Cancer Res Treat.
2019 Jul;51(3):1135-1143. 10.4143/crt.2018.392.
Prognostic Implications of Extranodal Extension in Relation to Colorectal Cancer Location
- Affiliations
-
- 1Department of Surgery, Institute of Innovative Cancer Research, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. jckim@amc.seoul.kr
- 2Department of Pathology, Institute of Innovative Cancer Research, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 3School of Life Science, Kyungpook National University, Daegu, Korea.
- KMID: 2454305
- DOI: http://doi.org/10.4143/crt.2018.392
Abstract
- PURPOSE
Extranodal extension (ENE) is closely associated with the aggressiveness of both colon and rectal cancer. This study evaluated the clinicopathologic significance and prognostic impact of ENE in separate populations of patients with colon and rectal cancers.
MATERIALS AND METHODS
The medical records of 2,346 patients with colorectal cancer (CRC) who underwent curative surgery at our institution between January 2003 and December 2011 were clinically and histologically reviewed.
RESULTS
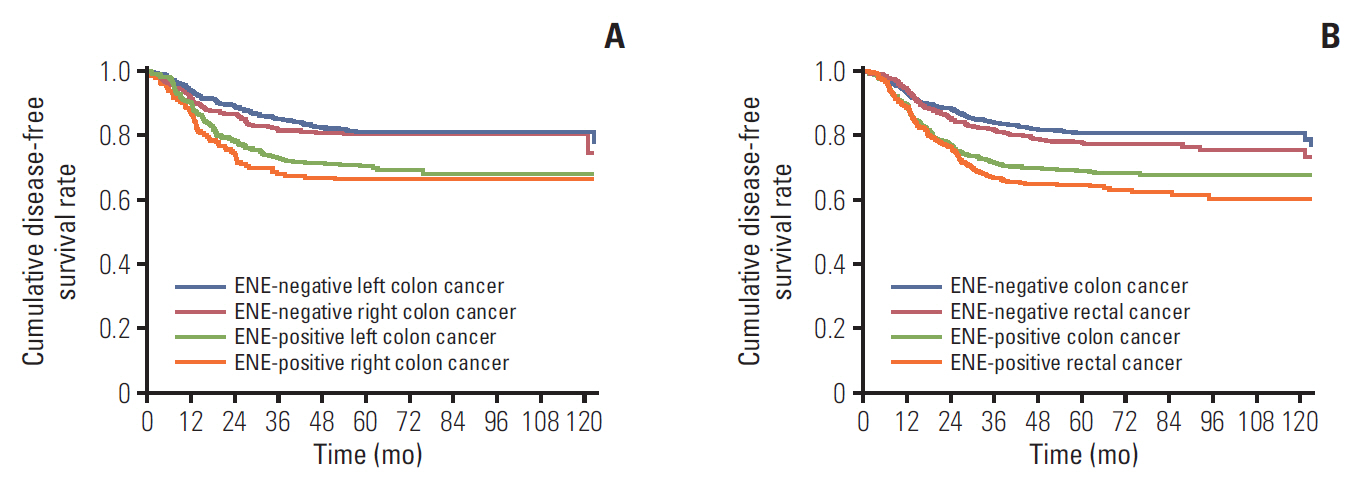
ENE was associated with younger age, advanced tumor stage, lymphovascular invasion (LVI), and perineural invasion (PNI) in both colon and rectal cancer. ENE rates differed significantly in patients with right colon (36.9%), left colon (42.6%), and rectal (48.7%) cancers (right vs. left, p=0.037; left vs. rectum, p=0.009). The 5-year disease-free survival (DFS) rate according to ENE status and primary tumor site differed significantly in patients with ENE-negative colon cancer (80.5%), ENE-negative rectal cancer (77.4%), ENE-positive colon cancer (68.6%), and ENE-positive rectal cancer (64.2%) (p<0.001). Multivariate analysis showed that advanced tumor stage, ENE, LVI, PNI, and absence of adjuvant chemotherapy were independently prognostic of reduced DFS in colon and rectal cancer patients.
CONCLUSION
ENE is closely associated with the aggressiveness of colon and rectal cancers, with its frequency increasing from the right colon to the left colon to the rectum. ENE status is a significant independent predictor of DFS in CRC patients irrespective of tumor location. ENE might be more related with distally located CRC.
MeSH Terms
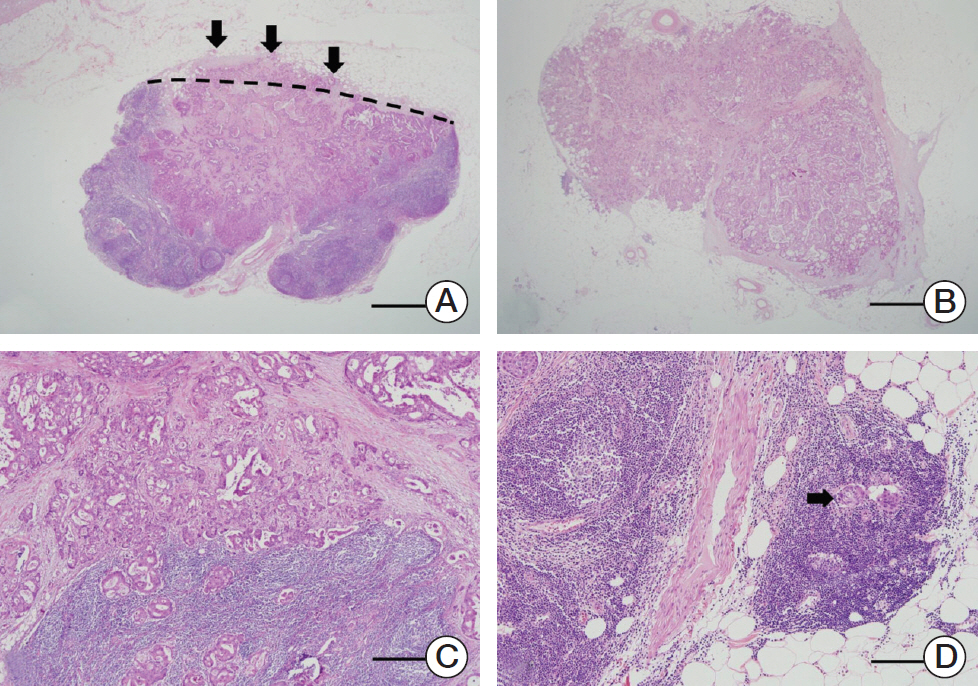
Figure
Reference
-
References
1. Lee IS, Park YS, Ryu MH, Song MJ, Yook JH, Oh ST, et al. Impact of extranodal extension on prognosis in lymph node-positive gastric cancer. Br J Surg. 2014; 101:1576–84.
Article2. Suh S, Pak K, Seok JW, Kim IJ. Prognostic value of extranodal extension in thyroid cancer: a meta-analysis. Yonsei Med J. 2016; 57:1324–8.
Article3. Fajkovic H, Cha EK, Jeldres C, Robinson BD, Rink M, Xylinas E, et al. Extranodal extension is a powerful prognostic factor in bladder cancer patients with lymph node metastasis. Eur Urol. 2013; 64:837–45.
Article4. Nottegar A, Veronese N, Senthil M, Roumen RM, Stubbs B, Choi AH, et al. Extra-nodal extension of sentinel lymph node metastasis is a marker of poor prognosis in breast cancer patients: A systematic review and an exploratory meta-analysis. Eur J Surg Oncol. 2016; 42:919–25.
Article5. Zhang ZL, Yu CP, Liu ZW, Velet L, Li YH, Jiang LJ, et al. The importance of extranodal extension in penile cancer: a meta-analysis. BMC Cancer. 2015; 15:815.
Article6. Lee YC, Wu CT, Kuo SW, Tseng YT, Chang YL. Significance of extranodal extension of regional lymph nodes in surgically resected non-small cell lung cancer. Chest. 2007; 131:993–9.
Article7. van der Velden J, van Lindert AC, Lammes FB, ten Kate FJ, Sie-Go DM, Oosting H, et al. Extracapsular growth of lymph node metastases in squamous cell carcinoma of the vulva. The impact on recurrence and survival. Cancer. 1995; 75:2885–90.
Article8. Luchini C, Nottegar A, Pea A, Solmi M, Stubbs B, Capelli P, et al. Significance of the prognostic stratification of extranodal extension in colorectal cancer. Ann Oncol. 2016; 27:1647.
Article9. Edge SB, Greene FL, Byrd DR, Brookland RK, Waashington MK, Gershenwald JE, et al. AJCC cancer staging manual. 8th ed. New York: Springer;2017.10. Yamauchi M, Lochhead P, Morikawa T, Huttenhower C, Chan AT, Giovannucci E, et al. Colorectal cancer: a tale of two sides or a continuum? Gut. 2012; 61:794–7.11. Tamas K, Walenkamp AM, de Vries EG, van Vugt MA, Beets-Tan RG, van Etten B, et al. Rectal and colon cancer: not just a different anatomic site. Cancer Treat Rev. 2015; 41:671–9.
Article12. Wei EK, Giovannucci E, Wu K, Rosner B, Fuchs CS, Willett WC, et al. Comparison of risk factors for colon and rectal cancer. Int J Cancer. 2004; 108:433–42.
Article13. Huang Q, Yang H. Prognostic impact of extra-nodal extension on colon and rectal cancer should be investigated separately. Ann Oncol. 2016; 27:956–7.
Article14. Iacopetta B. Are there two sides to colorectal cancer? Int J Cancer. 2002; 101:403–8.
Article15. Kim CW, Kim J, Yeom SS, Lee JL, Yoon YS, Park IJ, et al. Extranodal extension status is a powerful prognostic factor in stage III colorectal cancer. Oncotarget. 2017; 8:61393–403.
Article16. Wang B, Yang J, Li S, Lv M, Chen Z, Li E, et al. Tumor location as a novel high risk parameter for stage II colorectal cancers. PLoS One. 2017; 12:e0179910.
Article17. Luchini C, Wood LD, Cheng L, Nottegar A, Stubbs B, Solmi M, et al. Extranodal extension of lymph node metastasis is a marker of poor prognosis in oesophageal cancer: a systematic review with meta-analysis. J Clin Pathol. 2016; 69:956–91.
Article18. Veronese N, Nottegar A, Pea A, Solmi M, Stubbs B, Capelli P, et al. Prognostic impact and implications of extracapsular lymph node involvement in colorectal cancer: a systematic review with meta-analysis. Ann Oncol. 2016; 27:42–8.
Article19. Gervaz P, Bucher P, Morel P. Two colons-two cancers: paradigm shift and clinical implications. J Surg Oncol. 2004; 88:261–6.
Article20. Ghazi S, Lindforss U, Lindberg G, Berg E, Lindblom A, Papadogiannakis N, et al. Analysis of colorectal cancer morphology in relation to sex, age, location, and family history. J Gastroenterol. 2012; 47:619–34.
Article21. Butcher D, Hassanein K, Dudgeon M, Rhodes J, Holmes FF. Female gender is a major determinant of changing subsite distribution of colorectal cancer with age. Cancer. 1985; 56:714–6.
Article22. Ogino S, Goel A. Molecular classification and correlates in colorectal cancer. J Mol Diagn. 2008; 10:13–27.
Article23. Bertario L, Russo A, Sala P, Eboli M, Radice P, Presciuttini S, et al. Survival of patients with hereditary colorectal cancer: comparison of HNPCC and colorectal cancer in FAP patients with sporadic colorectal cancer. Int J Cancer. 1999; 80:183–7.
Article24. Markowitz SD, Bertagnolli MM. Molecular origins of cancer: Molecular basis of colorectal cancer. N Engl J Med. 2009; 361:2449–60.25. Alotaibi AM, Lee JL, Kim J, Lim SB, Yu CS, Kim TW, et al. Prognostic and oncologic significance of perineural invasion in sporadic colorectal cancer. Ann Surg Oncol. 2017; 24:1626–34.
Article26. Lim SB, Yu CS, Jang SJ, Kim TW, Kim JH, Kim JC. Prognostic significance of lymphovascular invasion in sporadic colorectal cancer. Dis Colon Rectum. 2010; 53:377–84.
Article27. Andre T, Boni C, Mounedji-Boudiaf L, Navarro M, Tabernero J, Hickish T, et al. Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med. 2004; 350:2343–51.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- ERRATUM: Prognostic Implications of Extranodal Extension in Relation to Colorectal Cancer Location
- N Stage: Controversies and Recent Issues
- Relation Between p53 Overexpression and Extablished Prognostic Facors in Colorectal Cancer
- Multivariate analysis of prognostic factors in colorectal cancer patients: significance of lymph node metastasis as a prognostic factor in colorectal cancer
- Clinical study for prognostic factors in colorectal cancer