: a potential modality for inducing long-term survival in selected patients. Lung Cancer. 2012; 77:140–5.
Article12. Griffioen GH, Dahele M, de Haan PF, van de Ven PM, Slotman BJ, Senan S. High-dose, conventionally fractionated thoracic reirradiation for lung tumors. Lung Cancer. 2014; 83:356–62.
Article13. Reyngold M, Wu AJ, McLane A, Zhang Z, Hsu M, Stein NF, et al. Toxicity and outcomes of thoracic re-irradiation using stereotactic body radiation therapy (SBRT). Radiat Oncol. 2013; 8:99.
Article14. McAvoy SA, Ciura KT, Rineer JM, Allen PK, Liao Z, Chang JY, et al. Feasibility of proton beam therapy for reirradiation of locoregionally recurrent non-small cell lung cancer. Radiother Oncol. 2013; 109:38–44.
Article15. McAvoy S, Ciura K, Wei C, Rineer J, Liao Z, Chang JY, et al. Definitive reirradiation for locoregionally recurrent non-small cell lung cancer with proton beam therapy or intensity modulated radiation therapy: predictors of high-grade toxicity and survival outcomes. Int J Radiat Oncol Biol Phys. 2014; 90:819–27.
Article16. Tada T, Fukuda H, Matsui K, Hirashima T, Hosono M, Takada Y, et al. Non-small-cell lung cancer: reirradiation for locoregional relapse previously treated with radiation therapy. Int J Clin Oncol. 2005; 10:247–50.
Article17. Trakul N, Harris JP, Le QT, Hara WY, Maxim PG, Loo BW Jr, et al. Stereotactic ablative radiotherapy for reirradiation of locally recurrent lung tumors. J Thorac Oncol. 2012; 7:1462–5.
Article18. Sumita K, Harada H, Asakura H, Ogawa H, Onoe T, Murayama S, et al. Re-irradiation for locoregionally recurrent tumors of the thorax: a single-institution, retrospective study. Radiat Oncol. 2016; 11:104.
Article19. Aktan M, Kanyilmaz G, Koc M, Aras S. Thoracic re-irradiation for locally recurrent lung cancer. Asian Pac J Cancer Prev. 2016; 17:5041–5.20. De Bari B, Filippi AR, Mazzola R, Bonomo P, Trovo M, Livi L, et al. Available evidence on re-irradiation with stereotactic ablative radiotherapy following high-dose previous thoracic radiotherapy for lung malignancies. Cancer Treat Rev. 2015; 41:511–8.
Article21. Trovo M, Minatel E, Durofil E, Polesel J, Avanzo M, Baresic T, et al. Stereotactic body radiation therapy for re-irradiation of persistent or recurrent non-small cell lung cancer. Int J Radiat Oncol Biol Phys. 2014; 88:1114–9.
Article22. Peulen H, Karlsson K, Lindberg K, Tullgren O, Baumann P, Lax I, et al. Toxicity after reirradiation of pulmonary tumours with stereotactic body radiotherapy. Radiother Oncol. 2011; 101:260–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Stereotactic Body Radiotherapy for Early Stage Lung Cancer
- Hyperfractionated re-irradiation using a 3-dimensional conformal technique for locally recurrent carcinoma of the nasopharynx; preliminary results
- Dosimetric comparison between modulated arc therapy and static intensity modulated radiotherapy in thoracic esophageal cancer: a single institutional experience
- Development of Conformal Radiotherapy with Respiratory Gate Device
- Evaluation of the hybrid-dynamic conformal arc therapy technique for radiotherapy of lung cancer